Journal of
eISSN: 2373-4426


Case Report Volume 5 Issue 7
1Professor, Department of Paediatric Surgery, Urology SDM College of Medical Sciences and Hospital, India
2Associate Professor, Department of Paediatric Surgery, Urology SDM College of Medical Sciences and Hospital, India
3Assistant Professor, Department of Paediatric Surgery, Urology SDM College of Medical Sciences and Hospital, India
Correspondence: Venkatesh M Annigeri MS, MCh, Professor, Department of Paediatric surgery, SDM College of Medical Sciences and Hospital, Sattur, Dharwad, Karnataka, India, Tel 91836-2477802, Fax 91836-2461651
Received: November 19, 2016 | Published: December 6, 2016
Citation: Annigeri VM, Bhuvanesh A, Gadgade BD, Halgeri AB (2016) Giant Retroperitoneal Mature Cystic Teratoma in an Infant: A Case Report. J Pediatr Neonatal Care 5(7): 00212. DOI: 10.15406/jpnc.2016.05.00212
We describe an unusual case of a 6 weeks old male baby, referred to our hospital due to a large mass in his abdomen. Radiological work-up revealed a large retroperitoneal mass. Exploratory laparotomy with tumor resection was performed. Histopathological examination confirmed a mature cystic teratoma. The baby is doing well on follow up.
Keywords: retroperitoneum, teratoma, laparotomy
Teratomas are congenital tumors comprising of tissues, arising from pluripotent embryonic cells. They are frequently seen in gonads. The involvement of extragonadal sites in decreasing order of frequency are anterior mediastinum, retroperitoneum, pre sacrococcygeal areas, pineal and other intracranial sites.1 Retroperitoneal teratoma (RPT) is a very rare germ cell tumors in children and comprises 3.5−4% of all germ cell tumors and 1−11% of primary retroperitoneal neoplasms.2,3
A 6 weeks old male infant, born by normal vaginal delivery at home, presented to our hospital with progressively increasing abdominal mass of 10 days duration, associated with poor feeding. Antenatal care was unsupervised. There was no history of fever, weight loss, bowel or urinary complaints. Post natal period was uneventful. On examination the abdomen was distended, a large firm mass occupying the central and left upper abdomen measuring about 15x 12x10 cm in maximum dimensions. No tenderness on palpation or overlying skin changes. The rest of general examination was unremarkable. Routine blood tests and urine analysis were all within normal limits. The serum levels of alpha-fetoprotein (AFP) was normal. A plain abdominal X-ray showed a well defined round radio-dense mass seen projecting at the left side of the abdomen, mass effect was evident marked displacement of the bowel loops peripherally (Figure 1A). Ultrasound of abdomen showed a large heterogeneous mass located on the left side associated with areas of cystic components. Contrast enhanced computed tomography (CECT) scan of the abdomen and pelvis demonstrates a large retroperitoneal heterogeneous mass occupying predominantly the left suprarenal region, measuring about 12 x 10 x 8 cm with two clumps of calcification, fatty tissue, and cystic contents. The mass crossing the midline was displacing the aorta and Inferior Vena Cava to the contralateral side and the left kidney posterior-inferiorly (Figure 1B&1C). The rest of abdominal and pelvic organs were within normal limits.

Figure 1 Images of computed tomography abdomen and pelvis.
1A CT topographic image showing large left sided abdominal mass displacing the bowel loops with internal calcification.
1B Plain CT axial image showing a large heterogeneous left suprarenal retroperitoneal mass with internal calcification.
1C Contrast CT axial image showing a large heterogeneously enhancing left suprarenal retroperitoneal mass with enhancing soft tissue components and non enhancing cystic and necrotic parts.
1D Contrast CT axial image showing a large heterogeneously enhancing left suprarenal retroperitoneal mass crossing midline, displacing aorta without encasing it. Left kidney is displaced inferiorly and compressed against the posterior abdominal wall.
The baby was planned for surgical excision of the mass. Exploratory transverse laparotomy was performed. On laparotomy a large complex, solid and cystic mass, with well circumscribed smooth border was seen. The pancreas was flattened and stretched over the cranial portion of the tumor (Figure 2A). There was no invasion to the aorta or inferior vena cava. The tumor measured 12 x 10 x 8 cm and weighted 700 gms. Cut section of the mass revealed multilocular cystic spaces, whitish grey wall scattered adipose tissue collection and areas of calcifications. The entire tumor was then excised and sent for histopathological reporting (Figure 2B). Histopathology confirmed the diagnosis of a mature cystic teratoma, benign in nature, with no malignant cells. The final diagnosis was made to be mature cystic teratoma of the retroperitonium. Post operative course was uneventful and baby was discharged on post operative day 8 in good and stable condition. On follow up, baby is doing well with adequate weight gain.
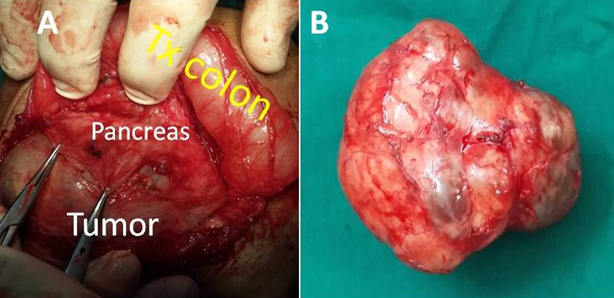
Figure 2 Surgical findings upon laparotomy.
2A On laparotomy a large complex solid and cystic mass with well circumscribed smooth borders. The pancreas is flattened and stretched over the tumor
2B Gross image of the resected tumor showed a large complex solid and cystic mass measuring about 12 x 10 x 8 cm and weighting 700 grams.
Retroperitoneal teratomas are the third most common primary retroperitoneal tumours in the paediatric population after neuroblastroma and Wilms tumour.4 Teratomas arise from germ cells that fail to mature normally in the gonadal locations. These totipotent cells can differentiate into tissue components representing derivatives of mesoderm, ectoderm and endoderm. The distribution of teratomas listed in order of decreasing frequency is: ovaries, testes, anterior mediastinum, retroperitoneal space, pre sacro-coccygeal areas, pineal and other intracranial sites, neck and abdominal viscera other than gonads. The developmental migratory properties of germ cells would explain teratomas in these extragonadal sites, which generally occur along midline structures.5,6 Majority of the tumors are benign, situated on the left side and para renal in location; occasional lesions are bilateral. Occurrence of RPT bimodal, with peaks in the first 6 months of life and in early adulthood. Additionally, the incidence of RPT in females is twice that in males. RPT often remain asymptomatic due to their location, and are usually identified only after they have grown to huge proportions.7 Patients usually present with abdominal distension or a palpable mass like in our case.
Preoperatively, the diagnosis can be established by its characteristic appearance on radiologic evaluation and biochemical study. Radiological manifestations of teratomas are presence of calcification, teeth and fat. Calcification is seen in 50–60% of the cases and is often helpful in making diagnosis preoperatively.8 Diagnosis can be possible with the help of plain radiography, ultrasound abdomen and CECT or magnetic resonance image (MRI) of abdomen. Ultrasound of the abdomen is usually the first imaging modality. CECT or MRI can identify various components of these tumors, including bone, soft-tissue density structures, adipose tissue, and sebaceous and serous-type fluids. These imaging studies can also display the precise location, morphology and adjacent structures of the tumor, which provide better preoperative planning and increased likelihood of complete removal of the tumor with less iatrogenic damage . The main step of therapy for RPT is complete surgical resection and the prognosis for children with RPT depends primarily upon the adequacy of surgical resection. The most important aspect of the excision is to dissect the tumour from renal and other major vessels, which are invariably stretched out over the lesion. Prognosis is generally good and curative if the tumour is completely removed. Unresectable lesions, immature teratomas and endodermal sinus tumours have a comparatively worse prognosis, and may warrant aggressive chemotherapy due to their metastatic nature.4,9 Lastly the single most important factor in prognosis of RPT is complete removal which must be tried in every case of RPT irrespective of its size. The prognosis is excellent for benign RPT if complete resection can be accomplished.
None.
The authors declare no conflict of interest.
None.

©2016 Annigeri, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.