Journal of
eISSN: 2373-4426


Review Article Volume 3 Issue 1
1Department of Pediatric Neurology, "P & A Kyriakou" Children's Hospital, Athens 11527, Greece
2National and Kapodistrian University of Athens, Greece
3Department of Neonatology, Aretaieio Hospital, Greece
Correspondence: Nicoletta Iacovidou, Assistant Professor of Pediatrics-Neonatology National and Kapodistrian University of Athens, Medical School, Department of Neonatology, Aretaieio Hospital, Athens, Greece, Tel 302000000000, Fax 302000000000
Received: September 20, 2015 | Published: October 13, 2015
Citation: Mouskou S, Troizos-Papavasileiou P, Xanthos T, Iacovidou N (2015) Neonatal Transportation through the Course of History. J Pediatr Neonatal Care 3(1): 00104. DOI: 10.15406/jpnc.2015.03.00104
The knowledge of history forms the basis for the present and guides new generations for the future. The present review attempts a historical overview on the evolution and establishment of the neonatal transportation from ancient times to present, time coinciding with rapid and important developments in this area. The aim is to elaborate on personal efforts of individuals- known and unknown to the public- that dedicated themselves to this goal and pioneered the development of a worldwide neonatal transportation system.
Keywords: neonatal transportation, history, incubator, ground transportation, air transportation
IWM, infant welfare movement; USA, United States of America; NICUs, neonatal intensive care units; CDC, center for disease control and prevention; ELBW, extremely low birth weight; AAP, American academy of pediatrics; ACOG, American college of obstetricians and gynecologists; EUROPET, European network perinatal transport; MOSAIC, models of organising access to intensive care for very preterm births
Neonatology emerged after remarkable scientific observations and technological innovations, in order to meet the need for critical care of a vulnerable infant population. This paper deciphers the ancient Greek myths, mentions the earliest references of the care of neonates and illustrates the specific historical time context when milestones in Neonatology were observed. It also aims to acknowledge the contributions of individuals over the last century, whose efforts resulted in neonatology advances (appropriate oxygen delivery, incubators) perinatal health care system establishment and the expansion of both air and ground neonatal transportation.
‘The history of medicine should have a more important place in the education of medical students. Neglecting history is like erasing memory. Ignoring the past is destroying an important part of science, which is past experience. Neglect of history represents a lack of respect for our roots and leads to identity crises. History is the necessary ingredient for future experiments.1
Paul Louis Toubas
The first reported neonatal transportation in mythology
The word ‘transportation’ derives from the Latin words ‘portare’ (to carry) and trans- (across). In the context of patient transportation, the word means “to carry the patient to a nursing entity”. The respective Greek word is found in a quotation of Phrynichos, dated back to the 6th century BC, where it is stated “the one, who transported Europe”.2,3
Dionysus, the god of the grape harvest, winemaking and wine, ritual madness, fertility, theatre and religious ecstasy, was born prematurely, after 8 months of gestation, and needed special care. Mercury/Hermes, the first neonatal transporter ever-recorded, transferred Dionysus to Mountain Nyssa, where Nymphs took care of him; this is first reported neonatal transportation. It is said that Nymphs placed Dionysus in a cave, at the entrance of which there was a dense ivy curtain (cover and protection from air currents) and pines (forming an air filter). Its dome was covered with vine branches, creating a double wall, which helped maintain stable environmental temperature. In this case, “the young God’s incubator”, he remained until he grew up and gained his normal weight.
Disabled infants in ancient times - creatures of “a lesser God”
However, the problem in antiquity was how society would get rid of the disabled infants and not how and where they would transfer and take care of them. These children were considered a burden to society and an obstacle to the fulfillment of the needs of other family members. In the ensuing years, among the more civilized nations, only healthy and strong infants were acceptable as they would become capable warriors when they grew up and they would be useful to society; the sick and weak were driven to death. In ancient Sparta, a committee of elderly citizens examined every newborn. Once the newborns were healthy and of good build, they were transported to the “Public Nursery” and handed over to the City-State where they were raised under special care. In the opposite case, the congenitally malformed infants4 were dismissed in Taygetus Mountain, where they would die of ‘natural causes’; thus the State would not be defiled by their execution. It is no wonder that ancient Spartans were the most healthy and well raised tribe of their time.
Neonatal care in Ancient times - Views of enlightened minds
Despite the lack of practical interest, Hippocrates, the Father of Medicine, mentioned the significance of the perinatal period for newborns’ later life since the 5th century B.C. He stated that newborns at birth should adapt to a new breathing and nutrition status, independent of the placental-fetal circulation. Any aberration could lead to neonatal disease or even death due to harmful food- and breathing-associated agents. (“On the Seventh Month's Foetus” (Loeb Classical Library edition 9) “On the Eighth Month's Foetus (Loeb Classical Library edition 9”, 12, 12.1-12.14). He also knew, that neonates born two months earlier, usually do not survive, as they are small and have difficulties adapting to the extrauterine environment,5 which was considered a basic condition for neonatal survival. This perception is still valid in the pediatric society. Soranus of Ephesus, the Father of Obstetrics/Gynecology, described similar views in a more refined form, in the first half of the 2nd century AD. In his book ‘On the care of the infant’ he elaborated on this issue in the first chapter, entitled ‘How to recognize infants, who deserve further nurture’. He also set the following guidelines/rules on the assessment of the newborn’s condition, especially helpful for the midwives.
They should first determine the newborn’s gender, and then they should assess the physical and mental status of the baby, taking into consideration the duration of pregnancy and problems during its course. Soranus of Ephesus clearly mentioned that health problems of the pregnant woman adversely affect the fetus. He also prompted midwives to notice if newborns were born at the appropriate time, at term (9 months of gestation), post-term (after 9 months of gestation), or prematurely. They should also examine the intensity and quality of newborns’ cry or its absence. In order to access the aforementioned issues newborns’ sensory organs, ears, noise, pharynx, urethral and rectal openings, should be evaluated. Later on, midwives should examine the limbs, joints movements, skin appearance and turgor. In case handicaps or weaknesses were documented, newborns would not be considered candidates for further support.6
From ancient times to the 19th century
Until the end of the 19th century, no one had seriously dealt with neonates/infants. Home delivery was the usual practice. Preterm and sick neonates often died without any medical intervention. Except orphanages, where mortality rate was up to 85-95%, there were no other institutions for neonatal care.7 However, looking back in history, there are a number of individual observations, inventions and achievements in the field of Obstetrics and Neonatology, which per se helped the development of Neonatology and contributed to a gradually increasing neonatal survival rate Table 1.
|
1834 |
First description of neonatal endotracheal intubation (Blundell)50 |
|
1853-55 |
Establishment of Children Hospitals, Great Ormond Street Hospital,51 Nursery and Child's Hospital in New York City52 Children’s Hospital of Philadelphia53 |
|
≈1864 |
Correlation of cerebral palsy with birth trauma and asphyxia (Dr. Little)54 |
|
1891 |
Support for the first time of oxygen use in premature infants |
|
(Dr. Bonnaire)55 |
Table 1 Milestones in neonatal and perinatal medicine
At the same time, the Industrial Revolution of the 19th century, led to a great number of women working in factories. Inevitably an increase in formula administration occurred. This resulted in the greatest recorded infant mortality rate of more than 230/1.000 live births in 1870s.8 This epidemiological fact, combined with the reduced number of births by the end of the 19th century, resulted not only in the fear of population shrinking but also in a possible threat for national security. Europe thus, driven by specific political and social concerns of the time, was led to the Infant Welfare Movement (IWM) (1870–1920), which aimed at preserving the life of every single newborn, including the preterm ones.
“The revolution of the incubator”
The end of the 19th century was the “golden era” for advances in clinical Neonatology, with the introduction of incubators and the establishment of neonatal special care units. In 1878, the French obstetrician Stephane Tarnier amended a heated chamber, used for poultry farming, into the so–called Tarnier-Martin Couveuse incubator. The incubator concept was not a new one, as Jean Louis Paul Denuce (1824-1889) was the first one in 1857 to mention its use for the care of preterm neonates.9 However, Tarnier-Martin Couveuse incubator was the first of the closed-type one, made of wood and glass. Its primary principle was based on the use of heating air, being the ancestor of all modern types of neonatal thermo-protection equipment Figure 1. Nonetheless, it was a primitive and bulky construction, which could accommodate 1-2 infants. Furthermore, in the Maternity Hospital of Paris, under the direction of Professor Tarnier, in 1883 his colleague Auvard (1855-1941) made valuable observations and published the first documented scientific work with statistical data on the results of incubator use.4,10 This discovery gave a different twist in neonatal treatment and survival. This was reflected in the infant mortality rate reduction from 66% to 38% for newborns with a birth weight<2000 grams.11 Tarnier-Martin Couveuse Incubator made its first appearance in Paris Maternity Hospital in 1881, while in 1895 in the same hospital the first specialized neonatal intensive care unit, the “Pavilion for weaklings” was established by Pierre Budin (1846–1907), another colleague of Tarnier.1,12
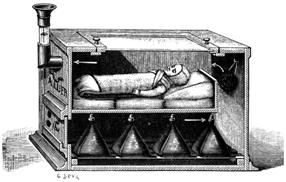
Figure 1 Tarnier's incubator, about 1883.
Available from URL: http://fn.bmj.com
With the intention to make French technology internationally known, Budin and his assistant Martin Couney launched in 1896 a strange and controversial project of organizing incubator exhibitions, which lasted for the next 40 years. They sent 6 incubators to the Exposition of Berlin Figure 2 and in their effort of making the whole project more realistic they exposed neonates from the local maternity unit to the incubators. This action was considered “acceptable”, as the newborns’ chances of survival were truly low. Couney named his exhibition Kinderbrutanstalt (“child hatchery”). Luckily, all 6 newborns survived.13 The exhibition was considered extremely successful and Couney was invited to Great Britain in 1897 to present his incubators/devices in the Victorian Era Exhibition. The maternity hospitals of the country though, did not consent to expose newborns in the exhibition, and Budin sent preterm neonates from France. [Their transportation through the Channel was held within 3 laundry baskets, with containers, which were heated by hot water.]The exhibition for preterm infants in Chicago in 1914 resulted in the establishment of the Premature Infant Station at Sarah Morris Hospital, part of Michael Reese Hospital in Chicago.14
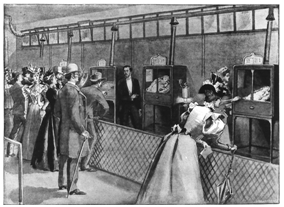
Figure 2 Neonates displayed in incubators at the Berlin exposition. Resource: baby incubators at the Berlin exposition. The graphic. 1896; 54:461.
A detailed description of Dr. Couney’s permanent exhibition is found under the title “Dr. Martin Couney and the Coney Island 'Child Hatchery'” “After traveling exhibitions throughout Europe and the US for a few years, Dr. Couney set up a permanent exhibition in the newly opened Luna Park at Coney Island. In those days, hospitals had no special care for premature babies, so Couney was never short of patients. The sign above the door read “Life Begins with the Baby Incubator” Figure 3. The inside was essentially a hospital. The atmosphere was quiet and clinical, incubators lined the walls, and trained nurses were employed to care for the babies. One of the nurses was Couney’s daughter, who ironically enough was born premature and spent some time in the incubator herself. The rules and regulations for infant care were strictly enforced, and professionalism was emphasized. The medical profession that had once called him into question eventually embraced his methods and began promoting their use and sending him patients. Dr. Couney would eventually open more incubator attractions. a couple more at Coney Island and a handful around the country at other amusement centers and fairs. It’s reported that over 40 years of operation, Couney’s incubator attractions had an 80% success rate and saved about 6500 newborns from almost certain death”.15 However, despite Boudin’s and Couney’s contribution to the expansion of incubator use, little was developed in the field of neonatal transportation.
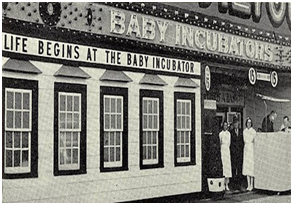
Figure 3 Dr. Couney’s permanent exhibition in the newly opened Luna park at Coney island.
Available from: URL: www.themeparkinsider.com
The beginning of an enormous effort
Neonatal transportation started basically in 1900 by the American physician Joseph Bolivar DeLee (1869 –1942), who was not only the Founder of Lying-in Hospital but was also regarded as the Father of modern Obstetrics. He showed great interest in Neonatology and preterm infants,4 recognizing the necessity for the creation of a thermo-regulated environment during their transfer.16–18 By the end of 1899, the Chicago Tribune described one of the innovations of the hospital, as the first portable transportation incubator. That device, also known as "hand ambulance", gave the opportunity to transfer newborns from their homes, where they were born, into the hospital.
A detailed description of the ambulance-incubator was published in 1903 in Neoplasm under the title «The smallest ambulance in the World” Figure 4. “The “baby ambulance” was 12 (length) x 22 (width)x 11 (height) inches, constructed of quarter-sawed oak and polished to a fine finished”. Cans of hot water were the heat source, and a metal water jacket lined the incubator. A battery-powered light bulb provided the physician with vision of the baby and of the temperature inside the incubator. A lamb was fueled by alcohol, kerosene, or oil to heat the water jacket if necessary. Babies weighing 1 to 4 lbs. were received in the baby ambulance, with prompt response to the delivery of the premature infant being a standard of care”.19,20
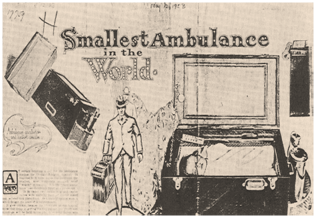
Figure 4 The smallest ambulance in the World (From the Neoplasm, 1903).
Available at: The pediatric clinics of North America/Transport Medicine/April 1993.
DeLee described the outcome of the first 28 babies, who were placed in the incubators at the Chicago Lying-In Hospital, and wrote in The Chicago Medical Recorder in 1902 “Of these, 8 died in a few hours, usually being frozen or in convulsions on arrival at the hospital”.19
Similar results, regarding mortality rate of the transferred neonates, were published by J. Zahorsky in his book Baby incubators, in 1905.21 He was a Pediatrician and Head Physician for the "Baby Incubators on the Pike", which was an incubator exhibition in St Louis Figure 5. In one of his medical articles published in the St. Louis Courier of Medicine (1905) Zahorsky writes, “Recognizing that the prevention of the initial heat-loss is most important the management early made provisions to minimize this danger. An ambulance and driver were provided which could be called upon day or night. A receptacle, in the nature of a small portable incubator, was utilized to keep the baby warm. The house physician and one of the nurses were usually dispatched to get the infant when a telephone message was received. Occasionally, due to a variety of causes, the infant could not be reached for three or four hours, but most commonly our physician, nurse and ambulance reached the premature infant in less than two hours, nevertheless, the number of infants for whom we were asked to send and had expired on arrival of the ambulance was very large. It is true that after it became generally known that the Incubator Institute was caring for all premature babies free of charge physicians, midwives and parents would send for the baby ambulance for miscarriages of 4 1/2 to 6 months”.22

Figure 5 Report of neonatal vital signs data. From: J. Zahorsky Baby incubators (1905).
Available from: URL: http://www.ebooksread.com/authors-eng/john-zahorsky/baby-incubators-a-clinical-study-of-the-premature-infant-with-especial-referen-hci.shtml
In 1914, J.H. Hess, who served as Professor of Pediatrics in Illinois University, designed functional incubators, heated by electrical current. Among his contributions was a relatively simple and commercially successful portable incubator designed for neonatal transportation. “A simple transportation incubator can be made by employment of an ordinary obstetrical bag with a false bottom. Hot-water bags or bottles can be carried in the lower compartment, and the infant in the bag proper. In the United States of America (USA), commercial production of incubators had already started in 189323 and the Hess portable incubator was built by V. Mueller Company in Chicago. “It was a 24x15x17 inch box covered by leather with access ports for oxygen administration and a small window for ventilation Figure 6. At first, taxicabs were used as ambulances with trained public health nurses in attendance” Figure 7. In 1934 Cooney donated a vehicle which was the first exclusive neonatal transport unit. It was used for the transport of newborns in Chicago World's Fair neonatal exhibition which was held in the Chicago Department of Health.19 Despite these encouraging efforts, the negative established perception about prematurity had to be overcome. In 1928 Capper characteristically wrote that. The fate of immature children is not enviable; almost one half of them die during the first year of life. Of those that remain alive, the majority are physically as well as mentally underdeveloped. When they are passed in review, one is surprised at the variety and amount of abnormality encountered, almost a regular “pathologic museum”.
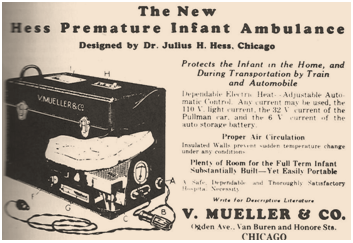
Figure 6 The new Hess premature infant ambulance (Courtesy of Lawrence gartner, MD). Available from: The pediatric clinics of North America/Transport Medicine/April 1993.

Figure 7 Some of the earliest neonatal transport units as we know them today were developed by Dr. Julius H. Hess in Chicago around 1923.
Available from: URL: www.neonatology.org
Evelyn Lundeen, a colleague of Hess sharing the same vision for neonates, was the first supervisor of the largest premature infant station in the USA, at the Michael Reese Hospital in Chicago. Both Hess and Lundeen stated that. ”Oxygen must always be available to the infant during transportation” and recommended a nurse should accompany the infant. In case the infant was in poor condition, they recommended “delay of the transportation for 8 to 24 hours, while the infant was treated with oxygen in an incubator until he or she improved”. In 1949 they published a second edition of the “Premature Infant”. An entire chapter was devoted to the transportation of these infants to neonatal units, which was recommended for those “who weighed less than 4.5 lbs, if the baby was cyanotic and required oxygen, or if the conditions of the home were inadequate”.24,25 After World War II, incubators had a new design, which included walls made of thin lucite. The practice of placing the neonates naked in these transparent boxes was quickly established.23 Silverman and associates published in the 1950s and the 1960s a series of randomized control trials, using different humidity standards and environmental temperatures. They proved that the survival of preterm infants could be increased by increasing either environmental temperature or environmental humidity.26
The organization of the neonatal transportation system
The first organized transportation program was held in 1948 (New York Premature Infant Transport Service) by the New York Department of Health in collaboration with regional hospitals.27,28 This remarkable system, was created more than a decade before the Neonatal Intensive Care Units (NICUs) establishment, and incorporated many of the main characteristics of the modern neonatal transportation units. It had specially trained nurses on 24-hour a day basis, a vehicle for exclusive use, someone in charge for the recording of phone calls, and finally, someone in charge of the control of the required equipment for neonatal transportation. During the next 2 years, 1209 patients were transferred under this program, 194 of them with birth weight<1000 grams.28 Knowledge expansion in neonatology along with great technological advances resulted in the establishment of several NICUs across Europe, Australia and North America,29 during the second half of the 20th century. Furthermore, the idea of transportation of preterm and severely sick neonates to regional centers was conceived in order to receive optimal treatment. In 1966, the first newborn with brocho pulmonary dysplasia was transferred to the California University Hospital, in San Francisco by the NICU staff. Three years later the first transportation of a pregnant woman in preterm delivery from one city to another was recorded. The change of the term “preterm neonates unit” to “special care unit” and finally to “NICU” reflects a gradual shift of interest from premature to critically ill newborns.9 After that, a great number of pediatricians became specialized in Neonatology. In 1975 the first examination for the Sub-Board of Neonatal-Perinatal Medicine of the American Board of Pediatrics were implemented. At the same period, the meeting of the Perinatal Section of the American Academy of Pediatrics was held for the first time.30
In the late 1970s the number of organized transportation programs remarkably increased. Regionalization (the model of regional distribution of perinatal health care system) became a necessity. This revolutionary remodeling of the health care system, applied already in some states of the USA during World War II, was an extremely effective concept, especially for patients with special surgical conditions. It was evident among the scientific community that under special circumstances, the delivery and the neonatal care in specialized centers with modern infrastructure had a beneficial outcome. The idea of organizing a regional perinatal healthcare system was thus implemented by the USA Public Health programs. This regionalization reduced the number of neonates who required transportation and prompted the idea of intrauterine transportations. This was mainly recorded in North America.29 It shifted though the responsibility of the transportation of the neonates in need of special care from the referral hospitals to the tertiary nursery centers. In addition, regional and tertiary hospitals organized transportation teams and implemented collaboration projects among these teams.
A remarkable example was the establishment of a regional perinatal access program (Stanford/Lucile Packard Children’s Hospital Neonatal Transport Program) in 1970, aiming at covering the medical needs of several cities of Northern California. However, the transportation of critically ill newborns could not last for more than 30 minutes, as life support and temperature control could not be achieved for long. Clinical evidence suggested that the transportation of these infants could significantly reduce the mortality and morbidity rate. According to the Center for Disease Control and Prevention (CDC) until the early 1980’s, infant mortality declined rapidly by an average of 4,5 percent per year, from 24,7 in 1965 to 11,9 in 1981.31 Healthcare personnel in charge for the transportation of sick neonates should be specially trained. In order to achieve this, perinatal programs were established.29 This effort resulted in a remarkable improvement of infant morbidity32 and mortality33 rates during the next decade. At the same time the percentage of the extremely low birth weight (ELBW) and critically ill neonates, transferred to tertiary hospital centers, increased.
In parallel with the expansion of ground neonatal transportation systems, air transportation began to develop. The first air neonatal transportation was held in 1958 with the fixed wing transport Colorado Air National Guard.19 In 1967, the transportation of a preterm infant to St. Francis Hospital, Peoria, Illinois with Peoria Journal Star helicopter was the first one using first motor wing.19 In 1970 Shepard described for the first time a flying intensive-care newborn nursery in the military system, on a C-9 aircraft. “An especially Sierracin cradle warmer with removable end pieces, monitor for heart rate, respiratory rate, and blood pressure, volume respirators and laboratory equipment for blood gas determinations with micro electodes. The infant is cared for by the flight pediatrician and by the flight nurse”34 Figure 8. Air neonatal transportation policy began in 1972 with the Flight for life Denver’s Saint Anthony Hospital.35

Figure 8 Infant transported by aircraft in continuous warmth, oxygen and fluids administration, and ventilation assistance. Available from: Sheppard KS Air transportation of high-risk infants utilizing a flying intensive-care nursery.
Neonatal transportation, its inclusion in the formal guidelines, as a special scientific field
In 1968 the Department of National Health and Welfare in Canada issued for the first time guidelines for the transportation of the mother or the newborn to tertiary hospitals.36
In 1976 American Medical Board representatives in collaboration with the American Academy of Family Physicians, the American Academy of Pediatrics (AAP), the American College of Obstetricians and Gynecologists (ACOG) and the National Foundation-March of Dimes established the Committee on Perinatal Health. This committee aimed at reducing maternal, perinatal and neonatal morbidity and mortality. During this period, they published the document “Towards Improving the Outcomes of Pregnancy, Recommendations for the Regional Development of Maternal and Perinatal Health Services”. With this declaration, they proposed the development of regional Perinatal Healthcare Centers and defined the three hospital levels of neonatal care. They emphasized the significance of the uniform data collection and training.37 Furthermore, they advocated that regionalization could improve the specialized care provision and reduce the cost. This was the core of the organization of perinatal healthcare system in the USA in the 1970s and 1980s acting as a national reference model for the development of neonatology centers.19 These guidelines were certainly a useful aid for other countries as well, which organized the expansion of regional perinatal healthcare systems in the next years.
The need for a quick and safe transportation of sick and injured patients to tertiary centers led to the introduction of specialized transportation teams for children and neonates.38 The ΑΑΡ published in 1986 the “Guidelines for Air and Ground Transportation of Pediatric Patients” in order to provide advice and protocols for children transportation.39 The development of a system, dealing exclusively with the neonatal transportations was mandatory, despite an already existing pediatric or pediatric/neonatal system.40 In 1990, the ΑΑΡ established a separate section, dealing with transportation (Section on Transport Medicine), for the continuous education of health care providers. Scientific meetings were organized, research programs were set up, and guidelines were issued. Furthermore the exchanging of ideas online was also a possibility.41–43
In 1993 the AAP published the “Guidelines for Air and Ground Transport of Neonatal and Pediatric Patients”, where an extensive reference to neonatal transportation was made for the first time.44,45 The latest AAP guidelines were published in 2006 and provided additional references to several issues such as the education of healthcare personnel dealing with transportation, the necessary equipment for optimum transportation and the cost of it. It included advice for the improvement of the provided care. Ethical and legal issues were addressed. Information about research advances was provided, and guidelines on the stressful cases management were given. The support of the patient’s family (family-centered care) was one of the issues discussed and finally standard forms for data collection, necessary for the transportation were provided.41,46 In November 1994, a joint congress for obstetricians, neonatologists and epidemiologists was held in Paris. The heterogeneity in healthcare systems organization as well as the need for collaboration between countries was discussed. For example, in Austria and Belgium NICU provide transfer services, Germany has detailed guidelines for in utero transfer to perinatal centers and both in Spain and Italy, levels of care and indications for transfer differ between regions.47
The concept of EUROPET (European Network Perinatal Transport) was introduced which aimed at assessing different policies among counties, regarding antenatal and postnatal transportation and institutionalization of relative guidelines. Emphasis was placed on the in-utero transportation of high risk pregnancies, as well as the transportation of newborns with gestational age <32 weeks. The project was implemented in 1996 with a European Union Grant (Research Directorate-general (DG 12)-BIOMED II).48 Furthermore, the MOSAIC ('Models of Organising Access to Intensive Care for very preterm births,') project financed by the DG-RESEARCH, European Commission, was designed in order to study the organization of the already existing healthcare services, regarding this highly vulnerable neonatal population group, as well as their outcomes (mainly the extremely preterm infants).49 The results of these studies confirmed the heterogeneity among the European countries on these issues.
What is evident throughout history is that neonatal transportation remains fundamental for perinatal care. Despite the great advances, there is undoubtedly more to be done in this field. The technological improvement is a constant need. The required next generation equipment should combine the minimization of the space needed with the excellence in the provided diagnostic (monitoring) and therapeutic (drug and oxygen administration, temperature/humidity control and correcting) tools. Furthermore, the periodic reorganization of each country’s perinatal healthcare system, based on epidemiological data and medical needs, and the reassurance of a feasible accessibility to it are argued. These are crucial, even among countries, where healthcare system regionalization exists and prenatal risk assessment is a norm, because unexpected and urgent cases could always happen. In addition, the implementation of training programs on both neonatal resuscitation and expertized neonatal transportation, combined with the need for increased healthcare providers awareness and compliance to the issued guidelines should also be included in our future goals. We argue that a combination of the aforementioned issues may continue to reduce the mortality and morbidity rate during neonatal transportation.
Authors would like to thank Mr. Filippos Dellagrammatikas for language editing.
There is no conflict of interest associated with any of the senior author or other coauthors contributed their efforts in this manuscript.
None.

©2015 Mouskou, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.