Journal of
eISSN: 2373-6445


Research Article Volume 6 Issue 6
1Montreal Mental Health University Institute Research Centre, Canada
2Psychiatry Department, University of Montreal, Canada
Correspondence:
Received: October 01, 2016 | Published: December 20, 2016
Citation: Blais MT, Bodryzlova Y, Aardema F, O’Connor K (2016) Open Trial of Inference-Based Therapy in the Treatment of Compulsive Hoarding. J Psychol Clin Psychiatry 6(6): 00403. DOI: DOI: 10.15406/jpcpy.2016.06.00403
Background and aims: Non-pharmaceutic approaches to the treatment of hoarding disorder (HD) use interventions based of cognitive-behavioral therapy (CBT). Inference-based therapy (IBT) focuses on the doubts which form the basis of preoccupation in HD and deals with ego syntonic values in hoarding by exposing how the hoarding-self sabotages the authentic self. The objective was to establish if the IBT would lead to the clinically significant decrease of hoarding symptoms.
Methods: 18 participants (17 completers) received 20 –weeks of IBT therapy. Hoarding was assessed in pre-treatment, post-treatment and at 6-month follow-up with the Vancouver Obsessional Compulsive Inventory Hoarding Subscale (VOCI-H) (n=14) and the Savings Inventory Revised (SI-R) (n=7). A general linear model for paired observations was used to assess treatment effect. The participants were divided into OCD -/+ according to a clinical diagnosis on the SCID-I and the VOCI-H scores were compared between the two groups.
Results: Twelve of 14 completers where outcome was measured in VOCI-H (86%; CI 67%-100%) showed positive changes in hoarding; four crossed the threshold for clinically significant changes (28%, CI 5%-55%); all of them maintained the gain at follow-up. Three of 9 participants at follow-up crossed over the threshold to non-clinical status (33%, CI 3%-64%) (VOCI-H=6); six of nine participants (66%, CI 35%-97%) had positive changes in hoarding between baseline and 6-month follow-up. There were no differences in outcome on hoarding in participants classified by severe or moderate OC
Discussion: The IBT showed significant diminution of hoarding symptoms in the range previously reported for CBT.The cognitive aspects of IBT add new dimensions to existing CBT approaches.
Keywords:hoarding, inference-based therapy, cognitive behavioral therapy, open trial
Hoarding disorder (HD) is increasingly recognised as a serious psychiatric problem1‒3 despite being highly mediatised 4,5 is a relatively new6,7 diagnostic entity. Diagnostic and statistical manual of mental disorders (DSM-58) has recognized HD as a distinct disorder within the Obsessive Compulsive and Related Disorders category, and defined as a persistent difficulty discarding or parting with possessions, regardless of the value others may attribute to them, and a difficulty to get rid of unnecessary objects and an excessive acquisition result in clutter.
Previously HD was considered as an Obsessive compulsive personality trait or as a variant of Compulsive Obsessive Disorder (OCD); so, initially, evaluation tools and treatment approaches used in OCD were applied to the HD population. Nonetheless, new HC-specific evaluation tools have been developed.9‒12 However, current treatment approaches to HD overlap with OCD treatment practices in the clinical management of HD.
Pharmaceutical treatment
Selective serotonin reuptake inhibitors,13‒16 Serotonin–nor epinephrine reuptake inhibitors 17, Central nervous system stimulants18 and atypical antipsychotic agents19 have been administered for HD, but results from pharmaceutical treatment trials for hoarding are equivocal.
Cognitive-behavioral therapy
Frost & Hartl20 described a cognitive-behavioral model of HD in 1994, which highlights information processing deficits; problems in forming emotional attachments; behavioral avoidance and erroneous beliefs about the nature of possessions. Cognitive-behavioral therapy (CBT) in individual psychotherapy is widely used for HD treatment.21 In an open trial conducted by Tolin et al.,22 60% patients met criteria for clinically significant change on the Savings Inventory-Revised scale after 26 individual sessions of CBT. Await list-controlled 26-week trial23 treatment included CBT case formulation, motivational interviewing, skills training for organizing and problem-solving, direct exposure to non-acquiring and discarding, and cognitive therapy. The intervention showed a nearly 10-point (15%) average reduction in total SI-R scores in the CBT group and an insignificant reduction in the wait-list group. Short-term (12weeks) CBT therapy has reduced HD symptoms in 30% of the sample.24 In geriatric patients, however, CBT did not demonstrate any significant effect.25 Jónssonet & Haugaard26 compared group and individual CBT in patients with OCD including participants with HD. The meta-analysis showed overall large (Cohen’s d>0.8) mean changes on the Y-BOCS scale after group and individual CBT and a non-significant effect-size difference of 0.19 Cohen’s d (95% CI 0.84 to 0.46) in favour of individual therapy.
A meta-analysis of 10 trials of CBT in HD, performed by Tolin et al.,27 showed reliable and clinically significant change in HD patients of 40.12% for functional impairmentand 25.44% for clutter. Williams et al.,28 reported effect sizes, limits and challenges of different option in HD treatment.28
Methods based on CBT
Some variations of CBT have been also developed, including CBT with bibliotherapy,29 CBT with cognitive rehabilitation30 CBT with motivational interviewing,31 CBT with internet supported group32 and isolated bibliotherapy.33‒35 In conclusion, these studies reveal that there are a percentage of hoarders who do not benefit the current CBT approaches. The limited response to current CBT approaches included a tendency to drop out during exposure, reluctance to let the therapist enter the home, decision-making deficits, lack of motivation to change and egosyntonic hoarding preoccupations.
Inference-based therapy
Inference Based Therapy (IBT,36) is an alternative CBT approach which focuses initially on hoarding doubts which according to IBT form the basis of preoccupation in both OCD and HD. In HD such doubts include: «maybe I will use this one day», «maybeI will lose my memories if I let go this object», etc. Evidence of the importance of doubts comes from studies showing such doubts can be reliably identified and measured.37 IBT focuses on these doubts as the origin of the hoarding obsession and considers the doubts pathological and illusory. The doubts are often supported by a subjectively constructed egosyntonic narrative containing missociations and out of context facts and non-pertinent sometimes imagined information which supports and justifies the doubts and so motivates the hoarding. The person with hoarding becomes immersed in illusionary doubts with spiral off into imagined possibilities remote from real probabilities. The themes of such narratives also reflect vulnerable self-themes. For example a narrative about the importance of finding a use for everything and so being ecological may reflect a wider theme that the person fears becoming un ecological. IBT has been successfully applied in single case of hoarding,38 and as a part of virtual-reality based treatment of HD.39
IBT aims to
In IBT, the person gains insight into how he/she inverses normal inference by mistaking a subjective often imaginary possibilities for real probabilities and this blending of reality and imagination, termed ‘inferential confusion’ accounts for certain types of dissociation (e.g. obliviousness; depersonalisation41 found in HD and OCD. This subjectively constructed narrative supporting the hoarding doubts helps to shift the focus away from reality and away from using sense-based criteria to decide if the object is worth keeping or not, based on realistic criteria.
In therapy the person gains insight into the confusion between reality and the illusionary associations accorded to possessions and so to help the person with hoarding realize that he/she is imposing a subjective illusionary value on the actual value of possessions. IBT also deals with apparent ego syntonic values in hoarding by exposing how the constructed hoarding-self in reality sabotages the authentic self and self-values.
This treatment was applied to HD since hoarding behaviour contains over valued ideas (OVI);42 the advantage of IBT that it has shown great symptoms improvement than CBT43 success with other types of OVI.
This open trial study planned to explore
Study sample
Participants were recruited from 2007 to 2014 from the Obsessive Compulsive Disorders and Tics Study Centre by announcement, from local health providers and from volunteers. The inclusion criteria was hoarding as a principal problem. Exclusion criteria were: bipolar disorder; psychotic disorder and schizophrenia; not stabilised on medication within the last 3months; major problems on axes I and II; organic brain disorder and suicidal ideation within the last 6months.
We screened 50peoplereporting significant hoarding problem; 11people were excluded according to the exclusion criteria, the remaining participants (n=39) were assigned to IBT: 12 participants were assigned to virtual reality-based therapy;39 and 27 participants were assigned to individual IBT therapy. Among the participants assigned to individual therapy, eight participants refused treatment before the beginning of therapy because of scheduling conflict: the IBT sessions were available in working hours only. Of the 18 participants who were enrolled in the therapy one participant abandoned. A total of 17 participants completed the therapy. Six-month follow-up data was available in nine participants. All participants from the above studies were recruited from the same reference sources; so no population bias was associated with allocation to different type of therapy.
Procedures
The IBT intervention is a program of 20weeks comprising modules addressing the difference between pathological doubts and normal doubts; the confusion between illusions and reality; exposing the narrative supporting the hoarding doubts; constructing an alternative narrative grounded in reality; making decisions based on senses and common-sense; exploring the feared-self, motivating the doubts and identified with hoarding versus recognising the authentic non-hoarding self; relapse prevention. All participants received the same manualized program and work-sheets over the same number of sessions (twenty sessions). Therapy was administered by licensed Psychologists trained in IBT for OCD and HD with at least 5years’ experience. Four separate therapists administrated identical manuals for IBT and treatment adherence and fidelity were assured by close supervision.
Measures
Participants were evaluated by independent clinical evaluators blind to type of therapy in pre and post treatment stages and 6 months after the completion of therapy.
Clinical evaluation was made with the Structured Clinical Interview for DSM-4 Axis I and Axis II Disorders (SCID-I and SCID-II). The SCID-I and SCID-II are semi-structured interview for making the major DSM-IV Axis I and II diagnoses. SCID-I has a reliability of 0.65-0.83; SCID-II has a reliability from k=0.62 for schizotypal personality disorder to k=0.94 for depressive personality disorder.45
The outcome of interest measure was the Vancouver Obsessional Compulsive Inventory Hoarding Subscale(VOCI-H.46)Vancouver Obsessional Compulsive Inventory is a 55-item self-reported questionnaire with very good internal consistency of >0.9 and good test-retest reliability of 0.8 in OCD setting. Internal consistency of the Hoarding Subscale (items 10, 22, 26, 35, 42, 45, 51) ranges between 0.8 in nonclinical adults and 0.92 in participants with OCD.
Some participants were additionally evaluated with the Saving-Inventory Revised questionnaire (SI-R,10) a23-item questionnaire which measures compulsive acquisition, difficulty discarding objects and clutter. The questionnaire has a reliability of 0.8-0.93 and internal consistency of 0.94.
Comorbidity status was assessed by Yale-Brown Obsessive-Compulsive Scale (YBOCS),47 the Beck Depression Inventory,48 the Beck Anxiety Inventory49 and Structured Clinical Interview for DSM-IV Axes I and Axes II Disorders.45
Yale-Brown Obsessive-Compulsive Scale (YBOCS) is a 19-item semi-structured interview evaluating a presence of obsessive-compulsive symptoms with an internal consistency of 0.69 and test-retest reliability of 0.9.50 Higher scores are associated with more severe symptoms. Scores between 8 and 15 are associated with mild; between 16 and 23 with moderate; between 24 and 31 with severe and between 32 and 40 with extreme obsessive-compulsive symptom severity.
Beck Depression Inventory (BDI II) is a 21-item self-report inventory of depression. Higher scores are associated with more severe depressive symptoms; scores between 14 and 19 associated with moderate; between 20 and 28 with severe and between 29 and 63 with extreme depression symptom severity (Beck, Steer, & Carbin, 1988). The test has internal consistency =0.92 – 0.93 and test-retest reliability = 0.93. Beck Anxiety Inventory (BAI) is a 21-item self-reported rating of anxiety. Higher scores are associated with more severe anxiety symptoms; scores between 8 and 15 associated with moderate; between 16 and 25 with severe and between 26 and 63 with extreme anxiety symptom severity.51 The test has an acceptable internal consistency (α = 0.84) and test-retest reliability of 0.63.
The Expanded version of the inferential confusion questionnaire (ICQ-EV,52) Aardema et al.,53 is a 30-item self-administrated questionnaire measuring distortion of the senses and imaginary possibilities; higher scores are associated with higher distrust of the senses and inverse inference. The ICQ-EV was used to evaluate attributed to therapy underlying inferences in patients’ perception. The test internal consistency is 0.97 and test-retest reliability is 0.9.
Statistical analysis
The descriptive statistics of study sample provided means/frequencies and standard deviations for continuous/ordinal variables. All measures pre- and post-test therapy and their differences scores were tested for normality of distribution; further statistics were carried out according to these tests results.
Comorbidity status measures were dichotomised as clinical/non clinical symptom severity. Cut-points were established as follow: for the YBOCS a cut-point of 15 points (0-15 vs 16 and more), for the BDI II a cut-point of 19 (0-19 vs 20 and more), and for the BAI a cut-point of 15 (0-15 vs 16 and more).The ICQ-EV scores and VOCI-H scores were dichotomised according to Jacobson(1991) from reported means and standard deviations for clinical and non-clinical samples, as (0-85) vs (86 and more) for ICQ-EV and (0-12) vs (13 and more) for VOCI-H. Missing data imputation was made using regression method.54 A significance level of 0.05 was established for all the tests.
We compared socio demographic and clinical characteristics in participants who desisted before treatment or abandoned during treatment with participants who completed therapy; we also compared participants with missing data and completed data. We compared the same characteristics in participants who completed the therapy and participants available at 6-month follow-up.
Pre-treatment vs post-treatment and 6month follow-up were analysed separately in each group by univariate general linear models for repeated measures to test for differences in VOCI-H scores as well as in mental health comorbidities measures. Age, sex, OCD, pre-treatment depression and anxiety symptoms, pre-treatment inference level and personality disorders were established as factors likely to affect or moderate the IBT efficacy; so, their impact on within and between group differences was assessed. Power of tests results and effect size (partial eta square, η2p55) was also calculated.
Hierarchical linear regression with stepwise variable selection was used to understand the impact of
Ethics
The Institutional Review Board of the approved the study. All subjects were informed about the study and all provided informed consent.
Participants
In the data set, there was one missing value for one ICQ-pre-treatment and for one ICQ post-treatment score in different participants, which were imputed using the regression method. The flow of participants is presented in Figure 1. Participants’ socio-demographic and clinical information are presented in Table 1, and pre-treatment and post-measures scores are presented in Table 2. In 14 participants the primary outcome measure was the VOCI-H scores only; in three participants primary outcome measure was available in SI-R scores only; four participants completed both VOCI-H and SI-R.
|
Variable |
Treatment, n=14 |
Follow-up, n=9 |
||
|
Age, mean (std) |
50 (10.63) |
52.22 (9.55) |
||
|
Sex, females, n (%) |
9 (64.3%) |
6 (66.7%) |
||
|
OCD, moderate to severe, n (%) |
8 (57.1%) |
4 (44.4%) |
||
|
OCD, severe, n (%) |
6 (42.9%) |
4 (44.4%) |
||
|
Obsessive-compulsive PD, n (%) |
12 (85.7%) |
9 (100%) |
||
|
Paranoid PD, n (%) |
4 (28.6%) |
2 (22.2%) |
||
|
Histrionic PD, n (%) |
3 (21.4%) |
3 (33.3%) |
||
|
Antisocial PD, n (%) |
2 (14.3%) |
1 (11.1%) |
||
|
Avoidant PD, n (%) |
6 (42.9%) |
2 (22.2%) |
||
|
Borderline PD, n (%) |
4 (28.6%) |
3 (33.3%) |
||
|
Depressive PD, n (%) |
6 (42.9%) |
4 (44.4%) |
||
|
Dependent PD, n (%) |
2 (14.3%) |
1 (11.1%) |
||
|
Negativistic PD, n (%) |
2 (14.3%) |
2 (22.2%) |
||
|
Schizoid PD, n (%) |
2 (14.3%) |
1 (11.1%) |
||
|
Schizotypal PD, n (%) |
1 (7.1%) |
1 (11.1%) |
||
|
Narcissistic PD, n (%) |
2 (14.3%) |
2 (22.2%) |
||
Table 1 Study sample characteristics
PD: Personality Disorder
|
Variable |
Pre-treatment |
Post-treatment |
|
|
VOCI_H, mean (SD)** |
22.14 (6.81) |
16.93 (7.76) |
|
|
ICQ-EV, mean (SD) |
76.34 (29.69) |
65.64 (28.37) |
|
|
BDI, mean (SD) |
18.07 (9.68) |
15 (11.31) |
|
|
BAI, mean (SD)* |
12.64 (12.39) |
8.43 (9.23) |
|
|
Y-BOCS, mean (SD)** |
25.86 (6.49) |
16.86 (8.49) |
|
Table 2 Treatment results
*Significant on 0.05 level
**Significant on 0.001 level
Participants who abandoned the study did not differ from participant who completed the therapy in terms of principal diagnosis distributions (p=0.96), sex (p=0.06), age (p=0.90) and baseline scores in BDI (p=0.84), in BAI (p=0.75), in Y-BOCS (p=0.54), and in ICQ-EV (p=0.75). There were no difference in age, sex distribution and pre-and post-treatment scores between participants with complete datasets and participants with missing data. Participants non-available for 6-month follow up had a lower probability of obsessive-compulsive personality disorder (chi-square test; p=0.04) and higher probability of avoidant personality disorder (chi-square test; p=0.036) than those who presented at follow-up. However, there was no difference in overall distribution in demographical and clinical variables in participants completing the treatment and participants available for 6month follow-up.
Pre-treatment vs post treatment
The general linear model showed significant within-group difference in VOCI-H pre-and post treatment scores at the level of p=0.001 (x̄ = -5.21 SD=4.60, p=0.001, η2p=0.58). There were no demographical and clinical variables interacting with the treatment effect.
A significant between-group difference was found in groups of clinical/non clinical depression (p=0.035) and anxiety symptoms (p=0.01) and a marginally significant difference was found in groups of high and low ICQ-EV levels (p=0.085). Subjects with clinical depression or/and anxiety symptoms or/and higher ICQ-EV scores had a tendency to
|
|
Depression Symptoms |
x̄ |
||
|
|
Clinical, n=5 |
Non-clinical, n=9 |
||
|
Pre-treatment |
27.8 |
19 |
8.8 (p=0.013) |
|
|
Post-treatment |
21.4 |
14.44 |
6.96 (p=0.11**) |
|
|
x̄ |
6.4 (p=0.013) |
4.56 (p=0.031) |
||
|
|
Anxiety Symptoms |
x̄ |
||
|
|
Clinical, n = 4 |
Non-clinical, n = 10 |
||
|
Pre-treatment |
30 |
19 |
11 (p=0.02) |
|
|
Post-treatment |
23 |
14.5 |
8.5 (p=0.06*) |
|
|
x̄ |
7 (p=0.029) |
4.5 (p=0.018) |
||
|
|
Confused inferences |
x̄ |
||
|
|
Higher level, n=7 |
Lower level, n=7 |
||
|
Pre-treatment |
25.86 |
18.43 |
7.43 (p=0.035) |
|
|
Post-treatment |
19.57 |
14.29 |
5.29 (p=0.25**) |
|
|
x̄ |
6.29 (p=0.001) |
4.14 (p=0.11**) |
||
Table 3 Changes in VOCI-H scores in higher BDI, BAI and ICQ-ev groups
*Statistical power in range 0.5-0.6
**Statistical power in range=0.2-0.49
6month follow-up
A global test of differences in VOCI-H scores across the three time points (pre-treatment, post-treatment, 6-months follow-up) was significant at the level of p=0.043, η2p=0.33 (pre-treatment – post-treatment: x̄=-5.11, SD=1.73, p=0.018; pre-treatment - 6months follow-up: x̄ = -6.0; SD=2.73, p =0.06; post-treatment – 6 month follow-up : x̄= -0.89, p=0.72). The difference remained significant after controlling for demographical and other clinical variables, except depressive personality disorder.
The presence of depressive personality disorder significantly modified treatment effect (p=0.003, Figure 2): participants with depressive personality disorder (n=4) showed less pre- and post-treatment difference in mean VOCI-H scores and no difference between pre-treatment and 6-month follow-up scores while participants without the disorder (n=5) showed a clear descending linear trend in VOCI-H changes across all the time-points.
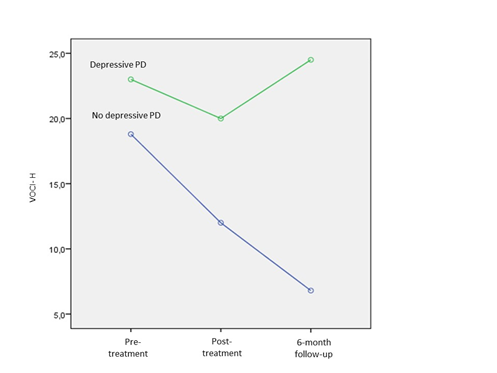
Figure 2 Changes in VOCI-H scores in pre-treatment, post-treatment and 6-month follow-up in participants with and without depressive personality disorder (DPD).
The participants were divided into OCD -/+ according to a clinical diagnosis on the SCID-I and the VOCI-H scores were compared between the two groups. There were no differences in outcome on hoarding in participants classified as both severe and moderate OCD.
Twelve of 14 participants (86%; CI 67%-100%) showed positive changes in hoarding; four of them achieved the threshold of clinically significant changes in hoarding established according to the Jacobson and Truax criteria (28%, CI 5%-55%); all of them maintained the gain at follow-up; three of them crossed the threshold to non-clinical status at follow-up (33%, of nine participants at follow-up, CI 3%-64%) (VOCI-H=6). Six of nine participants (66%, CI 35%-97%) had positive changes in hoarding between baseline and 6-month follow-up; two of nine had no changes and one of nine had negative changes in hoarding.
Seven participants’ treatment effect was measured with SI-R and pre-treatment scores were compared with post-treatment (n=5) or follow-up scores (n=2). These SI-R results corroborated findings measured in VOCI-H (general linear model; global SI-R changes scores: x̄ =-27.14, SD=9.1, p=0.025, η2p=0.60; difficulty discarding: x̄ =-9.86, SD=3.31, p=0.025, η2p=0.60; acquisition: x̄ -8.43, SD= 2.95, p=0.03, η2p=0.58; cluttering x̄ =-8.86, SD=3.8, p=0.06, η2p=0.48).
Hierarchical linear regression
Hierarchical linear regressions with stepwise variable selection showed an impact of pre-treatment BDI on pre-treatment VOCI-H scores: r2 =0.46, β = 0.5, SD=0.14, p=0.005. There was no variable influencing the change between VOCI-H pre- and post-treatment scores.
The regression model for the VOCI-H scores at 6-month follow-up had an r2 of 0.78 and included depressive personality disorder (β= 17.7, SD=3.25, p=0.001) as the independent variable.
The IBT showed overall positive changes and a clinically significant diminution of hoarding symptoms in the range previously reported for CBT.27 The effect of IBT remained stable at 6-month follow-up for 100% of cases who had shown clinically significant post-treatment hoarding improvement; there was no difference between post-treatment and 6-month follow-up hoarding scores. The treatment had a large effect-size57 both at post-treatment and maintained at 6-month follow-up.
Depression, anxiety symptoms and high inferential confusions level or a combination of these factors were associated with higher pre-treatment hoarding level and affect the hoarding dynamics during the treatment, but more observation is required to understand the impact of each of these variables separately on treatment. Absence of depressive personality disorder was a strong predictor of improved VOCI-H scores at follow-up. Neither baseline moderate nor severe OCD, nor age and sex influenced treatment effects.
The reduction of Y-BOCS scores logically followed from the fact that the IBT addressed doubts, illusions and over evaluated ideas also relevant to OCD. As well, improvements in anxiety symptoms can be explained by diminution in hoarding. There were no participants with normal/mild level of Y-BOCS scores, so, we could not test the impact of OCD severity on treatment results more precisely then by using established OCD diagnosis.
Results are preliminary due to weak statistical power but the preliminary results do give some insight in the hoarding therapy process. Other limits of the study are clearly the lack of a control group and the small number of completers. The choice of the VOCI-H scale as an outcome measure did not permit evaluating the hoarding components: such as difficulty discarding; acquisition; and clutter. However improvement was confirmed in a sub-sample of participants through convergence with the SI-R.
IBT directly addresses clinical features particular to hoarding: namely doubts and dissociative states (reasoning process giving rise to these doubts; inferential confusion and feared self). IBT is largely cognitive in nature and addresses the overvalued ideation in hoarding through targeting illusory associations and inferential confusions as well as beliefs about the self. The IBT target of doubt is a central component in changing the motivation to hoarding and is not addressed in traditional CBT. Whether focusing on cognitive factors facilitates eventual discarding requires a larger scale dismantling design but the clinical improvement shown in the preliminary results give a limited insight into the efficacy of the therapy process in IBT for hoarding.
Further, the results indicate that the presence of OCD did not impair application of the program but does highlight the role of personality disorder and comorbidity in limiting treatment success. IBT also grapples with the ego syntonic aspects of hoarding less by motivational interviewing and more by revealing how hoarding behaviour reflects a feared rather than an authentic self. For example a person may store newspapers convinced that the travel sections ‘may’ one day be useful and that he is the sort of person who could forget or will lose this information and be incapable of finding the information elsewhere. But listing the attributes of his authentic Self show he is a capable and efficient person well able to inform himself from diverse sources. This focus may help in repatriating the person from the paralysing world of hypothetical negative possibilities to the more dynamic and grounded land of the living. Self-themes seem to be increasingly recognised as underlying motivations for OCD.58
The advantage of focusing on the feared self as one such self-theme may be that the feared-self reveals to the person the underlying insecurity motivating the doubts which in turn support the hoarding of one type but no other type of objects or hoarding in one but no other situations So what appears to be ego syntonic values in hoarding are an illusion generated by close identification with the self the person erroneously fears they can become, the feared self, and not the authentic self. IBT then complements existing approaches to HD and the cognitive aspects of IBT may add new dimensions to existing CBT approaches.
It makes us a pleasure to thank our clinical coordinator, Natalia Koszegi and our administrative coordinator, Karine Bergeron, for their engagement in the project.
Author declares there are no conflicts of interest.
Author declares there are no conflicts of interest.

©2016 Blais, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.