Journal of
eISSN: 2373-6445


Research Article Volume 14 Issue 4
1Pediatrician, UCB/HMIB/UniCeub, Brazil
2Physical Education, Catholic University of Brasilia, Brazil
3Nursing, UFPE: Universidade Federal de Pernambuco, Brazil
4Psychology, UniCeub, Brazil
5Psychology, UCB, Brazil and University of Wales Trinity Saint David, UK
Correspondence: Marta Helena de Freitas, Psychology, Catholic University of Brasilia, Brazil, University of Wales Trinity Saint David, UK
Received: June 27, 2023 | Published: July 11, 2023
Citation: Leal MM, de Melo GF, Gomes E, et al. Relationship between perceived stress and religious/spiritual coping in pregnant women with malformed foetus. J Psychol Clin Psychiatry. 2023;14(4):95-100. DOI: 10.15406/jpcpy.2023.14.00736
Congenital Foetal Malformity (CFM) is a stress factor for pregnant women, and religiosity and spirituality have an important role to play in coping with it. The aim of this study was to identify the correlation between stress, as perceived by pregnant women with CFM, and the diverse forms of religious/spiritual coping (RSC). This is a cross-sectional study with pregnant women treated in a hospital specializing in obstetrics in the city of Brasília, located in the Federal District in Brazil. The sample comprised 99 expectant mothers. Religious/spiritual coping was measured using the RCOPE scale devised by Pargament, Koenig and Perez (2000) which was subsequently translated into Portuguese and adapted for Brazil by Panzini and Bandeira. Stress was evaluated using the Perceived Stress Scale of Cohen, Kamarck and Mermelstein (1983), translated and validated by Luft et al. (2007). For the purposes of analysis, the SPSS-IBM 22.0 software application was employed, with a statistical analysis using means, standard deviations and frequencies, along with the Chi-Squared (elevated power of sample – 0.77) and Logistical Regression tests aimed at evaluating the relationship between perceived stress and the type of RSC. The results indicated that 92.8% of pregnant women with CFM presented with positive religious/spiritual coping (PRSC), with a mean value for perceived stress of 41.17 ± 9.03, there being an inverse relationship between perceived stress and PRSC (p = 0.02). Just five of the pregnant women presented with higher levels of stress and negative religious/spiritual coping (NRSC), without any correlation with demographic data (expectant mother’s age, religion, income, schooling, CFM prognosis or time since diagnosis). It was found that 81 (81.8%) of the pregnant women would like this topic to be addressed in the hospital setting, primarily by the doctors (56.6%) treating them.
Keywords: religious coping, pregnancy, stress, religion, spirituality
Pregnancy is a time of intense physiological and anatomical change,1,2 which is directly related to psychological and emotional aspects of women.3 During pregnancy, women tend to undergo psycho-affective restructuring with the aim of assimilating the new reality and opening up to the possibility of motherhood, which will enable interaction between mother and baby.4 Various studies5, 3 have shown that, in this stage of life, women present with a composite psychodynamic, which may be accompanied by affective regression, pronounced narcissism and the capacity to indulge in fantasy. Although such psychological phenomena tend to be normal and to be experienced by all pregnant women, they could potentially take on a pathological character.5–7 As part of this process, pregnant women tend to build up an idealized notion of their babies, creating a series of expectations with regard to the child, and for themselves as mothers-to-be.8,9 According to contributions deriving from psychoanalysis, depending on the psychic organization of this future mother, this idealized baby could embody characteristics of omnipotence and perfection.8,9 Thus, representing the renaissance of the maternal narcissism, it may be expected as a being immune to disease and death, and possessing the capacity to realize the dreams which they, the women, or the children’s fathers never achieved.9 So, depending on the degree and the rigidity of this natural idealization mechanism, a diagnosis of foetal malformation could end up being intolerable for this mother-to-be, producing conditions that affect her mental health, such as anxiety and depression.10,11
A foetal malformation is defined physiologically as a “morphological defect of an organ, part of an organ or larger area of the body, resulting from a process of intrinsically abnormal development.”12 This diagnosis generates stress in the expectant mother, which could be even more accentuated when experienced as an unsustainable threat to her narcissism, eroding her expectations of the imaginary baby. Conversely, in cases of lethal pathologies, the grief experienced by these women goes beyond the loss of the imaginary baby, characterized by the loss of the real baby.13 In these situations, the stress, built on the basis of a relationship between the individual and her environment,14 ceases to be a merely organic reaction and assumes a psychological component. Accordingly, based on the perception of the individual with regard to the situation and the analysis she makes thereof, the stress is also related to the way she experiences it at the psychological level, to how much she can or cannot bear it emotionally, and/or the extent to which she feels, or does not feel, she is actually capable of dealing with it.15 This is evident, for example, in a study conducted on women in the second trimester of pregnancy, who demonstrated a high level of psychological stress and depression on receiving the diagnosis of foetal malformation, but with a diminishing tendency as the gestation progresses.16
Other studies have shown that stress affects the life of the individual and is also related to the way in which the individual deals with the stressor, in this case the foetal malformation.17 Accordingly, one of the dimensions that interferes with the life of the expectant mother with a diagnosis of CFM and the level of stress she experiences, is that which, in the area of cognitive psychology, is termed coping: “A set of strategies used by people to adapt to adverse circumstances. The efforts expended by individuals in dealing with stressful, degenerative or acute situations”.18 In fact, in studies involving pregnant women with malformed babies, a variety of strategies can be observed, ranging from those focusing on the problem itself (foetal malformation), to the emotions related to it experienced by the mothers-to-be.15,17,19,20 Several articles have also reported a style of coping that focuses on religiosity and/or spirituality,10,21 a style which is the one most employed by expectant mothers in Brazil, according to Brazilian studies on this topic.10,22
In Brazil, 92% of the population tend to refer to themselves as religious,23 involving a variety of different religions, though predominantly connected to Christianity. Religious/spiritual coping (RSC), which consists of employing religious/spiritual beliefs and behaviours to deal with, prevent or alleviate life’s diverse problems and their material or emotional consequences,24,25 is described in the pertinent literature25–27 as being positive or negative in nature. Positive religious/spiritual coping (PRSC) is characterized by the seeking of spiritual support, aimed at resolving problems with the help of God and/or redefining the stressor in benevolent fashion, having positive impacts on the stress coping process. Negative religious/spiritual coping (NRSC), on the other hand, has a prejudicial effect on the individual and tends to go hand in hand with a denial of reality and/or a questioning of existence, love or the actions of God.24,25
Bearing in mind the specifics of Brazilian reality, as well as the relevance of religious coping in the hospital setting, particularly in cases of expectant mothers receiving a diagnosis of foetal malformation, the aim of this study was to identify the correlation between stress, as perceived by the pregnant women with CFM, and the different forms of RSC. In addition, the study sought to verify the role of clinical and demographic variables in this process.
This study was submitted to and approved by the Ethics Committee of the Department of Health in the Federal District of Brasília, under CAAE reference 15068919.9.0000.5553, and approved under opinion no. 3.585.731. It is a cross-sectional study conducted in the Foetal Medicine Outpatient Clinic at the Mother & Child Hospital in Brasília (HMIB). As CFM is a complex diagnosis involving many emotional aspects, this service boasts a multidisciplinary team including a psychologist and psychiatrist to attend to these expectant mothers. This outpatient clinic takes place on Tuesday mornings and on two Saturdays each month. During the period of two years in which the data collection was performed, a total of 228 pregnant women with a diagnosis of foetal malformation were seen, of whom only 119 were approached to take part in the study. The study inclusion criteria comprised all those who had had at least one consultation in the area during the period of the study, while the exclusion criteria were: a) those who were functionally illiterate and/or unable to answer the questionnaire, or; b) those who did not agree to take part in the study, and c) those who failed to fully answer the questionnaires.
The study instruments employed were: a) Sociodemographic questionnaire consisting of 15 questions; b) perceived stress scale devised by Cohen, Kamarck and Mermelstein,28 translated and validated by Luft et al.,29 (Cronbach’s alpha of 0.82); c) the complete RCOPE scale elaborated by Pargament27 translated and validated in Brazil by Panzini and Bandeira.25 The items on the scale fall into two groups: PRSC, with 8 factors (Cronbach’s alpha of 0.98); and NRSC, with 4 factors (Cronbach’s alpha of 0.86).25
The data were collected in the waiting room in the outpatient clinic, the calmest and most private location available in the building. Still, the expectant mothers were not left alone to fill in the questionnaires. Their companions and the other patients were all seated in this location. All the pregnant women were approached by the principal researcher who explained to them the purpose of the study and asked them to sign an informed consent form (ICF). They read the questionnaire and responded without any interference from the researcher. The patients had to hand back the questionnaire the same day. They began to answer it prior to entering the consulting room and were able to complete it once the consultation was over.
Means, standard deviations and frequencies were employed in the analysis of the descriptive data. To evaluate associations between the variables, the Chi-Squared and Logistical Regression tests were applied. For all analyses, a level of significance of p ≤ 0.05 was applied. All data were analysed using version 22.0 of the SPSS-IBM software application.
Table 1 displays the sociodemographic distribution of the participants. The mean age of the pregnant women investigated was 29.36 ± 7.32 years (17 to 46) and the mean gestational age on diagnosis was 18.2 ± 5.7 weeks, ranging from 6 to 35 weeks.
Variable |
Category |
Frequency |
Percentage (%) |
Age Range |
Up to 34 years |
72 |
72.7 |
Over 35 years |
27 |
27.3 |
|
Marital Status |
Single |
55 |
55.6 |
Married |
42 |
42.4 |
|
Widow |
1 |
1.0 |
|
Did not respond |
1 |
1.0 |
|
Residence |
No response |
3 |
3.0 |
Brasilia City Centre |
9 |
9.1 |
|
Satellite Town |
65 |
65.7 |
|
Surrounding Area |
14 |
14.1 |
|
Other states |
8 |
8.1 |
|
Schooling |
Incomplete Elementary |
6 |
6.1 |
Completed Elementary |
4 |
4.0 |
|
Incomplete Secondary |
9 |
9.1 |
|
Completed Secondary |
38 |
38.4 |
|
Incomplete Higher Education |
12 |
12.1 |
|
Completed Higher Education |
17 |
17.2 |
|
Postgraduate |
13 |
13.1 |
|
Income |
Up to R$ 1,000 |
39 |
39.4 |
From R$ 1,001 to R$ 3,000 |
45 |
45.5 |
|
Over R$ 3,000 |
15 |
15.1 |
|
Left her job? |
Yes |
15 |
15.2 |
No |
84 |
84.8 |
|
Religion |
No religion |
7 |
7.1 |
Catholic |
50 |
50.5 |
|
Evangelical |
35 |
35.4 |
|
Candomblé |
2 |
2.0 |
|
Christian |
5 |
5.0 |
Table 1 Descriptive data of sample
Table 2 exhibits the relationship between perceived stress and the forms of RSC, positive or negative. The sample produced a mean value for perceived stress of 41.17 ± 9.03 (21 – 61). As the scale does not establish levels of stress, we chose to compute it through the quartiles of the sample itself, in which the cutoff for light stress levels was 35; moderate went from 35.1 to 47.99; and high stress levels began at 48 points.
Religious coping |
Perceived stress |
|||
Low |
Moderate |
High |
Total |
|
Positive |
27 (29.3%) |
43 (46.7%) |
22 (23.9%) |
92 (100%) |
Negative |
0 (0.0%) |
2 (28.6%) |
5 (71.4%) |
7 (100%) |
Total |
27 |
45 |
27 |
99 |
Table 2 Relationship between stress levels and religious coping
*p = 0.02.
As illustrated in Table 2, pregnant women with NRSC presented with levels of perceived stress ranging from moderate to high, predominantly the latter. None of them exhibited low levels of stress. Meanwhile, pregnant women with PRSC demonstrated an equilibrium of intensity of perceived stress, scoring moderate in almost half of these cases. A calculation was performed of the delta of the period elapsing between gestational age when the foetal malformation was communicated to the expectant mother and the gestational age when the interview was conducted, classifying the result into three categories: low (1-5 weeks), moderate (6-13 weeks) and high (14 weeks and above). The end result is shown in Graph 1, noting the delta between the diagnosis and the collection of data in the questionnaire. Graph 2 illustrates the gestational age when the foetal malformation was diagnosed, divided into three groups, each representing three months of gestation, (observing the standards used in the disciplines of gynaecology and obstetrics). Graph 3 shows the distribution in relation to the diagnosis of foetal malformation.
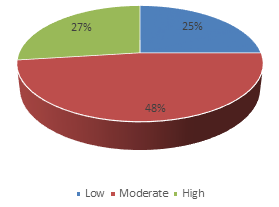
Graph 1 Distribution of pregnant women according to time elapsed between current gestational age and gestational age at the time of the diagnosis.
Through the use of logistic regression, and using RSC as the dependent variable and epidemiological factors as the independent variables, the model did not present significance (p = 0.33). The values for each independent variable were as follows: Age (p = 0.83), schooling (p = 0.61), income (p = 0.12), marital status (p = 0.69), age of diagnosis by trimester (p = 0.60) and classification of malformations with regard to the prognosis (p = 0.06). Thus, the inference was that these variables did not exert an influence on the intensity of the stress in those who demonstrated a higher rate of negative coping.
As far as religiosity and spirituality are concerned, the expectant mothers were asked if they would like the aforementioned topic to be addressed by the team. It was found that 81.8% (81) of pregnant women stated they would like the topic to be broached in their appointments. They stated that doctors were the preferred professionals for addressing the topic in question (56.6%), followed by nursing staff (31.3%) and technicians (24.2%).
In line with the literature10,16,30 this study demonstrated that a diagnosis of foetal malformation causes stress in women, not just physically but also psychologically. In the qualitative study conducted by Cristofalo et al.,31 involving 35 pregnant women with foetuses presenting with a choroid plexus cyst, 88% of women stated that the immediate reaction to the diagnosis was profoundly negative, corroborating the findings in the present study.
By employing a perceived stress scale to evaluate how a diagnosis of foetal malformation might affect expectant mothers, a value was observed close to the mean (41.17 ± 9.03) of the parameters established by the scale (21 – 61), but no comparison was made between perceived stress among pregnant women with CFM and those without such a diagnosis, as was carried out in the study of Kaasen et al., for example.16 In their studies, the authors noted that pregnant women initially suffered from high levels of stress but that this subsided towards the end of the pregnancy, when the levels were virtually the same as in pregnant women without foetal changes. The present study, being cross-sectional in nature, only found that the prognosis of malformation was not a stress factor.16
In the bibliographical review conducted for this study, no studies were found which used the perceived stress scale in pregnant women with CFM, however studies were found with high-risk pregnant women. A study developed in Jordan32 (218 patients) used the same scale but with just 10 items and, after proportion conversion, the mean value obtained for perceived stress in said study was 37.92 ± 9.2, a degree of stress similar to the results in the present study. In another study, conducted in Ethiopia33 with 396 patients, the mean value for perceived stress was 49.5 ± 48, a value somewhat higher than in the present sample.
The present study uniquely investigated the form of coping relating to religiosity and spirituality, insofar as, in both national and international studies, faith and religion were the principal forms of comfort used following a diagnosis of CFM.10,11 The results show that the majority of pregnant women (92.2%) presented with PRSC and just 7.8% with NRSC. The present study differs from that of Martins et al.,34 conducted on 28 pregnant women diagnosed with CFM. The researchers applied the 3-Factor model of the Coping Based on Problems Scale (CBPS) used for this study. The CBPS scale is an adapted version of the Ways of Coping Checklist developed by Folkman and Lazarus, in which religious coping is not characterized as negative or positive, but rather as favourable or unfavourable, and in which the majority presented with unfavourable coping (17 expectant mothers).34
In the study by Nunes and Abrahão,19 in which 120 Brazilian pregnant women diagnosed with CFM took part, religious coping was heavily used by women and was identified as a positive way to reevaluate CFM, giving positive meaning to the situation experienced, focusing on personal growth that this disease promoted in the family. This outcome is in harmony with the present study. In other words, in positive religious/spiritual coping (PRSC), religiosity and spirituality are lived by the individual to be something welcoming, a succour in situations of suffering or sickness. PRSC is represented by a search for spiritual support, resolving problems involving collaboration with God, redefining the stressor in a benevolent manner.24,25
Even though several studies have acknowledged the beneficial role of religion and spirituality, they also tended to highlight the negative aspects, particularly when presented as a way to deny reality, characterizing an NRSC, which was found to be extremely low (7%) in this study. Nunes and Abrahão,19 in their study, noted that in a minority of the sample, religiosity and spirituality are used as a form of escape/avoidance response, desires and actions to flee from or deny the problem. The study conducted in Sweden by Carlsson,1 focusing on an analysis of 18 online posts, evaluated coping and the process of grief of pregnant women with foetal malformations. In conversations with family members, one of the coping styles identified was to distance oneself from the diagnosis, with the desire for a miracle being cited as a form of NRSC.
Borges and Petean22 report that most pregnant women present with stress and use RSC, however, they understood that religiosity and spirituality were a negative way of coping, i.e., NRSC. In their study comprising 33 Brazilian pregnant women, they found that 45.5% of women presented with clinical indications of anxiety and 30.3% depression, the primary coping strategy focusing on religious practice and fanciful thinking (51.5%). The authors report that “religion may be as much a protective factor as a risk factor, preventing the expectant mother from ‘seeing’ reality, wherein the expectation of a magical solution may be present, impairing decisions which need to be taken.”22
The present study investigated RSC by way of an instrument translated and validated for use in the Brazilian setting,25,27 enabling the identification of results diverging from those found in the abovementioned studies, which investigated coping in women with CFM in a general sense and identified religiosity and spirituality as the main form of coping. The principal discrepancy between these studies and the one presented here is that, in the present study, 92% of pregnant women presented with PRSC, related to a reduction in the perceived stress of expectant mothers (p:0.02). In the study by Piccinini et al.,35 however, positive coping was not identified as being protective or as a driver of the mental health of the expectant mothers. This discrepancy between results may be ascribed to the failure to apply the proper instruments to evaluate RSC in all its profundity and also to the small sample size in the quoted studies. Another explanation may lie in the fact that the majority of the studies conducted, by using scales, originate in the positivist paradigms that guide the sciences, in which they simply consider religion and spirituality to be defence mechanisms, generally associated with a rational form of denial of reality.36
The negative component of RSC exists but, in the population studied herein, only 7 (7%) expectant mothers presented with NRSC and, of these, only 5 (5%) presented with high levels of stress. In the study conducted by Piccinini et al.,35 it was observed that NRSC was associated with changes in mental health, such as depression and anxiety. However, the sample is made up of pregnant women in general, without specifying whether or not they had a diagnosis of CFM. In the present sample, it was not possible to draw this parallel. A scale to evaluate the mental health of expectant mothers was not applied and they did not state if any of them suffered from any of these disorders. However, considering that pregnant women with NRSC presented with high rates of perceived stress, it cannot be inferred that the pregnant women in the study suffer from any mental health impairment.
A further relevant piece of information is that it was not possible to predict which patient will have NRSC, seeing that no clinical/epidemiological variable (age group, schooling, religion, marital status, difference in timing between the diagnosis and the collection of the data and the prognosis of malformation) was sufficiently statistically significant to identify which women these would be. These data suggest that, only when approaching religiosity and spirituality with these patients, personally and in a more profound manner, will it be possible to identify the nature of their respective RSC strategies.
This study also showed that addressing religiosity and spirituality is the wish of the majority of the pregnant women who took part in the study and, in their perception, the doctors are the professionals who should be leading the conversation. However, for this wish to materialize, it will still be necessary to develop a training and review of the paradigms by health professionals in Brazil. Lucchetti et al.,37 in their study involving 3,630 medical students in public and private universities in the various federal states of Brazil, found that 81% stated they had never received “spirituality and health” training during graduation, 61.6% believed that they should receive preparation to address spirituality with their patients and 83.4% noted that medical schools in Brazil were not providing adequate training in this area. On the other hand, 62.2% of students believed that health and spirituality content should be included in the medical curriculum37. In other words, it appears that the vast majority of students are receptive to this training and revision of paradigms.
The results of this study added more elements in the sense of evidencing the importance of religiosity and spirituality in the coping of pregnant women with foetal malformation as well as reiterating that positive RSC was the most prevalent, also serving as a protective factor for stress in these women. Another important aspect to highlight is that the presence of negative RSC, and also the high level of stress, do not indicate significant correlation with any item of clinical or epidemiological data. Accordingly, in order to identify the nature of NRSC, as well as the nature of the concomitant stress, it is necessary for health professionals to address religiosity and spirituality and to understand the way in which these topics are manifested in the lives of each individual, particularly during the gestation of a baby with foetal malformation.
Indeed, this approach is desired by the expectant mothers participating in the study, who emphasize the prominent role of the doctors in this process. As a direct implication of these findings, we see the need for these topics to be included throughout the education of health professionals, providing them with adequate training in the clinical management of religious coping and their relationship with the physical and mental health of these pregnant women at such a delicate moment in their lives.
Special thanks to the Professinals who integrate the Fetal Medicine Outpatient Clinic at the Mother& Child Hospital in Brasilia (HMIB).
There is no conflicts of interest.

©2023 Leal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.