Journal of
eISSN: 2373-4426


Case Report Volume 13 Issue 1
Department of Paediatric Cardiology, Aster Ramesh Hospitals, India
Correspondence: Dr. Murtaza Kamal, Consultant Paediatric Cardiology, Room no: 10, Aster Ramesh Hospitals, Vijayawada, India, Tel +91-9971259799
Received: December 26, 2022 | Published: January 3, 2023
Citation: Kamal M. Uhl’s anomaly: A rare form of congestive cardiac failure in early childhood. J Pediatr Neonatal Care. 2023;13(1):1-3. DOI: 10.15406/jpnc.2023.13.00481
Uhl’s anomaly is a rare congenital anomaly of the heart in which there is a congenital absence of the right ventricular myocardium. Only a few cases have been reported in the literature. It normally presents in infancy with features of congestive cardiac failure; however, cases have been reported in adults with right heart failure. Although the prognosis is not good, palliative surgical modalities are being done in this population. We report below 2 cases of children with Uhl’s anomaly who presented to us with this rare condition and are un- der medical management.
Keywords: uhl’s anomaly, congestive cardiac failure, right ventricle, myocardium, right ventricular dysfunction
Uhl’s anomaly is a rare form of congenital right ventricular cardiomyopathy which is characterized by the partial or complete absence of right ventricular myocardium. The epicardium and endocardium of the right ventricle are opposed, but the septum and the papillary muscles of the right ventricle are normally muscularized. The condition is mainly sporadic, though some familial occurrences are present in literature. About a century ago, Ostler1 described the “parchment heart” but the first case was reported in 1952 by Henry Stephen Mc Graw Uhl.2 It is so rare condition that till 1993 only 84 cases were reported in a systemic review by Gerlis.3 A close differential diagnosis of this condition is ARVD (arrhythmogenic right ventricular dysplasia). We present the cases of 2 children who presented to us with this rare anomaly and are under medical management.
Case 1: 8 months old, apparently asymptomatic male child was referred from an outside hospital as a case of pulmonary atresia who presented there with excessive crying and breathing difficulty with mild cyanosis. On examination, the child had a heart rate of 106/ min, reg ular, BP: 98/58mm Hg, RR: 28/min with no retractions, Spo2: 90% room air. The cardiac apex was in the 4th intercostal space 0.5 cm lateral to the midclavicular line, the first sound was normal in intensity and duration, and the second heart sound had normal split and intensity. A soft pan systolic murmur of 2/6 intensity was heard at the lower left sternal border. Soft non-tender hepatomegaly of 1 cm was present with no splenomegaly. CXR revealed massive cardiomegaly. ECG showed sinus rhythm with right atrial enlargement. An echocardiogram revealed dilated right atrium and ventricles with a thin right ventricular lateral wall. The leaflets of the tricuspid valve were non-coating and thence, severe low-pressure tricuspid regurgitation. Severe RV dysfunction was present. The left ventricle had normal function.
A suspicion of Uhl’s anomaly was made, so a CMR (cardiac magnetic resonance) imaging was done which confirmed Echo findings of dilated RA, RV (RVEDV-123ml/m2) with severe tricuspid regurgitation. Poor right ventricular function (RV EF-15%) with thin free wall with flattened inter-ventricular septum during diastole. There was no evidence of fibro-fatty RV wall infiltration, thus ruling out ARVD. On delayed enhancement imaging, there was enhancement along the RV free wall, apical RV and RV portion of the distal IVS (Figure 1). Min- imal pericardial effusion was present. The CMR (cardiac magnetic resonance) findings con- firmed Uhl’s anomaly and parents were counselled about the management options and they did not prefer surgical palliation. The child was discharged on diuretics and ACE inhibitors and is in follow up without any symptoms presently.
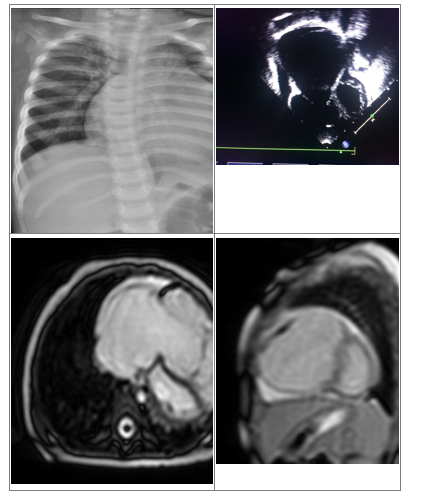
Figure 1 A: CXR showing cardiomegaly;
B: 2D Echo showing dilated RA and RV;
C and D: CMR images showing dilated RA, RV with thin RV free wall.
Case 2: 2 years old apparently asymptomatic boy was referred to us with an incidental murmur. On examination his vitals were normal with HR: 98/mins regular, RR-20/min, BP: 102/64 mm Hg, saturation in room air: 94%. Apex was in the 5th intercostal space 1 cm lateral to the midclavicular line. The first heart sound was normal in intensity and duration and the second heart sound was normal in intensity with normal splitting. A soft systolic murmur was present at the left lower sternal border. CXR showed mild cardiomegaly. Echocardiography showed dilated RA and RV with severe tricuspid regurgitation and right ventricular dysfunction. A diagnosis of organic TR was made, diuretics were started and the child was under follow up. The child developed features of congestive heart failure. CMR (cardiac magnetic resonance) imaging was done which showed dilated RA, RV with thinned out RV wall with- out any fatty infiltration of the RV wall, suggesting Uhl’s anomaly (Figure 2). Parents were in- formed about the condition and prognosis and they too preferred medical management over the palliative surgical procedure.
Uhl’s anomaly is the congenital complete or partial absence of the right ventricular myocardium. There is no evidence of deposition of adipose tissue, inflammation or necrosis. Since the first description of Uhl’s anomaly about 70 years back different theories have been proposed for this anomaly although the exact cause still is not known. Initially, it was thought to be due to embryologic failure of the right cardiogenic fold which in turn leads to a congenital absence of the right ventricular myocardium. Apoptotic destruction of the myocardium after the heart has fully developed is a recent explanation which has been given by some studies including Uhl’s himself too in 1996.4 A potential genetic predisposition is also a possibility as the anomaly has been described in twins and family members.5,6
In most cases, the anomaly presents in the early years of age with congestive cardiac failure.3 Cyanosis is also not so uncommon a symptom. Cases have been reported in which it has presented with massive peripheral edema of pleural effusion leading to cardiac tamponade.7,8 It may rarely mimic other congenital cardiac anomalies like Ebstein’s anomaly or even functional pulmonary atresia.9,10 The baby in our first case was referred to us with a diagnosis of pulmonary atresia. The association of other congenital anomalies with Uhl’s anomaly is relatively rare. The diagnosis of Uhl’s anomaly was done initially by Uhl’s on autopsy, but presently with the advent of echocardiography and cardiac magnetic resonance (CMR) imaging, early diagnosis is possible.11
Arrhythmogenic right ventricular dysplasia (ARVD) is a closely related entity to this condition.12 The characteristic feature of ARVD is fibro fatty tissue replacement of RV myocardium whereas the Uhl’s anomaly has a complete absence of muscle in the parietal wall of RV (composed only of the opposing layers of endocardium and epicardium). Features of these two conditions overlap each other, so Gerlis and co-workers 1993 enumerated certain fea- tures to differentiate between the 2 conditions.3 The diagnosis of UHL’s anomaly is favoured by the younger age of presentation, predominant features of cardiac failure, lack of family history and associated other congenital heart diseases. Even in Uhl’s anomaly, RV is known to be arrhythmogenic.
The prognosis of Uhl’s anomaly is not good and palliative surgical procedures are being done. The aim of surgical management of Uhl’s anomaly is the alleviation of right heart fail- ure by the complete exclusion of RV with bidirectional Glenn or Fontan connection or a reduction plasty of RV combined with bidirectional Glenn (one and a half ventricle). All these palliative procedures are being described with good results now a days.13
The authors acknowledge Mr. P Satheesh Kumar, Pediatric Echo Laboratory in charge for his technical assistance.
None.
The author declares no conflicts of interest.

©2023 Kamal. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.