Journal of
eISSN: 2373-4426


Case Report Volume 14 Issue 3
1MS, MCh Pediatric Surgery, Head of the Department, Department of Neonatal and Pediatric Surgery, Santokba Durlabhji Memorial Hospital and Research Institute, India
2Consultant Pediatrician, Department of Neonatology and Pediatrics, Santokba Durlabhji Memorial Hospital and Research Institute, India
3Head of the Department, Department of Neonatology and Pediatrics, Santokba Durlabhji Memorial Hospital and Research Institute, India
4Pediatric Intensivist, Department of Neonatology and Pediatrics, Santokba Durlabhji Memorial Hospital and Research Institute, India
5Junior Resident, Department of Neonatology and Pediatrics, Santokba Durlabhji Memorial Hospital and Research Institute, India
Correspondence: Dr. Sunita Ojha, MS, MCh Pediatric Surgery, Head of the Department, Department of Neonatal and Pediatric Surgery, Santokba Durlabhji Memorial Hospital and Research Institute, Jaipur (Rajasthan), India, Tel 9950595509
Received: October 28, 2024 | Published: December 13, 2024
Citation: Ojha S, Goyal S, Chaturvedi A, et al. Esophageal foreign body in neonates: How do they get it?. J Pediatr Neonatal Care. 2024;14(3):205-210. DOI: 10.15406/jpnc.2024.14.00568
Esophageal foreign body is common in pediatric age group but is rare in neonatal period. A 5-days old newborn presented to us with provisional diagnosis of Esophageal atresia (EA) with or without Tracheo-esophageal fistula (TEF). Child had drooling of saliva and inability to feed. Surprisingly X-ray showed radiopaque shadow in esophagus. Esophagoscopy revealed an impacted stone with a large ulcer. Stone was mobilized by endoscopy but could not be retrieved above cricopharynx due to proximal esophageal oedema. Stone was pushed into stomach and was retrieved by gastrotomy. Literature search from 1955-2022(67 years), identified thirty-nine neonates with wide variety of esophageal FB. Details are discussed with different modalities used for removal of FB and their outcome.
Esophageal Foreign body(FB) more commonly occur in pediatric population from 6 months to 3 years of age due to curiosity and tendency for oral exploration. Although coins are more commonly found esophageal FBs but button batteries, marble stone, pins, nails have also been reported.1 Delay in treatment can lead to complications like perforation, stricture, abscess or death. Early treatment can prevent morbidity and mortality. Respiratory distress with drooling of saliva in newborn is usually considered as esophageal atresia with/without trachea-esophageal fistula (EA/TEF). In a neonate, occurrence of esophageal FB is rare as newborn is on milk-feed and is not picking up, or exploring objects. Diagnosis is difficult to make because of fallacious negative history. Neonatal FBs are usually incidental, due to negligence, sibling curiosity or homicidal.
We discuss here a case of a female neonate who had a large stone impacted in the upper one-third of esophagus along with review of 39 cases of neonates with variety of interesting and unusual esophageal FB found in literature over last 67 years from 1955-2022.
A 3.62 kg, 5 days-old-newborn girl was referred to our tertiary care hospital with complaints of respiratory distress and frothing from mouth for 2 days. The child was apparently well for 3 days after birth. She had respiratory distress, tachypnoea, and chest retraction. She was managed at local hospital, where feeding tube could not be negotiated into stomach and was referred to us for suspected EA/TEF.
On examination, heart rate was 147/min, blood pressure was 75/50 mmHg, and respiratory rate was 52/ min, SPO2 was 97% with oxygen and capillary refilling time was <3 sec. with chest retraction. She had moderately increased secretions from mouth with bilateral conducted sounds. Feeding tube could not be negotiated into stomach. X ray showed coiling of infant feeding tube and large radiopaque shadow in the upper esophagus (Figure 1). Fact that child had accepted feeds well for initially 3 days without any discomfort, raised doubt in it being esophageal atresia. Contrast study was done which revealed large opacity from T2-4and trickling of contrast in stomach ruling out EA and esophageal perforation (Figure 2).

Figure 1 X ray showed coiling of infant feeding tube and large radiopaque shadow in the upper esophagus.
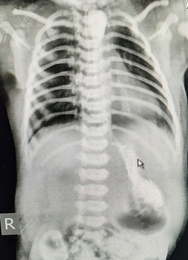
Figure 2 Contrast study showing radiopaque shadow from T2-4and trickling of contrast in stomach ruling out EA and esophageal perforation.
Upper GI endoscopy revealed large impacted stone in upper esophagus with ulcerated mucosa, and surrounding oedema. Stone could not be extracted by flexible endoscope. Under general anesthesia rigid endoscopy was done and impacted FB was mobilized with difficulty but could not be pulled up above the cricopharynx. FB slipped into stomach and was retrieved by gastrotomy. In view of large esophageal ulcer, this gastrotomy was used for tube gastrostomy to feed. Child was fed through gastrostomy tube and was allowed orally on 9th postoperative day after contrast study. Child tolerated feeds well and subsequently gastrostomy was removed. Endoscopy at 2 month showed healed ulcer, mild scars and no stricture. Parents were not aware of FB but had suspicion on 3year old sibling who had tendency to play with toys and mimic feeding them stone.
Eder-Hufford rigid esophagoscope was introduced in 1949. Rigid endoscopy and removal of FB was done by Chevaliar Jackson in 1937.2 Rigid esophagoscopy has been primary tool upto 1957 when Hirchowitz constructed first flexible fibreoptic endoscope.3 Removal of FB by flexible esophagoscope was reported by Mckenhnie in 1972.4 With advent of flexible esophagoscopy, use of rigid endoscopy is significantly less common, but rigid esophagoscopy still plays a role in case of impacted FB not mobilized by flexible endoscopy.
Children are prone to esophageal FB, as they have curiosity and tendency for oral exploration of objects and swallowing almost anything. Most of the FBs pass through the gastrointestinal tract without difficulty but 10-20% require endoscopic removal and about 1% require surgical procedure.1 In neonates usually FB is not expected as the child is neither moving nor picks up the objects. It is either accidental or homicidal. Usual presentation of esophageal FB is difficulty in swallowing, or respiratory discomfort in pediatric age group (6 months to 3 years) but in neonates drooling of saliva with respiratory discomfort is more common presentation that usually leads to misdiagnosis of TEF/EA.
Chest radiograph is the commonest investigation for respiratory discomfort which can reveal FB if it is radiopaque. Radiolucent FB are missed on plain radiograph. Contrast study or CT scan may be helpful in making diagnosis in such cases.
A through literature search from 1955-2022 (67years), with MeSH terms like neonatal, esophageal Children, foreign body, pediatric, oesophageal perforation, was done. Thirty nine neonates with esophageal FB were identified in literature (Table 1).5–28 Diagnosis becomes easier when there is history of FB aspiration but in neonates usually history of FB is not available either because the incident is not witnessed, or it is intentional (homicidal case no 1,2) or accidental (case no 3,4). Definite history of FB was present in two cases only (case no. 5, 6) while allegation was on sibling in three cases (case no. 7, 33 and present case). Parents were unaware of FB’s like dropper caps, pendent, finger ring, ear ring that slipped into child’s mouth and esophagus and came to notice only after the xray (case 3, 4, 6, 16).
Youngest newborn required rigid endoscopy and Portsmouth ET removal from esophagus that had slipped into esophagus and lost while resuscitation immediately after birth (case no. 8-12). Eldest neonate was 28 days of age (case no 13). First case of reported esophageal FB was found in 1960, since then 39 neonates have been reported. Interestingly endotracheal tube (ET) was more common FB in neonates (7cases no. 8-12, 15, 17) (Table 1).
Varieties of FB were found (battery, cotton buds, stone, button, catheter tip, medicine dropper cap, pendent, finger ring, safety pin) (table 1). In two case (no.1, 2) multiple FB were found as it was homicidal intent. Case 18 had slippage of glossoptysis button in bronchus leading to broncho-esophageal fistula after 18 months which ultimately lead to mortality. In an unoperated case of TEF/EA, (case 19) slipped broken end of red rubber catheter in upper pouch was present as FB. Case 1 was posted for thoracotomy considering it TEF/EA. Betel nut was found on esophagotomy as surprise on operating table. Preoperatively feeding tube was coiled up in upper esophagus due to impacted radiolucent bettlenut which was not visualized on radiograph. Out of 39 cases in literature, in 3 cases details about type of foreign body was not found.
|
Sl.No. |
Author (ref) |
Year |
Age/sex |
Foreign body |
Procedure |
Outcome |
|
1 |
Pujar V5 |
2013 |
6days/f |
Bettlenut (Homicidal) |
thoracotomy, |
Recovered |
|
2 |
Medatwal A6 |
2008 |
12days/f |
Multiple FB (total 9) |
FE |
Expired |
|
3 |
Chioukh FZ7 |
2017 |
7days/m |
eyedrop cap |
FE |
Recovered |
|
4 |
Patil8 |
2016 |
5days/m |
Finger ring |
RE, slipped in stomach |
**Recovered |
|
5 |
Nassir GA9 |
2002 |
24days/m |
safety pin |
Magnet/gastrostomy |
Recovered |
|
6 |
Srikant KP10 |
2016 |
4days/m |
dropper cap |
FE |
Recovered |
|
7 |
Entesham HN11 |
2015 |
21days/f |
Marble |
RE |
Recovered |
|
8-12 |
Dickson12 |
1967 |
at birth/m |
Endotracheal tube |
RE |
Recovered |
|
13 |
Syahputra DA13 |
2021 |
28days/m |
Pendent |
FE |
Recovered |
|
14 |
Zlotnikov SA14 |
1960 |
Newborn |
No details |
RE |
Recovered |
|
15 |
Banerjee A15 |
1983 |
Neonate/m |
Endotracheal tube |
RE |
Recovered |
|
16 |
Tasneem Z16 |
2004 |
3days/m |
Finger ring |
RE |
Recovered |
|
17 |
Tasneem Z16 |
2004 |
2days/m |
Endotracheal tube |
RE |
Recovered |
|
18 |
Zunzunegui17 |
1997 |
3days/m |
button for glossoptysis |
Thoracotomy for BEF |
Expired |
|
19 |
Gupta R18 |
2016 |
2days/f |
Broken red rubber |
Retrieved while intubation |
Recovered |
|
20 |
Mohammed Z19 |
2010 |
25days/m |
stone |
FE, oesophagostomy |
Recovered |
|
21 |
Raboei20 |
2009 |
22days/f |
Battery |
RE |
*Recovered |
|
22 |
Singh R21 |
2012 |
12days/f |
Battery |
FE twice |
Recovered |
|
23 |
Altokhais TI22 |
2017 |
5days/m |
No details |
RE |
Recovered |
|
24 |
Chowdhary CR23 |
1992 |
21days/f |
Button |
FE |
Recovered |
|
25 |
Uba AF24 |
2002 |
23days/f |
No details |
FE |
Recovered |
|
26 |
Al Odaidan25 |
2000 |
20days/f |
Thumbtack pin |
FE |
Recovered |
|
27 |
Sharma LK26 |
1993 |
6days/f |
Cotton |
FE, pushed to stomach |
Recovered |
|
28 |
Mirza B27 |
2010 |
2days/m |
Silicon Catheter tip |
direct laryngoscopy |
Recovered |
|
29 |
Kim N28 |
2008 |
7weeks/m |
button |
FE |
Recovered |
|
30 |
Singh H29 |
2012 |
20days/f |
Battery |
RE |
Recovered |
|
31 |
Tarnowska A30 |
2010 |
8days/m |
cotton bud |
FE |
Recovered |
|
32 |
Aggarwal SK31 |
2005 |
4hrs/m |
cotton ball |
FE |
Recovered |
|
33 |
Sardana P32 |
2002 |
20days/m |
Glass piece |
Laryngoscopy |
Recovered |
|
34 |
Pooray33 |
2008 |
27days/f |
Stone |
RE |
Recovered |
|
35 |
Saboo R34 |
2005 |
20days/m |
button with pin |
FE |
Recovered |
|
36 |
Thapa BR35 |
1993 |
6days/f |
stone |
FE |
Recovered |
|
37 |
Dogruyol H36 |
1989 |
4days/m |
Bean |
FE |
Recovered |
|
38 |
Trivella G37 |
1962 |
Newborn |
No details |
RE |
Recovered |
|
39 |
LI ZS38 |
2006 |
24hrs/m |
ear ring |
FE |
Recovered |
|
40 |
Ojha S (present) |
2022 |
5days/f |
stone |
FE,RE, gastrostomy |
Recovered |
Table 1 cases of Neonatal esophageal foreign body
RE: Rigid Endoscopy
FE: Flexible Endoscopy
BEF: Broncho-esophageal Fistula
* developed stricture, required dilatation for 1 year
** required Chest tube for pneumothorax
Chart 1 depicts various procedures done for retrieval of foreign body. Flexible and/or rigid endoscopy was attempted in all cases. FB was removed by flexible endoscopy alone in 17 cases, rigid endoscopy in 15, laryngoscopy in 2 and surgery was required in 5 cases (including present case) esophagostomy, thoracotomy, broncho-esophageal fistula repair and gastrostomy (Table 1, chart 1) (Case no. 1, 5, 18, 20, present case).29–38
Out of 40 neonates (39 cases in literature and 1 present case), 38 recovered while 2 expired, one due to broncho-esophageal fistula (case 18) and one had multiple FBs (case 2, total of 9 FB including coin, safety pin, screw, polythene, glass piece). Out of 38 that recovered, one had pneumothorax that improved with chest tube insertion (case 4) while one developed stricture that required dilatation for about one year (case 21).
Various techniques like flexible endoscopy, rigid endoscopy, magnet, foley’s catheter, pushing the FB into stomach, gastrotomy, esophagotomy and thoracotomy have been done depending upon the situation (condition of child, esophagus, availability of equipments). Based on these procedures done for FB removal in neonates, suggested procedures/options are depicted in chart 2.
Parents should be warned about use of eye dropper cap, small jewelry like rings, as it can fall accidentally in neonate’s mouth. Newborn child should not be left unsupervised with a young sibling.
Incidents where history is doubtful and homicidal/intentional FB is suspected, child abuse/neglect should be thought of and should be informed to Child Right Commission or Human Right Organization.39
Esophageal FB although rare in newborn, is often missed in case of radiolucent FB due to absence of history. Usually, newborn get FB by incident, accident, siblings or intentional (homicidal). FB can be anything like slipped catheter tip, rings, pin, stone or medicine dropper cap. Parents should be cautioned about rings, dropper caps, safety pins of napkins while handling newborns.
Esophageal FB should be suspected where history is doubtful or not clear, in cases of sudden onset of drooling of saliva, or difficulty in swallowing, bleeding from oral cavity in a newborn who had been otherwise feeding well before this incident (thereby ruling out oesophageal atresia) or history of throat suctioning, or sibling playing with newborn, or newborn left unattended just before the incident.
Delay in diagnosis can lead to complications like perforation, stricture, abscess, broncho-pleural fistula and even mortality. An early diagnosis and appropriate treatment can prevent morbidity and mortality.
We acknowledge contribution of Ms Arpita Chippa, Jophy Jose, and Sourav Lohan in technical support for manuscript.
Ethics committee approval and consent was taken. Approval was granted by SDMH ethics committee.
Not applicable.
None.
Author declares that there is no competing interest.

©2024 Ojha, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.