Journal of
eISSN: 2373-4426


Research Article Special Issue Neonatal Illness I
1Department of Medical and Paediatric Oncology, Gujarat Cancer Research Institute, India
2Department of Neonatology, Fernandez Hospital, India
3Department of Paediatrics, PBM Hospital, SP Medical College, India
4Department of Paediatrics ,Umaid Hospital, SN Medical College, India
Correspondence: Deepak Sharma, Department of Neonatology, Fernandez hospital, Hyderabad, India,, Tel 9849590876
Received: January 17, 2015 | Published: February 27, 2015
Citation: Choudhary M, Sharma D, Nagar RP, Gupta BD, Nagar T et al. (2015) Clinical Profile of Severe Acute Malnutrition in Western Rajasthan: A Prospective Observational Study from India. J Pediatr Neonatal Care 2(1): 00058. DOI: 10.15406/jpnc.2015.02.00058
Background: Diarrhoeal diseases rank with acute respiratory infections as among the major causes of morbidity and mortality among children under 5 years of age. Probiotics has been used in the diarrheal episode and have been proved to be useful. The traditional Indian yoghurt which is easily available at all places is being used in Indian villages during episode of diarrhoea. There is only one study comparing the efficacy of yoghurt with probiotics and this study was done tocompare the efficacy and cost effectiveness of traditional yoghurt and probioticin the treatment of acute childhood diarrhoea.
Material and Methods: Children aged between three months to five years admitted with some dehydration due to acute diarrhoea were included. Children were randomised in to two groups comprising of 50 cases in each group, intervention group received traditional yoghurt and control received market available probiotic.
Results: Data was analysed with the help of SPSS version 16 and the continuous data were compared by Students ‘t’ test. The chi-squared test or Fischer’s exact test was used to test the difference between groups and statistical significance was considered as p ≤ 0.05. There was no significant difference between probiotic and traditional yoghurt when time of appearance of first semi formed stool {46.70 ± 14.40 Vs 50.64 ± 13.40 hours}, amount of stool passed per 24 hours {155.74 ± 74.27 Vs 167.53 ± 109.58 grams}, mean numbers of stools {6.29 ± 1.94 Vs 7.22 ± 2.63} and mean weight gain {121.94 ± 94.21 Vs 113.29 ± 73.85 grams} were compared. However, treatment cost with traditional yoghurt was almost half (7.20 Indian Rupees (INR) /patient/day) as compared to Probiotics (15.60INR/patients/ day).
Conclusion: Traditional yoghurt was equally efficacious to probiotics and the relative cost of traditional yoghurt was less than probiotic and is easily available at all places especially in the villages and rural areas of tropical countries.
Keywords: traditional yoghurt, probiotic, acute childhood diarrhoea
FAO, food and agriculture organization; WHO, world health organisation; ORS, oral rehydration salts; EDTA, ethylene diamine tetraacetic acid; INR, indian rupees
Diarrhoea is a Greek word that’s literal meaning is “to flow through like a stream”. Diarrhoea is defined as the passage of 3 or more liquid or watery stools in a day with change in consistency and character of the stools. Therefore diarrhoea is a symptom but it is also a sign when the loss of water (stool volume) is more than 15gm/kg/day in children < 3 year and > 200gm/day in children > 3year of age.1 Acute diarrhoea is rivalled in importance only by the respiratory infection, as a cause of morbidity on a world wide scale. Approximately 4.6 million children were dying each year by diarrhoeal dehydration, when the WHO initiated the diarrhoeal disease control program in 1980. According to recent reports oral rehydration therapy may now be preventing about three million dehydration deaths per year.2 In developing countries like India it still continuous to exert a high toll on children aged less than five year in form of a median of 3.2 episodes of diarrhoea per child - year and in estimates of mortality 4.9 children per 1000 per year died because of diarrhoea.
The management of acute diarrhoea consists of the replacement of lost fluid, glucose and electrolyte by oral rehydration solution. However, this solution reduces neither the severity nor the duration of diarrhea.3 A search has continued for an agent that could prove to be safe and efficacious in reducing the duration of diarrhoeal episode. In recent years it has been shown that probiotics can promote a more rapid recovery of acute diarrhoea. Yoghurt (yogurt, yoghourt, youghurt or yogourt) is a dairy product produced by bacterial fermentation of milk. Fermentation of the milk sugar (lactose) produces lactic acid, which acts on milk protein to give yoghurt its texture and its characteristic tang. Soy yogurt, a dairy yoghurt alternative, is made from soy milk. It is nutritionally rich in protein, calcium, riboflavin, vitamin B6 and vitamin B12. In India, yoghurt is commercially sold under the name “curd”, or more commonly under the local name of “dahi”.4 Probiotics are dietary supplements containing beneficial bacteria or yeast. According to currently adopted definition by FAO/WHO - Probiotics are “Live Micro-organism which when administered in adequate amount confers a health benefit on the host”.5 Till date so many studies have been conducted to evaluate the role of probiotics and yoghurt use in acute diarrhoea separately, in majority of these studies it was shown that probiotics and yoghurt (curd) both were effective to prevent and treat acute childhood diarrhoea. To the best of our knowledge no study in India has been done to compare the efficacy and cost effectiveness of traditional yoghurt and probiotic to treat the diarrhoea. So our study planned with the above objective kept in mind.
This study was conducted in the Department of Paediatrics, Regional Institute for Maternal & Child Health (RIMCH) - Umaid Hospital, Dr. S. N. Medical College, Jodhpur < Rajasthan India over a 12-month period. It was a time bound double blind non-inferiority randomized controlled clinical trial. The objective of the study was to compare the efficacy of curd (Natural Probiotic) with Probiotics available in market in term of correction of dehydration, reduction in diarrhoea duration & frequency.
Inclusion Criteria
Exclusion Criteria
Severe dehydration was not included in our study because these children required intravenous fluids for management and in the same way children with no dehydration were also not included in our study as they do not required hospitalization for management. The degree of dehydration was assessed in every case as per guidelines laid down by WHO.
The previous data were collected of over last six months of the admitted children aged between six months to five years admitted with some dehydration due to acute diarrhea of duration five days or less. Expecting a reduction of 20% and with an alpha error of 0.05 and power of 80% the sample sized required was 50 children in each group. The patient who met the inclusion criteria and satisfying the case definition were included in the study after taking consent for the same form the parents. The eligible children were allotted a study number. These numbers corresponded to the order of patients entering in the trial. Children were randomised in to two groups i.e. Group ‘A’ and Group ‘B’. A simple randomisation done using a computer generated random number table on a master list.
In our study we used low Osmolarity ORS (ORS - 224; marketed by CURATUO Health Care Pvt. Ltd.) with total Osmolarity - 224 mmol/litre, Glucose-84mmol/litre, Sodium - 60mmol/litre, Citrate - 10mmol/litre, Potassium - 20 mmol/litre & Chloride-50mmol/litre and offered at a rate of 75ml/kg in first 4 to 6 hours (approximately) for both study groups. It was followed by maintenance ORS at a rate of 10-20 ml/kg body weight for each loose stool. Group A (50 children) - were put on low Osmolarity ORS with usual diet and Indian Dahi (natural Probiotic). Indian Dahi (curd) was offered ad libitum (at least 15gm/kg body weight of patient per day for 3 days). Indian Dahi (Lf 40) containing 108 of each Lactococcus lactis, Lactococcus lactis cremoris and Leuconostoc mesenteroides cremoris per gram.
Group B (50 children) - were put on low Osmolarity ORS with usual diet and market available Probiotic (SPORLAC sachets; Manufactured in India by UNI-SANKYO LTD.). In Probiotics Lactic acid bacillus (Earlier known as Lactobacillus sporogenes) spores were used in dose of 1.35 x 109 spores per patient and given thrice a day for three days(1 sachet of 1gm powder contain not less than 150 million spores of lactic acid bacillus). This was a double blind study in which all the data were collected by a health care professional who was not aware of the group randomized and was trained prior to start of the study to fill the patient information leaflet for all investigations. A detailed history regarding epidemiological profile included residential status, source of water supply, type of house, family size, educational status of parents, type of feeding, socio-economic status (Percapita income) and history of present diarrheal episode (included duration, frequency, volume, consistency and color of stool with associated vomiting and other complaints) was taken at the time of admission and recorded on pretested proforma specially designed for this study. Each case was followed for next 72 hours.
If the patients of study group did not improve & needed intravenous fluids then these patients were excluded from study and considered as treatment failure. Every case was assessed clinically by weight, psyche (mental status), thirst, mucus membrane, eyes, tear, skin turgor, urine output, pulse, temperature, respiration, BP, degree of dehydration, stool volume & frequency, acceptance of the fluids and episodes of vomiting at the time of admission, at the end of 6 hr, 24 hr, 2nd day & 3rd day. The base line laboratory investigations included blood urea, serum creatinine, serum sodium and serum potassium that were performed on every case and repeated as and when required and data were recorded on a proforma specially designed for this study. Required amount of the ORS calculated (75ml/kg in four to six hour) and recorded on proforma. The actual amount of the ORS given to the patient in first six hours was also recorded. All the patients were weighed over electronic weighing machine (which shows weight at 5gm intervals that is within ± 5 grams range).
Blood samples (venous blood) were drawn with all aseptic precautions and a free flow of blood droplets was maintained. Blood samples (2ml) for blood urea, serum creatinine and serum electrolytes was collected in a dry, clean test tube, subjected to centrifugation and serum was analysed immediately in the research laboratory attached to our department. Blood for hemogram was collected in EDTA vial (1ml) and analysed in the central laboratory attached to the Umaid Hospital, Jodhpur. The serum electrolytes were performed by using ‘Flame photometry’ method as described by Harold Varley; the blood urea was done by using SEAC Computerised Photo analyser S-267 (manufactured by Ames Division of MILES India Ltd.), while the hemogram was done by using Haemo camp auto analyser (manufactured by MILES India Ltd).
For measuring stool volume in the cases of older children we collected the motion in a disposable container (cup or plastic glass) & for younger we first took weight of dry napkin or diaper, then the same diaper or napkin weighted with motion and subtracted dry napkin’s weight from wet napkin’s weight. Mothers were also educated/trained to collect urine in a container or bottle, for infants we used minicoms to collect the urine for measuring urine output. Patients were discharged 24 hour after cessation of diarrhoea (passage of formed stool or passage of no stool for 12 consecutive hours) or at the end of five day from admission. At the time of discharge each patient was categorized as having completed the trial, treatment failure (not improved or needed intravenous fluids) or as withdrawal (left the study in between/ absconded). Data was analysed with the help of SPSS version 16. Continuous data were compared by Students ‘t’ test. The chi-squared test or Fischer’s exact test was used to test the difference between groups. Statistical significance was set at P ≤ 0.05.
In our study mean age (in months) and mean weight (in kilograms) of patients were 16.88 ± 13.24 and 7.80 ± 2.25 respectively. The mean frequency of motions and duration of diarrhoea at admission were 8.20 ± 2.45motions/day and 2.17 ± 1.22 days respectively. All these parameters were comparable in between both of the groups as observed p values were non-significant. No significant difference was observed in two groups according to feeding pattern, severity of dehydration, presence or absence of vomiting and serum levels of sodium and potassium at the time of admission (Table 1). 60% children of study population had protein energy malnutrition while remaining 40% children had >90% weight for age. [Patients with PEM grade III and IV were not included in our study]. Distributions of cases according to demographic and social factors were comparable in both groups.
|
Characteristics |
Traditional yoghurt (Mean ± S.D.) |
Probiotic (Mean ± S.D.) |
P value |
Total |
|
Weight in Kg |
7.67± 2.32 |
7.93 ± 2.20 |
0.6 |
7.80 ±2.25 |
|
Age in months |
14.7+12.20 |
18.5± 13.98 |
0.1 |
16.88±13.24 |
|
Frequency of motions (per 24 hours) |
8.36±2.48 |
8.04 ± 2.43 |
0.5 |
8.20 ± 2.45 |
|
Duration of diarrhoea ”before enrolment” in days |
2.08 ± 1.29 |
2.27 ± 1.17 |
0.5 |
2.17 ± 1.22 |
|
Serum Sodium level in meq/L |
142.68± 11.80 |
142.76±11.95 |
0.9 |
142.72±11.90 |
|
Serum Potassium level in meq/L |
3.81±0.53 |
3.85±0.58 |
0.7 |
3.83±0.55 |
Table 1 Distribution of cases according to various admission characteristics
Out of 100 children, four children needed IV fluids (treatment failure), one child absconded (withdrawal) and 95 children improved. One absconded child belonged to probiotic group (B), while two children (4%) of each group needed IV fluids. Thus 96% of group ‘A’ children and 94% of group ‘B’ children were improved. Finally group ‘A’ comprised of 48 children and group ‘B’ had 47 children (Figure 1). No significant difference was observed in final outcome in group ‘A’ and group ‘B (p = 0.7) (Table 2).
|
Outcome |
Traditional yoghurt |
Probiotic |
|
Improved |
48 |
47 |
|
Failure |
2 |
2 |
|
Withdrawal |
0 |
1 |
Table 2 Final outcome of therapy in two groups
(X2=1.01, p value >0.7)
No significant difference was observed in hydration status of cases at six hour and 24 hour from admission in group A and group B (p value = 0.7). The time of appearance of first semi formed stool was earlier in probiotic group (46.70 ± 14.40 hours) then traditional yoghurt group (50.64 ± 13.40 hours), but difference was statistically insignificant (p = 0.2). The mean weight gain on completion of 72 hours was better in the probiotic group (121.94 ± 94.21 grams) then the traditional yoghurt group (113.29 ± 73.85 grams) with a p value 0.7 (statistically insignificant). The amount of stool (in grams) passed per 24 hours was slightly higher in traditional yoghurt group as compare toprobiotic group and remained statistically insignificant. Observed frequencies at 24 hour, 48 hour and 72 hour for probiotic and traditional yoghurt were 6.29 ± 1.94 and 7.22 ± 2.63 (p = 0.1), 2.93 ± 1.25 and 3.83 ± 1.66 (p = 0.01) , 1.8 ± 1.07 and 1.95 ± 1.21 per 24 hours(p value = 0.5) respectively (Figure 2). The numbers of stools at every point were less in probiotic, but again on statistical analysis it was not significant (Table 3).
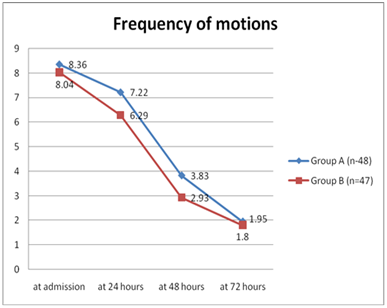
Figure 2 Showing response according to reduction in frequency of motions.
Group A is traditional yoghurt group, Group B is probiotic group.
|
Characteristics |
Traditional yoghurt |
Probiotic |
p value |
|
|
Time of appearance of first semi formed stool (in hours) |
50.64 ± 13.40 |
46.70 ± 14.40 |
0.2 |
|
|
Number of stools |
0-6 hours |
1.77±1.13 |
1.65±0.84 |
0.6 |
|
0-24 hours |
7.22±2.63 |
6.29±1.94 |
0.1 |
|
|
25-48 hours |
3.83±1.66 |
2.93±1.25 |
0.1 |
|
|
49-72 hours |
1.95±1.21 |
1.80±1.07 |
0.5 |
|
|
Stool weight |
0-6 hours |
46.14±44.83 |
46.06±30.62 |
0.9 |
|
0-24 hours |
167.53±109.58 |
155.74±74.27 |
0.5 |
|
|
25-48 hours |
81.56± 71.60 |
68.19±41.31 |
0.3 |
|
|
49-72 hours |
40.74±2.54 |
42.17±28.43 |
0.8 |
|
|
ORS consumed in first 6 hr (in ml) |
568.75±166.60 |
605.31±175.15 |
0.3 |
|
|
Weight gain in grams |
113.29±73.85 |
121.94±94.21 |
0.7 |
|
Table 3 Comparison of various parameters between traditional yoghurt (group A) and probiotic (group B)
At the admission the average weight of children was 7.8 kg. We offered traditional yoghurt and probiotic to the patients at the rate of 15gm/kg/day so required amount of yoghurt was about 7.8 x 15 = 117 gm/day/patient. At the time of study market value of traditional yoghurt (Dahi/ Curd) was 60Indian rupees (INR)/kg. So daily expenditure was about 7.20 INR/patient/day. For Group B daily cost of treatment was 15.60 INR/patient/day which was more than double the cost of traditional yoghurt.
Acute watery diarrhoea still remains a frequent condition, causing world-wide morbidity and mortality. However, the incidence, severity, morbidity and mortality due to this disease are substantially more in tropical countries then in other part of world. With use of ORS improving trends in mortality rates but there was no concurrent decrease in morbidity rates attributed to diarrhoea. A search has continued for an agent that could prove to be safe and efficacious in reducing the duration of diarrhoeal episode. For at least a century, researcher have hypothesized that live bacterial cultures, such as those found in yoghurt, may help to treat and prevent diarrhoea 4. In recent years it has shown that probiotics can promote a more rapid recovery of acute diarrhoea. Some common probiotics includes strains of various species of the Genera – Bifidobacterium (Bifidobacterium lactis, Bifidobacterium bifidum, Bifidobacterium breve, Bifidobacterium Infants, Bifidobacterium longus) and Genera- Lactobacillus (Lactobacillus acidophilus, Lactobacillus Casei, Lactobacillus Plantarum, Lactobacillus reuteri, Lactobacillus rhamnosus including Lactobacillus GG).
The mechanisms by which probiotics seem to be effective in controlling overgrowth of potentially pathogenic microorganisms include competition for colonization sites and nutrients, production of toxic compounds, modulation at the endogenous flora, enhancement of the intestinal barrier and stimulation of the immune system.5 Probiotics may promote nonspecific stimulation of the host immune system, such as immune cell proliferation, enhanced phagocytic activity, increased production of secretary immunoglobulin A6 and modulation of a variety of substances that are involved in healing of inflammation (such as interleukins, metalloproteinase and nitric oxide synthase NOS).7
In our study we showed that traditional yoghurt was equally efficacious to the probiotic which is sold by pharmaceutical companies clamming that these are better than traditional yoghurt. There was no significant difference in the hydration status in traditional yoghurt group at six hour and 24 hour from admission in comparison to probiotic group. Likely the time of appearance of first semi formed stool though was earlier in probiotic group but it was not statistically significant. Again the mean weight gain on completion of 72 hours was better in the probiotic group than traditional yoghurt group but was statistically insignificant. Similarly the amount of stool (in grams) passed per 24 hours, and stool frequencies at 24 hour, 48 hour and 72 hour were comparable showing equal efficacy of traditional yoghurt. The traditional yoghurt was equally efficacious to probiotic but was costing half to the cost of probiotic. The cost efficacy and easy accessibility of traditional yoghurt which is very crucial in tropical countries can make it very good and cheap alternative to probiotic.
Van Neil et al.,8 McFarland et al.,9 and Canani et al.,10 conducted meta-analysis of randomized, controlled studies to assess whether treatment with probiotics improved clinical outcome in children with acute infectious diarrhoea. They noticed reduction in diarrhoea duration and frequency in the participants who received probiotics compared to those who received placebo. Isolauri et al.,11s tested the effect of orally administered lactobacilli on acute rotavirus diarrhoea in 42 well-nourished children aged 5-28 months and found that the diarrhoeal phase was shortened in probiotic group. Billoo et al.,12 and Szajewska et al.,13 assessed the efficacy and safety of Saccharomyces boulardii in acute watery diarrhoea and observed that S. boulardii group had a significantly lower frequency as compared to control group. Henker et al.,14 conducted a study to assess the effect of Probiotic Escherichia coli strain Nissle 1917 (EcN) in acute diarrhoea in infants and toddlers and observeda significant superiority compared to the placebo. In India, study done by Khanna et al.,15 showed that there is no significant benefit of tyndalized Lactobacillus acidophilus (Probiotics) in acute diarrhoea in infants & children.
Yoghurt is also being used in the management of acute diarrhoeal disorders. This recommendation is based on the traditional approach in many countries all over the world, as well as on evidence gained in human intervention studies such as Boudraa et al.,16 Nizami et al.,17 Agarwal and Bhasin;18 Pashapour and Iou.19 Till date so many studies conducted to evaluate the roll of probiotics and yoghurt use in acute diarrhoea separately, in majority of these studies it was shown that probiotics and yoghurt (curd) both were effective to prevent and treat acute childhood diarrhoea.
To the best of our knowledge only on study in world has been done to compare the efficacy of traditional yoghurt and probiotic to treat the diarrhoea. The purpose of the trial was to evaluate the clinical efficacy and cost/effectiveness of Saccharomyces boulardii compared with yogurt fluid (YF) in acute non-bloody diarrhea in children. They enrolled 55 children in study and group A received lyophilized S. boulardii and group B received YF. They observed that the duration of diarrhea was shorter with S. boulardii but the hospital stay was reduced with YF, although these differences were not significant. Diarrhea resolved in significantly more children on day 3 in the S. boulardii group but in outpatient cases, yogurt treatment was cheaper than S. boulardii whereas in hospitalized patients, treatment cost was similar. They concluded that the effect of daily freshly prepared YF was comparable to S. boulardii in the treatment of acute non-bloody diarrhea in children.20 Our findings were contrary to observed by earlier worker that could be explained by small sample size of the study population because of which we were not able to find any statistically significant difference. But treatment cost with traditional yoghurt was almost half as compared to Probiotic. In addition to this advantage it is a part of Indian ancestral diet and has nutritive value; since most of our children with diarrhoea are already malnourished and traditional yoghurt can be easily mixed with rice or khichri, which make this diet more palatable and nutritive too.
The limitations of the present study are that
Finally, our study has shown that the use of traditional yoghurt is equally efficacious in the acute childhood diarrhoea as commercially available probiotic as there was no statistically significant difference observed in the various outcome variables. But traditional yoghurt has several advantages over probiotics, such as easy availability at all places especially in the villages and rural areas of tropical countries and more cost effective than probiotic products. So by this study we recommend universal use of traditional yoghurt (Indian Dahi) in acute childhood diarrhoea.
None.
None.
None.

©2015 Choudhary, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.