Journal of
eISSN: 2373-4426


Research Article Volume 1 Issue 3
1Department of Public Health, Jigjiga University, Ethiopia
2Department of statistics, Jimma University, Ethiopia
3Department of Public Health, Haramaya University, Ethiopia
Correspondence: Gudina Egata, Department of Public Health, Haramaya University, Harar, 18087, Ethiopi, Tel +2519-1164-1362
Received: May 25, 2014 | Published: July 5, 2014
Citation: Seifu W, Assefa G, Egata G (2014) Prevalence of Exclusive Breast Feeding and its Predictors Among Infants Aged Six Months in Jimma Town, Southwest Ethiopia, 2013. J Pediatr Neonatal Care 1(3): 00017. DOI: 10.15406/jpnc.2014.01.00017
Background: Breastfeeding is an important public health strategy for improving child and maternal health conditions. However, the prevalence of exclusive breastfeeding is very low in many low-income countries including Ethiopia. Therefore, this study was conducted to determine the prevalence of exclusive breastfeeding and associated factors among infants aged six months in Jimma town, Southwest Ethiopia.
Materials and methods: An institutional based cross-sectional study conducted with qualitative inquiry from January to February 2013. Quantitative data were collected from 422 mother infant-pairs attending health institutions in Jimma town using a pretested structured questionnaire. The qualitative data were generated through focus group discussions among purposely selected discussants. Odds ratio with 95% confidence interval was estimated using multivariable logistic regression to identify independent predictors of exclusive breastfeeding while thematic framework analysis was employed for the qualitative data.
Results: The majority (96.6%) (95% CI: 0.86-0.97) of the mothers have ever breastfed their infants. The prevalence of exclusive breastfeeding was 67.2% (95% CI: 0.83-1.03), 24.3% (95% CI: 0.71-0.86) and 8.4% (95% CI: 0.13-0.34) at the age of ≤ 2, 3-4 and > 4months respectively with a mean duration of 3.2 months. Having good knowledge on breastfeeding {AOR: 2.1 (95% C.I: 1.54 - 4.33)}, age of infants ≤ 2months {AOR: 2.1 (95% CI: 1.67- 3.31)}, lower parity (≤1) {AOR: 3 (95% C.I: (2.2- 6.08)}, and having antenatal care visit {AOR: 1.2 (95% C.I (1.06-4.08)} were independent predictors of exclusive breastfeeding practice.
Conclusion: The prevalence decreases dramatically as the age of the infants’ increases. Being younger age, positive perception on the adequateness of breast milk, having one child and attending antenatal clinics during pregnancy was predictors of exclusive breastfeeding in this study. Hence, providing behavioral change communications using multiple channels including mass media and antenatal counseling is recommended to promote exclusive breastfeeding practices in the studied community.
Keywords: exclusive breast feeding, infant, prevalence, factors, Jimma, southwest ethiopia
ANC, antenatal care; AOR, adjusted odds ratio; CI, confidence interval; COR, crude Odds Ratio; EBF, exclusive breastfeeding; EDHS, Ethiopian demographic and health survey; FGD, focus group discussion; MDGs, millennium development goals; SD, standard deviation; SPSS, statistical package for social sciences; UNICEF, united nations children’s fund; WHO, world health organization
Breastfeeding is an important public health strategy for reducing infant and child morbidity and mortality as well as reducing maternal morbidity and mortality. The World Health Organization (WHO) and United Nations Children’s Fund (UNICEF) recommend that all mothers should breastfeed their children exclusively for the first 6 months and thereafter they should continue to breastfeed for as long as the mother and child wish, and both appropriate and sufficient weaning food should be added after six months of life.1,2
Exclusive breastfeeding (EBF) has been defined as the situation where the infant has received only breast milk from his/her mother or a wet nurse, or expressed breast milk and no other liquids, or solids, with the exception of drops or syrups consisting of vitamins, minerals supplements, or medicines for the first six months.2 In order to achieve the Millennium Development Goal (MDGs) of reduction of child mortality, infant breastfeeding has been identified as one of the major intervention areas both globally and nationally.3 Infants who have been breastfed optimally have reduced risk of common childhood illnesses such as gastrointestinal and respiratory infections, otitis media, atopic eczema, and allergy during childhood and also chronic non communicable diseases such as obesity, diabetes mellitus and cardiovascular diseases.2,3
Despite its demonstrated benefits, EBF prevalence and duration in many countries including Ethiopia is lower than the international recommendation of exclusive breastfeeding for the first six months of life.1-5 A cross-sectional community based study that was carried out in Jimma Arjo Woreda and Goba district indicated that the crude prevalence of exclusive breastfeeding was 52.1% and 71.3%.6,7 respectively . The prevalence of exclusive breastfeeding in Ethiopia was 50% but the prevalence decreases progressively as the age infants’ increases.8 The low prevalence of EBF in most developing countries including Ethiopia is attributed to various factors that differs from community to community and from set up to set up.8-14 Exclusive breastfeeding practice was highly affected by cultural malpractices, attitude and knowledge of the mothers and or care givers.15-19 As the age of the child increases the rate of EBF decreased significantly which is evidence with studies done in Ethiopia, Uganda, Nepal, and Nigeria.6,20-22 Mothers having antenatal care (ANC) visits are more likely to promote exclusive breastfeeding practice since mothers get more information which encourage exclusive breastfeeding practice during the first six months.23,24 while having positive perception about the adequateness and balanced nature of breast milk alone for the first six month was positively associated with exclusive breastfeeding practice.16,25
Planning, implementation, and evaluation of programs to promote appropriate infant feeding practices require detailed current information about these practices in the target population. However, these efforts are not based on systematic evidence on the level of existing practice which might be due to the scarcity of data from studies on exclusive breastfeeding. Therefore this study was conducted to assess the prevalence of exclusive breastfeeding and its predictors among infants under six months of age in Jimma town. Based on this information stakeholders will take actions accordingly to improve child health status in the study area. Ultimately maternal and child health will be improved and then they will become a productive community members who have a distinctive role in their community.
The study was conducted in Jimma town which is located 335Km from the capital city Addis Ababa in the Southwest Ethiopia. In the town, most people are engaged in commercial activities as a major livelihood means. There are 5 public health institutions (3 health centers & 2 hospitals) and 18 non-governmental health institutions owned by NGO’s and private owners which provide different services for the community.26
An institutional based cross sectional quantitative study supplemented with qualitative inquiry was conducted among randomly selected mothers of infants under six months of age in Jimma town from January to February 2013. The sample size for the quantitative study was determined using a single population proportion formula with the following assumption: Prevalence of exclusive breastfeeding to be - 47.9%,6 margin of sampling error tolerated- 5% (0.05), critical value at 95% confidence interval of certainty (1.96), and 10% for non response making the final sample size of 422 mother infant pairs. For the qualitative approach 2 Focus Group Discussion (FGD) which contained 8 individuals in each group were conducted among purposely selected health professionals and mothers in the study community.
The participants were selected systematically from three governmental health centers and two hospitals in the study area. The sample size was proportionally allocated to the health institutions based on the total mother infant pairs visiting per day seeking for vaccination and other medical services for their infants. Each mother infant pairs were selected and interviewed every one interval which was determined by statistical formula until the desired sample size was achieved for the respective health institutions. The quantitative data were collected using a pretested structured questionnaire while the qualitative data were collected through focused group discussion among purposely selected mothers and health professionals from the respective health institutions. The quantitative data were collected using structured and pretested interview questionnaires while focus group discussion was used to collect the qualitative data. A structured questionnaire was used to collect data on the socio demographic characteristics, maternal and child characteristics, knowledge and attitude towards breastfeeding and as well cultural beliefs regarding infant feeding practices.
Data collectors were given three day training on the questionnaires and interviewing techniques. The questionnaires were initially prepared in English and then have been translated into the local language, Afan Oromo and again it was translated back into English to check its consistency. The questionnaires were pre-tested before the actual data collection. Additional modifications were made to the questionnaire in terms of in terminologies and formatting based on the pretest findings. The supervisors checked each completed questionnaire and principal investigator monitored the overall quality of the data collection. Moderators for the FGD were given two day training on how to chair the discussion and other related issues. They had been moderated with help of a check list prepared by the investigators for this particular study.
In this study , exclusive breastfeeding was defined in this study as the situation where the infant has received only breast milk from his/her mother or a wet nurse, or expressed breast milk and no other liquids, or solids, with the exception of drops or syrups consisting of vitamins, minerals supplements, or medicines in the first six months. Respondents were said to have good knowledge if they answered at least 70% of the questions related with breastfeeding practice. Their attitude was measured through seven closed ended questions using Likert scale was applied ranging from 1= strongly disagree to 5=strongly disagree. The total sum score was calculated and those who scored above the mean were considered as having positive attitude towards exclusive breastfeeding practice. On the other hand, low parity was understood as a mother having one live birth during the study period.
Quantitative data were cleaned, edited, and entered onto Epidata version 3.2 and exported to SPSS version 16 statistical software for analysis. Frequency distribution and cross tabulation were done against the variables of interest. Bivariate analyses were done to assess the association between explanatory variables and outcome variable of the study. All variables with a p-value of < 0.3 at the bivariate analysis were included into multivariable logistic regression model in which odds ratio with 95% confidence intervals were estimated to identify independent predictors of exclusive breastfeeding. P-values less- or equal to 0.05 were employed to declare the statistical significance. The qualitative data were analyzed through thematic framework analysis after summarizing the data into different thematic areas and the results were triangulated with the quantitative findings. The study was cleared from the ethical review board of Jimma University College of Natural Science. Official recognition and support was secured from the relevant organizations and departments. The interviewees have also been informed about the aim of the study. Additionally, written and verbal consent were secured from the study participants. Finally, confidentiality was ascertained by justifying that no information was disclosed individually without the full willingness of the respondent.
Majority (56.65%) of the respondents were ≤ 25 years of age while 166 (40.5%) were between the age group of 26-35 years of age with mean (±SD) age of 25.46 (± 5.01) years. Similarly majority of the respondents 280 (68.3%) were from Oromo ethnic group. More than half of the respondents were Muslims 235(57.3%) by their religion (Table 1).
Variables |
Frequency(n) |
Percent(%) |
Maternal Age(Years) |
||
≤ 25 |
232 |
56.6 |
26-35 |
166 |
40.5 |
36-45 |
12 |
2.9 |
Ethnicity |
||
Oromo |
280 |
68.3 |
Amhara |
64 |
15.6 |
Gurage |
27 |
6.6 |
Tigrea |
8 |
2.0 |
Others |
31 |
7.6 |
Religion |
||
Muslim |
235 |
57.3 |
Orthodox |
120 |
29.3 |
Protestant |
45 |
11.0 |
Catholic |
10 |
2.4 |
Occupation |
||
Gov’t employed |
78 |
19.0 |
Merchant |
28 |
6.8 |
House wife |
273 |
66.6 |
Private employed |
14 |
3.4 |
Daily labor |
13 |
3.2 |
Others |
4 |
1.0 |
Educational Status |
||
Illiterate |
101 |
24.6 |
Literate |
309 |
75.4 |
Marital status |
||
Married |
378 |
92.2 |
Unmarried |
32 |
7.8 |
Income |
||
300- 800 birr |
259 |
63.2 |
800-1300 birr |
87 |
21.3 |
1300-1800 birr |
25 |
6.1 |
> 1800 birr |
39 |
9.5 |
Table 1 Socio demographic characteristics of respondents among mother infant pairs in Jimma town, February, 2013(n=410)
Among the study participants, 220(53.7%) (95% CI: 0.451-0.572) had good knowledge while 190 (46.3%) (0.234-0.672) had poor knowledge about breastfeeding practice. Among mothers who had ever breastfed, most 312(76.1%) of them mentioned that breastfeeding should be initiated within one hour after delivery and 98(23.9%) initiated breastfeeding within the period of one hour to one day. Regarding timely initiation of breastfeeding, a 34 years mother with one month infant made the following remark, “...As usual most mothers initiate breastfeeding after one and half hour. I initiated breastfeeding after 4 hour because I had abdominal cramp and associated illness”. Similarly, a nurse from Jimma University Specialized Hospital stated that mothers who deliver at health institution started breastfeeding as soon as possible since we counsel and advise them about benefit of early initiation of breast milk for the infants and the mothers but mothers who deliver at home didn’t provide breast milk soon due different cultural beliefs and attitudes.
Fifty two (12.6%) of the study participants were mentioned that 4 month as the cut off point for exclusive breastfeeding. “A women having 5 months aged infant stated… I started to give other foods besides breast milk after 4 months since his age was four months where by breast milk alone was not enough”, on top of this a nurse mentioned that… “I faced many women who squeezed out colostrums since they believe that it might cause ill health effect on their infants but I tried to educate them about what colostrums is and its benefit for their infant”.
The majority of the study participants 303 (73.9%) (95% CI: 0.651-0.784) had positive attitudes towards breastfeeding practice. With regard to the reason for mixed feeding a 24 years old mother stated that “...my infant’s stomach cannot be filled with my breast milk alone and hence I gave cow milk and others accordingly”. Majority (34.9%) of the respondents strongly disagree to provide breast milk to their infants at public places whereas 128 (31.2%) were neither support nor oppose public place feeding of breast milk for infants. In support of discouraging public place feeding of breast milk a 27 years old mother said… “providing breast milk at public place such as market, religious places and other places where people are gathered was not good for my infants since at public place it causes health problem to my infant following evil sprite”.
Even though the majority of the respondents 396(96.6%) (95% CI: 0.861-0.972) fed their infant’s breast milk, the prevalence of exclusive breastfeeding was 60.0% (95% CI: 0.553-0.649) of the mothers. Exclusive breastfeeding was a norm at younger age where by 160(67.2%) infants below 2 and 58(24.3%) infants between 2-4 months were exclusively breastfeed. However, as the age of the infants increases, >4months only 20(8.4%) of the infants have been exclusively breastfed ().
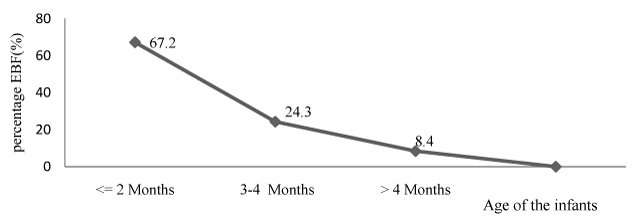
Figure 1 The pattern of exclusive breastfeeding practice as the age of infant’s increases among infants under six months, in Jimma town, Southwest Ethiopia, February, 2013.
In the multivariable logistic regression analysis, infants aged 2 months and below {AOR=2.1, CI: (1.67-3.31)}, being low parity {AOR=3, CI: (2.21-6.08)}, having ANC visit {AOR=1.2, CI: (1.06-4.00)}, and having good knowledge on breastfeeding {AOR=2.1, CI: (1.54-4.33)} were the independent predictors of exclusive breastfeeding among the infants aged under six months (Table 2).
Characteristics |
Exclusive Breastfeeding |
COR |
AOR |
|
|
Yes |
No |
(95% CI) |
(95% CI) |
Age of the mother(year) |
||||
≤ 25 |
141(62.7) |
84(37.3) |
1.00 |
1.00 |
26-35 |
94(59.1) |
65(40.9) |
0.9(0.57-1.32) |
1.4(1.05 - 6.32) |
36-45 |
25(3.0) |
9(75.0) |
0.2(0.05-0.75) |
0.8(0.15 - 2.75) |
Parity |
||||
1 |
129(69.0) |
58(31.0) |
2(1.32-3.08) |
3.0(2.2 - 6.08)** |
2-4 |
98(52.4) |
89(47.6) |
1.00 |
1.00 |
≥ 5 |
11(50.0) |
11(50.0) |
0.9(0.38-2.10) |
0.8(0.68 - 2.10) |
Age of the infant |
||||
< 2 months |
42(93.3) |
3(6.7) |
4(1.17-13.31) |
2.1(1.67- 3.31)* |
2-4 months |
163(78.0) |
46(22.0) |
1.1(0.5 - 1.14) |
0.9(0.76 - 5.14) |
> 4 months |
33(23.2) |
109(76.8) |
1.00 |
1.00 |
ANC Attendance |
||||
Yes |
207(59.7) |
140(40.3) |
2.2(2.06-4.08) |
1.2(1.06 - 4.08)* |
No |
31(64.6) |
17(35.4) |
1.00 |
1.00 |
Maternal occupation |
||||
Office worker |
54(59.3) |
37(40.7) |
1.00 |
1.00 |
House wife |
115(59.6) |
78(40.4) |
2.4(3.01- 6.09) |
1.0(0.53-2.26) |
Daily laborer |
69(61.6) |
43(38.4) |
0.6(0.46-1.02) |
0.7(0.28-1.52) |
Knowledge on breastfeeding |
||||
Good |
135(64.0) |
76(36.0) |
3.3(1.39- 4.24) 1.00 |
2.1(1.54 -4.33)*1.00 |
Poor |
164(44.3) |
206(55.7) |
|
|
Attitude towards breastfeeding |
||||
Positive |
183(63.1) |
107(36.9) 51(48.1) |
1.6(1.01-2.49) |
1.4(0.71-3.01) |
Negative |
55(51.9) |
|
1.00 |
1.00 |
Table 2 Predictors of exclusive breastfeeding among infants under six months in Jimma town, Southwest Ethiopia, 2013
* = p<0.05
** = p<0.01
This study attempted to determine the prevalence and associated factors of exclusive breastfeeding practice. The prevalence of ever breastfeeding was 96.6% while the crude prevalence of exclusive breastfeeding was 60.1%. In the multivariate analysis, infants aged 2 months and below, being low parity, having ANC visit, and having good knowledge on breastfeeding were the independent predictors of exclusive breastfeeding among the infants aged less than six months.
Majority (96.6%) of mothers practiced ever breastfeeding to their infants. This figure is similar to the EDHS 2011 report whereby ever breastfeeding rate of the country was (98%) and (98%) for Oromia region. The prevalence of other regional states in Ethiopia ranges from 93.4% in Addis Ababa to 97% in Harari.8 which was comparable with this study finding.
Although World Health Organization (WHO), global and national infant and young child feeding guidelines recommend that all newborns should be exclusively breastfed their infants for the first six months, the crude prevalence of exclusive breastfeeding in this study was 60.1%. This was lower than Goba district (71.3%) and Sir Lanka (75.8%).7,17 while higher than the finding from Arjo woreda Jimma, EDHS 2011, Saudi Arabia and Nigeria whereby the prevalence of exclusive breast feeding were 52.1%, 50%, 8.3% and 19%.6,8,19,22 respectively. This difference might be attributed that in our study majority (66.6%) of study subjects were house wife’s whereby the probability of exclusive breastfeeding is expected to be higher. Additionally Jimma town is one the Jimma university community based education site where by students from different disciplines are deployed year to year and because of this the study community might have better awareness about the issue.
Month-specific prevalence of exclusive breastfeeding decrease progressively as the age of the infants’ increases where by the prevalence was 67.2%, 24.3% and 8.4% at age ≤2 months, 3-4months and >4months respectively. This finding was comparable with a study finding in Nepal.21 which showed that the prevalence of exclusive breastfeeding were 74%, 24% and 9%, and EDHS, 2011.8 70%, 55%, and 32% at 1 month, 3 months and above 4 months respectively. As infants grew older and older, the prevalence of exclusive breastfeeding decreases significantly indicating the overall lower duration of exclusive breastfeeding in the study community. This is common in many developing countries as majority of mothers believe that breast milk alone was not sufficient as the age of infants grew older and older. Additionally they might become pregnant and they started to wean the infant through formula and other substitutes accordingly.
In the current study, knowledge of mothers about optimal breastfeeding recommendation was 53.7% which is lower than the study finding in Malaysia (74.8%).15 This difference might be attributed due to the difference in awareness level about breastfeeding practice. Qualitative finding also indicted that even though health information dissemination through Jimma university community education is high, there are still mothers who don’t have sufficient knowledge about the recommended breastfeeding practice in the study communities.
This study found that most (73.9%) showed favorable/positive attitude towards breastfeeding which was consistent with the study finding in Malaysia (83.9%) had positive attitude towards breast feeding practice.15 Although, in this study the attitude towards breastfeeding was generally favorable, 58.5% respondents do not agree on banning of bottle feeding. This is probably due to women started to join the work force and they would not spent much of their time with their infant at home and hence the possibility that they leave their infant with house workers, relatives or others and prefer to use bottle-feed with substitutes.
In multivariate analysis infants at younger age (≤ 2months) are 2 times more likely to be exclusively breastfed as compared to infants above 4months which was consistent with a study finding in Ethiopia, Bolivia, Uganda, Nepal, and Nigeria.6,18,20-22 exclusive breast feeding decreases as the age of the infants increases. This might be due to the mothers might think that breast milk alone was not enough as the infant get older and older and hence they provide additional food items other than breast milk. Additionally short birth interval/spacing as the case of developing country including Ethiopia reduces the duration of exclusive breastfeeding of infants in the first six months.
Being lower (≤1) parity were positively associated with exclusive breastfeeding practice which is consistent with a study done in Sir Lanka.17 whereby mothers having two and below children were more likely to practice exclusive breastfeeding practice. This might be due to mothers having few children were more concerned and worried about their infants since they have high passion unlike the one who have many children. A focus group discussant mother stated that we provide breast milk alone for six months at first delivery since I spent most of my time at home with my infants since I love him too much. But after the second child the responsibility to lead my family becomes too high and I began to work different activities to support my families and hence breastfeeding alone for the first six month is impossible and challenging.
Mothers having antenatal care (ANC) visits were more likely to practice exclusive breast feeding which was in line with a study done in Taiwan, Sudan and Egypt.12,23,24 This is true since mothers get more information that encourages and fosters exclusive breastfeeding practice during ANC visits. This idea was supported by a qualitative finding from a Nurse working at Jimma University Specialized Hospital when mothers are counseled and discussed very well the probability of exclusive breastfeeding will be high since they are eager and much more confidence to implement the advice of health professionals. But I think health care professionals are not doing very well especially in this regard.
Having good awareness on the adequateness and balanced nature of breast milk alone for the first six month was positively associated with exclusive breastfeeding practice. This finding was in line with a study done in Taiwan, Tanzania and Rural Uttar Pradesh.12,16,25 A mother from the qualitative group discussion group stated that supplementary foods were given because women and elders in the family perceived that mother’s milk is not sufficient for the child after the age of 3-4 months. She has reported that the child cried frequently, even soon after breastfeeding, because the child was still hungry. This might be attributed to if the mothers or care givers perceive breast milk is enough for the infants in the first six month they don’t provide anything else unless and otherwise ordered by health professional.
Since the study design was cross sectional cause and effect cannot be ascertained. Despite the above mentioned limitation the study has the following strength such as the quantitative finding was supported with qualitative data generated through focus group discussion among selected groups. Additionally the study includes mothers whose infants are six months and below where by recall bias might be minimized.
Even though the crude prevalence of exclusive breast feeding was high, age specific prevalence of exclusive breastfeeding decreases progressively as the age of the infants’ increases. In the current study, knowledge of mothers about optimal breastfeeding recommendation was lower than from other studies done in developing countries. However most of the study population had positive/favorable attitudes towards exclusive breastfeeding practice during the first six months. Being younger age (≤ 2months), having ANC visit, being lower parity and having good knowledge on breastfeeding were the independent predictors of exclusive breastfeeding practice in the studied community. Thus strengthening and promoting ANC visit with adequate counseling and discussion about breastfeeding issues focusing on the age for breast milk only, on the adequateness and balanced nature of breast milk for infants. Moreover, health information dissemination to bring behavioral change about exclusive breastfeeding practice using accessible means such as mass media and public meeting places as there is still low awareness about optimal breastfeeding within the study community.
None.
The authors have no conflict of interests related to this publication and have not received any grants.
None.

©2014 Seifu, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.