Journal of
eISSN: 2373-4426


Case Report Volume 8 Issue 5
Department of Pediatric Surgery,V.M.M.C & Safdarjang Hospital, India
Correspondence: Rajat Piplani, MCh. Pediatric Surgery, Senior Research Associate, Department of Pediatric Surgery, V.M.M.C & Safdarjang Hospital, New Delhi-110029, India, Tel 91 9971158129
Received: March 10, 2018 | Published: September 12, 2018
Citation: Piplani R, Acharya SK, Bagga D. Superior mesenteric artery syndrome (Wilkie’s syndrome): acute severe presentation in a 10 year old boy and role of early surgical management. J Pediatr Neonatal Care. 2018;8(5):211-212. DOI: 10.15406/jpnc.2018.08.00342
Superior mesenteric artery (SMA) syndrome is a rare cause of upper gastro intestinal (GI) obstruction in paediatric age group. It is an uncommon disorder that mostly occurs due to loss of retroperitoneal fatty tissue secondary to various debilitating conditions. SMA syndrome occurs when acute angulations of the superior mesenteric artery cause compression over the third part of duodenum between the SMA and aorta. We report this rare case of a 10 year old boy who presented with acute onset of epigastric pain and recurrent bilious vomiting. Based on radiological investigations, a diagnosis of SMA syndrome was made. A conservative trial was initiated but symptoms persisted. Hence, he underwent midline laparotomy and duodenojejunostomy. The postoperative period was uneventful and patient is asymptomatic on one year follow up.
Keywords: Superior mesenteric artery syndrome, Wilkie’s syndrome, Intestinal obstruction, Surgery.
Superior mesenteric artery syndrome is an atypical condition which was first described in 1861 by von Rokitansky.1 It is an unusual form of upper GI obstruction, also synonymous with Wilkie’s syndrome or cast syndrome or arteriomesenteric duodenal compression or chronic duodenal ileus which occurs due to compression of the third part of duodenum between abdominal aorta posteriorly and superior mesenteric artery anteriorly.2,3 It is mostly due to loss of retroperitoneal fat that normally acts as cushion around the SMA. Patient usually presents with chronic intermittent pain abdomen, bilious vomiting, nausea, early satiety and anorexia. A history of weight loss is usually seen but it is not a necessity.3 The diagnosis is basically by exclusion of other causes of upper GI obstruction and confirmed by upper gastrointestinal contrast study and contrast enhanced CT abdomen. A trial of initial conservative management can be given to all patients but surgical intervention in the form of duodenojejunostomy gives early and complete relief of the symptoms.
A 10 year old male chid presented with epigastric pain which relieves on vomiting for 10 days. There was a history of significant weight loss of the child secondary to fever of unknown origin over a month. On examination, pallor and visible gastric peristalsis were noted. Ultra sonography of the abdomen was normal. Contrast enhanced computed tomography (CECT) abdomen (Figure 1) (Figure 2) was suggestive of SMA syndrome with dilated proximal half of third part of duodenum and narrow aortomesenteric angle (<110) along with smaller aortomesenteric distance (<5mm). A conservative trial was attempted with nasogastric decompression, IV fluids, total parenteral nutrition and lying on left side or prone position, but proved to be ineffective as the symptoms persisted. Hence, exploratory laparotomy was planned after one week which confirmed the obstruction at the level of third part of duodenum with grossly dilated stomach and proximal duodenum above the level of origin of SMA from aorta and collapsed distal bowel (Figure 3). A side to side retrocolic duodenojejunostomy bypass was done. Postoperative period was uneventful. Oral feeds were started on 6th postoperative day and the patient was discharged on full feeds on 8th postoperative day. The child is asymptomatic and has gained weight on one year follow up.
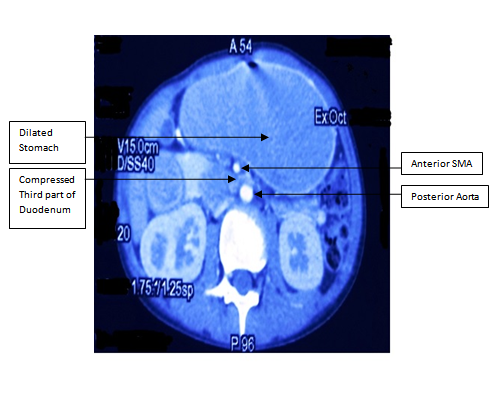
Figure 1 CECT Abdomen (axial view) showing dilated stomach and proximal duodenum along with compressed third part of duodenum between aorta posteriorly and SMA anteriorly.
SMA syndrome was first described by von Rokitansky in 1861 as an autopsy finding.1 Further, Wilkie published a detailed anatomical and pathophysiological description of this rare cause of upper GI obstruction in 1927.2 It is due to the obstruction of third part of duodenum between the SMA anteriorly and the aorta posteriorly.3 It is an uncommon entity with an incidence of about 0.013-0.3% in literature.4,5 This syndrome is more common in females and occurs usually in older children and teenagers. It is generally associated with history of acute weight loss in majority of the patients leading to loss of fatty cushion around SMA secondary to various catabolic states like burns, eating disorders, chronic illness, neoplastic diseases and malabsorbtive states.6,7 However, other causes include an abnormally high insertion of the ligament of Treitz, abnormally low insertion of the SMA, following corrective spinal surgery or spinal trauma.#ref77 Patients usually present with classic symptoms of upper GI obstruction like nausea, vomiting of bilious or partially digested food particles, early satiety, eructations and recurrent epigastric pain and fullness. The presentation can be chronic, intermittent or acute as result of partial or complete duodenal obstruction.5-9 These symptoms are generally relieved on lying prone or left lateral decubitus position and gets aggravated in supine position. The diagnosis of SMA syndrome is based on clinical symptoms and further substantiated on radiological findings. Upper GI dye study will reveal a dilated stomach and duodenum till second part and cut off at the third part of duodenum with no mucosal irregularity.
Contrast enhanced computed tomography (CECT) abdomen and Magnetic resonance angiography (MRA) are useful diagnostic investigations and provide better visualisation of a narrow a aortomesenteric angle between 6-250 (normal angle between 38-560) and reduced aortomesenteric distance between 2-8mm (normal 10-20mm) associated with this condition.6 Initial conservative management includes nasogastric decompression, intravenous fluid and electrolyte correction, promotility agents like metoclopramide, prone or left lateral position, surgically inserted nasojejunal feeding tube, or peripherally inserted central catheter for total parenteral nutrition administration should be given as a trial.4 Some patients respond to this conservative management and their symptoms gradually improves after weight restoration. However in patients with severe symptoms and not responding to initial conservative management as in our case surgical intervention should be planned.8 Duodenojejunostomy, the most common operation for SMA syndrome, was first proposed by Blood good in 1907.5 Other surgical options include gastrojejunostomy, Roux en Y duodenojejunostomy, anterior transposition of the third part of duodenum and division of the ligament of Treitz with mobilisation of the duodenum.6-8 The use of laparoscopic surgery in mobilisation of duodenum and lysis of the ligament of Treitz has also been reported.9,10 Surgery in SMA syndrome has an advantage over conservative management in severe cases as it gives immediate and complete relief of the symptoms and allows early weight gain in these patients. It also reduces the chances of potential delayed complications viz. electrolyte imbalances, aspiration pneumonia, catabolic wasting, acute gastric perforation and peritonitis in chronic recurrent cases.
Superior mesenteric artery syndrome is a rare condition that can present in an emergency with acute upper gastrointestinal obstruction. It usually presents in older children with history of significant weight loss in majority of the patients. A trial of conservative management should be given to all patients. However, if the initial conservative treatment fails, one should not delay surgical intervention so as to prevent further fatal complications. Duodenojejunostomy is the procedure of choice and is highly effective in managing acute severe form of SMA syndrome.
None
The author declares there is no conflict of interest.

©2018 Piplani, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.