Journal of
eISSN: 2373-4426


Educational Review Volume 14 Issue 3
1MD, (Radiodiagnosis), Department of Radiodiagnosis, MGS Hospital, India
2MD (Pediatrics), Department of Pediatrics and Neonatology, Guru Gobind Singh Government Hospital, Government of Delhi, India
Correspondence: Dr. Abhinav Gupta, Department of Radiodiagnosis, MGS Hospital, Punjabi Bagh, New Delhi, Delhi-110026, India , Tel +919891070040
Received: November 22, 2024 | Published: December 6, 2024
Citation: Gupta A, Gupta AK. Radiology pearls: decoding abdominal x-ray interpretation in pediatric patients. J Pediatr Neonatal Care. 2024;14(3):199-203. DOI: 10.15406/jpnc.2024.14.00567
Abdominal X-rays have long been a cornerstone in the diagnostic workup of various gastrointestinal and abdominal pathologies in children.1 However, in the modern era of radiology, the landscape of diagnostic imaging has evolved significantly with the introduction of high-end modalities such as ultrasound, computed tomography (CT), and magnetic resonance imaging (MRI).1,2 These advanced imaging techniques offer superior visualization of anatomical structures and pathological processes, often leading to more accurate and timely diagnoses.
Despite the advantages of advanced imaging, the role of abdominal X-rays remains crucial in certain clinical scenarios. Abdominal X-rays are quick, cost-effective, and readily available, making them valuable tools in the initial assessment of patients with acute abdominal pain, suspected bowel obstruction, or perforation. Additionally, X-rays play a key role in monitoring the progression of certain conditions, such as bowel obstruction or abdominal distention.
However, the interpretation of abdominal X-rays requires a systematic approach. This paper explores the role of pediatric abdominal X-rays and their limitations in the era of high-end radiology investigations, highlighting key diagnostic radiological features and tips that aid in diagnosis of specific abdominal pathologies in neonates and children and when to order a high-end investigation.
Step 1: Quality of radiograph:
In a good quality radiograph, the entire abdomen should be visible, extending from the diaphragm to the pelvis, with adequate exposure for a detailed assessment of the bowel.
Step 2: Gas distribution pattern:
It is important to note the normal progression of air in the bowel after birth: gas should be present in the stomach immediately, within the duodenum at 1 hour, in the proximal small intestine at 3 hours, throughout the small bowel at 12 hours, and finally in the rectum by 24 hours.3 These timelines serve as a guide for assessing the normal passage of air through the gastrointestinal tract and can aid in identifying abnormalities in gas distribution that may indicate underlying pathology.
In infants under one year of age, the normal gas pattern on an abdominal X-ray appears honeycomb or polygonal shaped throughout the abdomen (Figure 1).3,4
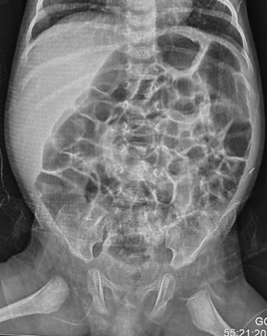
Figure 1 Anteroposterior supine radiograph in a normal neonate on day-3 of birth showing honeycomb or polygonal gas pattern throughout the abdomen with gas visible in the rectum. It is difficult to differentiate small from large intestine in the neonatal period.
Note the presence of a gasless abdomen or paucity of gas (Figure 2), as well as excessive gas in either the small or large bowel. Additionally, observe the presence of gas in the rectum.

Figure 2 Anteroposterior supine abdominal radiograph in a 4-year-old child showing paucity of gas, few dilated small bowel loops with smooth walls (few valvulae conniventes can be seen), some gas visible in distal bowel loop suggestive of a proximal or high, partial small bowel obstruction.
Absence of rectal air in infants aged more than 24 hours indicates an obstruction.
In older children, normally the gas distribution is good throughout the abdomen.
However, in small bowel obstruction, there is too much gas in the small bowel loops compared to the colon. Conversely, in colon obstruction with intact ileocecal valve, there is too much gas in the colon (Figure 3) compared to the small intestine and there is little or no gas in the rectum.5 The lack of gas in the rectum, however, is a late sign of bowel obstruction, so patients who present early in their disease process may have gas in the rectum on radiograph.

Figure 3 Anteroposterior supine abdominal radiograph in a 4-year-old child showing dilatation of bowel with smooth walls with too much gas in colon (haustra can be seen to identify colon) and absence of gas in the rectum suggestive of distal large bowel obstruction at level of rectosigmoid junction probably due to Hirschsprung’s disease.
In paralytic ileus, there is too much gas in both small and large bowels (Figure 4 & 5).

Figure 4 Anteroposterior supine abdominal radiograph in a 4-year-old child showing multiple dilatated bowel loops scattered throughout the abdomen haphazardly with presence of gas in the rectum suggestive of paralytic ileus.
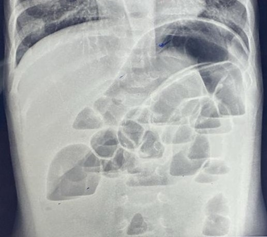
Figure 5 Anteroposterior supine abdominal radiograph in a 9-month-old infant with abdominal distention following diarrhea showing dilatated bowel loops with smooth walls scattered throughout the abdomen haphazardly with presence of gas in the rectum suggestive of paralytic ileus.
Detection of intramural gas in bowel wall which appears as a curvilinear or linear radiolucency paralleling the bowel wall, termed pneumatosis intestinalis, indicates necrotizing enterocolitis (NEC).6 There may be gas in the portal vein and its branches seen as branching of a tree upwards. It is most commonly seen in the right lower quadrant as NEC usually affects the terminal ileum and the ascending colon.
Step 3: Look for dilatation of bowel loops:
In neonates, dilatation of bowel loops is defined by the diameter of any single loop exceeding the transverse dimensions of a lumbar vertebra, specifically the interpedicular width of the L2 vertebra.3 This condition is characterized by the loss of the normal honeycomb/polygonal appearance of the bowel.
In older children, bowel dilatation is defined based on the diameter measurements: the small bowel exceeding 3 cm, the colon exceeding 6 cm, and the cecum exceeding 9 cm. This concept is commonly referred to as the "Rule of 3-6-9".3 However, when the small bowel diameter exceeds 6 cm, the large bowel exceeds 9 cm, or the cecum surpasses 12 cm, there is a significantly increased risk of bowel rupture. On radiographic imaging, a dilated bowel appears as smooth-walled and distended
Step 4: Check the number of dilated bowel loops, whether > 3 or ≤ 3:
The greater the number of dilated small bowel loops visible, the more distal the obstruction. Three or fewer dilated small bowel loops indicate a high or proximal obstruction (Figure 2& 7), while more than three dilated loops indicate a low or distal obstruction (Figure 6).3

Figure 6 Anteroposterior erect abdominal radiograph in a 6-year-old child showing dilated small bowel loops with multiple air-fluid levels, air-fluid level of unequal heights in the same bowel loop and absent of colon gas.
High bowel obstruction is up to Jejunum whereas low obstruction is in ileum/ or colon. Both can be complete or partial. In complete obstruction (Figure 3), there is no gas distal to the site of obstruction whereas in partial obstruction, some gas is able to pass through the obstructed segment (Figure 2 & 7), resulting in the presence of gas distal to the obstruction.
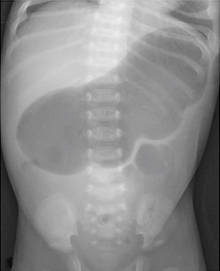
Figure 7 Anteroposterior erect abdominal radiograph in a 4 weeks aged neonate a single gaseous shadow of a markedly dilated stomach (caterpillar sign) with scattered gas in distal bowel segments, indicative of partial gastric outlet obstruction most probably due to hypertrophic pyloric stenosis.
Distally located atresia (complete obstruction) usually presents with delayed symptoms compared to proximal ones.
In low or distal obstruction, failure to pass meconium beyond 48 hours of age is the main symptom. Vomiting and abdominal distention are late features. Abdominal radiograph shows more than 3 dilated small bowel loops and colon due to non-use of colon of small width termed microcolon.
In complete high obstruction on radiograph no further imaging study is needed. However, in partial obstruction or doubtful imaging results, the upper GI contrast study is indicated.
Step 5: Identifying dilated bowel loops: whether small bowel or large bowel:
In neonates and infants, distinguishing between the small and large bowel is challenging as the loops are featureless and the colon lacks haustra (Figure 1). Additionally, the loops do not conform to anatomically predictable locations. In neonates and infants, the dilated bowel has smooth walls unlike older children.
In older children, like adults, the small bowel is centrally located, framed by the large bowel. The small bowel's mucosal folds, called valvulae conniventes, are visible across the full width of the bowel. The large bowel has pouches or sacculation called haustra that protrude into the lumen. Haustra are thicker than valvulae conniventes and typically do not appear to completely traverse the bowel (Figure 3). If the dilated bowel loops exhibit valvulae conniventes, it indicates involvement of the small intestine. Conversely, if they show haustra, it suggests involvement of the colon.
Step 6: Assessing if there is differential or diffuse dilatation of the whole bowel:
Mechanical intestinal obstruction typically causes differential bowel dilatation (Figures 2 & 6), where the loops proximal to the point of obstruction dilate while points distal to the obstruction collapse.
In small bowel obstruction, there is dilation of the small bowel loops that are disproportionate to the colon. Conversely, in colon obstruction with an intact ileocecal valve, the colon dilates from the point of obstruction backward disproportionately to the small bowel, leading to collapse of points distal to the obstruction.
In paralytic ileus there is uniform dilatation of bowel to the level of the rectum (Figure 4 & 5).
Step 6: Check for presence of air-fluid levels in AP erect position:
Air fluid levels are common in normal bowel, specifically on radiographs obtained in the upright position and on lateral shoot through abdominal views; but multiple ones (>3 air-fluid levels) usually indicate intestinal obstruction.
The best radiographic signs of small bowel obstruction are multiple (>3) air-fluid levels (Figure 6) , air-fluid levels with a width of 2.5 cm or more, and air-fluid levels of unequal heights differing more than 5 mm from one another in the same small bowel loop, and absent colon gas.
In colon obstruction, air fluid levels are not present because water is absorbed in colon (Figure 3).
In paralytic ileus, there are few and less dilated air fluid levels scattered throughout the abdomen (Figures 4 & 5).
Step 7: Check for arrangements of bowel loops in AP supine position:
In obstruction, fluid levels are short and on an erect film the gas pattern is often described as a step ladder pattern (Figure 6).
In paralytic ileus, the loops are scattered disorderly throughout the abdomen (Figures 4 & 5).
Step 8: Any extraintestinal gas/free air (pneumoperitoneum):
The presence of air under the diaphragm in erect radiograph indicates bowel perforation. If air leak is small the free air can only be detected on dorsal decubitus film.
Normally only the inner wall of the bowel should be visible on an abdominal X-ray. The presence of free air within the abdomen can result in both sides of the bowel wall becoming visible. This is called “Rigler’s Sign”. In massive pneumoperitoneum, there is an ovoid lucency with the visible falciparum ligament outlined by free air. This is called “Football Sign”.
It is possible, using careful radiographic technique, to demonstrate as little as 1 mL of free gas on an erect chest or left lateral decubitus abdominal films.7 The high percentage of missed cases is due to technical imperfections rather than limitations of the test.
Look for signs of specific intestinal lesions/ pathologies [Different case Scenarios]:
Single gas bubble:
A neonate aged 2-12 weeks presented with forceful projectile, non-bilious vomiting, and failure to thrive. Abdominal X-ray (Figure 7) reveals a single gaseous shadow of a markedly dilated stomach with scattered gas in distal bowel segments, indicative of partial gastric outlet obstruction, possibly hypertrophic pyloric stenosis.3
Double gas bubble:
A neonate presented with either bilious or non-bilious vomiting. The abdominal X-ray shows two large upper abdominal gas bubbles, one on each side of the midline, with an absence of gas in the distal bowel. This finding indicates complete duodenal obstruction, which can occur either distal or proximal to the ampulla of Vater. This specific pattern is characteristic of duodenal atresia.3
Another neonate with similar clinical presentation. The abdominal X-ray reveals two large upper abdominal gas bubbles, one on each side of the midline, with a small amount of gas in the distal bowel. This finding indicates partial duodenal obstruction, which can be either distal or proximal to the ampulla of Vater. This pattern may suggest duodenal stenosis, duodenal web, or annular pancreas.3
Triple gas bubble:
A neonate presented with abdominal distention and bilious vomiting at less than 2 days age. The abdominal X-ray reveals three lucencies in the upper abdomen with no distal gas.
This is the classical sign of Jejunal Atresia.3
Multiple dilated bowel loops with multiple air fluid levels
A 7-day old neonate presented with abdominal distention, and bilious vomiting. The abdominal X-ray reveals multiple dilated bowel loops, with an abrupt cutoff i.e. with no distal gas in the colon and rectum. There are greater than 3 air-fluid levels in upright radiograph.
This is consistent with distal small bowel obstruction due to ileal atresia.3
Hugely dilated loop of bowel arising from pelvis and pointing upwards towards diaphragm
A 13-year-old girl presented with colicky abdominal pain, vomiting, and constipation. X ray abdomen shows hugely dilated loop of bowel with loss of haustra, arising from her pelvis and pointing towards diaphragm. It has coffee bean appearance. Frimann Dahl’s Sign is positive with three dense lines converging toward the site of obstruction. Her rectum still contains some air. It is consistent with sigmoid volvulus.3,4
Hugely dilated loop of bowel in center of abdomen with preserved haustra and non-dilated small intestine loops present in right lower abdomen
A 15-year-old boy presented with colicky abdominal pain, vomiting, and abdominal distention. X ray abdomen shows hugely dilated large bowel loop with preserved haustra in the center of abdomen indicating volvulus of caecum. Its place is taken by small intestine identified by presence of valvulae conniventes.3,4
A neonate failed to pass the meconium after 48 hours
On X ray abdomen performed after 48 hours of age shows dilated bowel loops in the abdomen with absence of gas in the rectum. This differential diagnosis includes Hirschsprung’s disease and rectal atresia. Even ileal atresia cases have no gas in rectum.3,4
Fluoroscopy guided contrast enema is indicated. In Hirschsprung’s disease there is reversal of recto-sigmoid ratio.3,4 Normally the rectum is often larger than the sigmoid colon and recto-sigmoid ratio is more than 1. In babies with short segment disease, it is reversed. In ileal atresia in contrast study there is microcolon due to non-use.3,4
In imperforate anus, where there is no anal opening, an invertogram is typically performed after 24 hours of age. This imaging technique helps characterize the type of anal atresia by measuring the distance between the gas bubble in the terminal rectum and the perineal skin. A distance greater than 2 cm indicates a high-type defect, while a distance less than 2 cm indicates a low-type defect.3,4
Pitfalls of plain abdominal radiograph
On plain abdominal radiography, a small bowel loop can be identified by intraluminal air outlining valvulae conniventes.3,4 However, if a small bowel loop is completely filled with fluid, it may not be visible on a plain abdominal radiograph. This limitation can lead to an underdiagnosis of small bowel obstruction, as plain radiography may not accurately estimate the level of obstruction. The sensitivity and specificity of abdominal radiographs in the evaluation of mechanical small-bowel obstruction are poor, with a failure to confirm the diagnosis in a third of cases. Plain abdominal radiographs can yield false-negative, non-specific, or positive results. Most of these scenarios often result in the need for a CT scan which can identify fluid-filled bowel loops just proximal to the obstruction, which plain radiography cannot detect. However, both CT and plain abdominal radiography can produce false-negative diagnoses, particularly when the bowel is not dilated due to vomiting or nasogastric tube decompression, or when an examination is conducted before fluid can accumulate proximal to the obstruction.8
While plain abdominal radiography has a sensitivity and specificity of 84% and 72%, respectively, in detecting large bowel obstruction (LBO), patients with suspected LBO typically require urgent CT scans for a more definitive diagnosis. CT scans have a higher sensitivity and specificity (96% and 93%, respectively) in identifying the cause of LBO, including intraluminal, mural, and extraluminal causes.8
The American College of Radiology (ACR) eliminated abdominal pain as an indication for abdominal radiography in its 2011 revision. Plain abdominal radiography has limited diagnostic value in diagnosing conditions such as intussusception and acute appendicitis.9,10 Ultrasonography has emerged as the "gold standard" for noninvasive imaging in these cases.
At times, abdominal radiographs in children reveal abnormalities that are difficult to interpret, requiring advanced imaging studies for a definitive diagnosis. For example, an abdominal radiograph (Figure 8) of a 2-year-old child presenting with abdominal pain showed a distended stomach and duodenum, with collapsed small bowel loops, and scanty gas in the distal bowel. These findings underscore the importance of further evaluation with contrast studies to determine the underlying condition.

Figure 8 Anteroposterior erect abdominal radiograph in a 2-year aged child with abdominal pain (without any vomiting or abdominal distention) showing dilated stomach and duodenum, with collapsed small bowel and scanty gas in distal bowel.
Plain abdominal x-ray studies are of limited utility in the evaluation of liver disease, as they add little diagnostic value.11 Ultrasonography is often the initial radiologic study of choice for many hepatobiliary disorders due to its relatively low cost, lack of ionizing radiation, and bedside capability.
Plain abdominal radiography is not typically used as a primary method to detect ascites, although it can indirectly indicate its presence. Some indirect signs include changes in the hepatic angle or the presence of a flank stripe sign.12 Ultrasonography is considered the most sensitive technique for detecting ascites. In patients with minimal ascites, fluid tends to collect in the most dependent spaces, such as the hepatorenal recess (Morison’s pouch) and the pelvic cul-de-sac, allowing for the detection of less than 10 mL of fluid. In infants, ultrasonography can detect as little as 10 to 20 mL of fluid in the perivesical area. Additionally, besides confirming the presence of ascitic fluid, the ultrasonography can reveal other findings that may help determine the underlying cause.
Plain abdominal radiography is not accurate for detecting pneumoperitoneum, with studies showing specificity ranging from 53% to 89.2%. CT scans are extremely sensitive (92%) and specific (94%) for GI perforation and offer additional value by providing more detailed information on the location and underlying cause of the perforation, and it can also help in identifying alternative diagnoses.8
The Royal College of Radiologists (RCR) guidelines13 for the appropriate use of abdominal radiographs recommend advising abdominal X-rays in specific clinical scenarios. These include suspected bowel obstruction, acute exacerbation of inflammatory bowel disease, palpable abdominal mass, severe constipation, foreign body ingestion, pancreatitis, and abdominal injury. Meanwhile, the American College of Radiology (ACR) guidelines14 suggest that computed tomography is more appropriate than plain abdominal films for evaluating suspected bowel obstruction. However, these guidelines primarily apply to adults.
Diagnostic utility of abdominal radiographs in neonates & children in resource limited settings
Despite these limitations, plain abdominal radiographs have greater diagnostic utility in neonates and children, yet their role is often undervalued compared to modern imaging modalities. In resource-limited settings, where high-end radiological investigations may not be available and financial constraints require careful allocation of medical resources, abdominal radiographs offer a cost-effective and practical initial screening tool for specific clinical scenarios. They are especially useful for diagnosing small or large bowel obstructions, evaluating neonates who fail to pass meconium within 48 hours of birth, and assessing conditions such as abdominal distention, or bilious or non-bilious vomiting. In older children, radiographs are similarly valuable for evaluating the cause of abdominal distention, constipation, or diagnosing suspected bowel obstruction or perforation. When in doubt, contrast studies are indicated to close the diagnosis.
None.
This research received no external funding.
The authors declare no conflicts of interest.

©2024 Gupta, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).
World Down Syndrome Day is observed on 21 March 2026 to raise awareness about Down syndrome and to
promote inclusion, early intervention, and quality healthcare for children with genetic conditions. This day highlights the importance
of pediatric monitoring, developmental support, and continued research to improve health outcomes and overall well-being.
Researchers, pediatricians, and healthcare professionals are invited to submit their original research articles, reviews, and clinical
studies related to Down syndrome, neonatal screening, developmental pediatrics, and child health. Manuscripts submitted on the occasion
of World Down Syndrome Day will be eligible for a special publication discount of 30–40% in the Journal of Pediatrics & Neonatal Care (JPNC).