Journal of
eISSN: 2373-6445


Review Article Volume 15 Issue 5
1Clinical Professor, Family and Community Medicine/ Core Faculty Member at CNAH(Center For Native American Health)/University Of New Mexico, USA
2Tribal Relations Liaison, Center for Native American Health - a Public Health Institute for Indigenous Knowledge and Development/Lecturer II, Department of Family & Community Medicine/University of New Mexico Health Sciences, USA
3Senior Peer Specialist, Presbyterian Health Care Services, USA
4Psychopharmacologist Merano (Bz), Italy
Correspondence: Marcello Maviglia, Clinical Professor, Family and Community Medicine/ Core Faculty Member at CNAH(Center For Native American Health)/ University Of New Mexico, Albuquerque, USA, Tel 505-272-1855/ 1505620628
Received: October 10, 2024 | Published: October 22, 2024
Citation: Maviglia M, Hume D, Cooeyate NJ. Kindling in psychopharmacology: Unveiling an overlooked clinical challenge with significant implications. J Psychol Clin Psychiatry. 2024;15(5):282-290. DOI: 10.15406/jpcpy.2024.15.00793
The kindling phenomenon, often overlooked in clinical settings, emerges during the withdrawal phase from various substances, including sedative-hypnotic drugs (such as benzodiazepines and alcohol), psychiatric medications, and opioids. The progressive worsening of withdrawal symptoms with each successive episode characterizes this phenomenon. Consequently, its implications extend far beyond immediate clinical manifestations.
A thorough understanding of how to prevent kindling is crucial in the treatment of Substance Use Disorders and mental health conditions. Elucidating the mechanisms underlying kindling is essential for researchers, clinicians, and individuals undergoing treatment. This article delves into the implications of kindling, explores the issue of differential diagnosis, addresses strategies for its effective clinical management, and aims to enhance treatment outcomes. Additionally, it highlights the invaluable roles of medical doctors, therapists, and peer support specialists in addressing the challenges of kindling.
Keywords: kindling, psychiatric drugs withdrawal, ethics of medication withdrawals, peer specialists and kindling
Initially described by neuroscientist Graham Goddard, kindling represents a complex and multifaceted neurological condition. It arises as a consequence of repeated withdrawal episodes from a variety of substances, including sedative-hypnotic drugs (such as benzodiazepines and alcohol), psychiatric medications, and opioids. A progressive worsening of withdrawal symptoms with each subsequent episode characterizes kindling.1–3
Despite its clinical significance, kindling often remains unrecognized in routine practice, highlighting the necessity for early detection and intervention in patient care. In reality, it should be considered a critical concept in the management of psychotropic drugs. Many psychiatrists, often lacking the necessary experience and preparation, may frequently add and remove various psychotropic medications with relative ease and within short periods. This practice aims to suppress symptoms of mental suffering or withdrawal effects but often neglects the necessary steps for the safe discontinuation of these drugs.4
This widely adopted approach can have problematic consequences, leading to significant psychological and physical distress. The core issue is the sensitization of the nervous system receptors, resulting in exaggerated neurological, psychological, and physical responses.
For instance, individuals who initially had minimal difficulty discontinuing a psychotropic drug might, upon reintroducing the same drug or switching to another, experience much more severe withdrawal symptoms during subsequent discontinuation attempts. This heightened sensitivity occurs because the nervous system, having endured multiple withdrawal events and adverse effects from the drugs, becomes destabilized and sensitized.5–7
This article addresses this oversight by exploring the multifaceted aspects of kindling. We will examine its underlying biological mechanisms and the educational needs of patients, clinicians, and professionals. Additionally, we will outline strategies for evaluating the kindling phenomenon and discuss essential considerations for effective treatment and preventive strategies.
Furthermore, we will emphasize the crucial roles therapists and peer specialists play in addressing the challenges of kindling. By thoroughly examining this phenomenon, we aim to enhance clinical awareness, underscore the importance of timely prevention and treatment, and ultimately improve patient outcomes.
Ethical considerations in medication withdrawal
The process of withdrawing from psychiatric medications often presents significant challenges, primarily due to the lack of available support for individuals pursuing this option. Many resort to a “do-it-yourself” approach without professional guidance, which can lead to severe complications. One such complication is the kindling phenomenon, where each subsequent withdrawal attempt becomes progressively more difficult and problematic.8,9
Given these risks, healthcare professionals must provide appropriate medical support to individuals considering psychiatric drug withdrawal. This support is not just a medical necessity but also an ethical obligation. Several articles have examined this issue.10,11 A more recent article highlights the ethical dimensions of this issue, emphasizing the need for services that assist individuals in reducing or stopping antipsychotic medications. The article aligns this support with four core ethical principles: autonomy, justice, nonmaleficence, and beneficence.12
The authors emphasize that clinicians must carefully balance several ethical principles to support a patient’s recovery during medical withdrawal effectively. Each principle correlates with a specific aspect of medical care:
The ethical considerations highlighted in the article underscore the importance of supporting patients who wish to reduce or stop antipsychotic drugs. By aligning withdrawal strategies with these ethical principles, healthcare providers can help prevent the almost irreversible kindling phenomenon and improve patient outcomes.
Mechanisms implicated with kindling for psychiatric medications and addictive substance
Chronic use of substances like alcohol, benzodiazepines, antidepressants, antipsychotics, mood stabilizers, stimulants, and opioids, along with repeated withdrawal episodes, leads to significant changes in the brain’s neurotransmitter systems. This primarily affects the balance between inhibitory and excitatory neurotransmission mediated by GABA and glutamate. The resulting imbalance can cause a range of withdrawal symptoms and the kindling effect, where each withdrawal episode becomes progressively more severe.4,12–15
This destabilization is marked by reduced sensitivity of GABA receptors and increased activity of glutamate receptors, leading to a hyper-responsive state. This heightened responsiveness manifests as severe withdrawal symptoms, including intense anxiety, depression, nervousness, insomnia, and panic. In extreme cases, individuals may experience akathisia, a condition characterized by an overwhelming need to move continuously to alleviate intense inner agitation, which can become so unbearable that it may lead to suicidal thoughts.4,12–15
It is worthwhile to emphasize that the kindling phenomenon extends beyond alcohol and sedatives to various psychiatric medications. For example, individuals who initially had minimal difficulty discontinuing a psychotropic drug might experience much more severe withdrawal symptoms during subsequent discontinuation attempts.16
Understanding the roles of the GABAergic and Glutamatergic systems and the broader cascade of neurotransmitters helps clinicians manage withdrawal symptoms and prevent kindling progression. This knowledge underscores the importance of gradual tapering, individualized treatment plans, and close monitoring to mitigate the risks of kindling and improve patient outcomes.8
Prevention
Due to the lack of effective treatment interventions regarding kindling, the best intervention is prevention. As already stated, many healthcare professionals may not fully grasp the intricacies of withdrawing people from psychiatric medications and of the kindling effect. This can significantly hinder the effectiveness of treatment plans and the management of withdrawal symptoms, resulting in suboptimal treatment outcomes.17
Prescribers, for example, may prescribe anticonvulsants (i.e., carbamazepine and valproate) to manage withdrawal symptoms and prevent kindling. However, the appropriateness of these interventions is debatable. From the data and reports available, avoiding repeated episodes of withdrawal should be a primary focus in the management of psychiatric medication discontinuation. As shown by the gray and official literature, psychiatric drug withdrawal syndromes have been increasingly documented, with recent studies indicating that the incidence of antidepressant withdrawal syndrome is widespread in the face of a significant lack of medical information on safely discontinuing these medications.17
This gap was initially addressed by individuals with lived experience who have established a comprehensive online network to provide peer support to assist in the tapering of psychiatric medications and managing withdrawal symptoms.18,19
A significant example is the first peer-lead online site, SurvivingAntidepressants.org, which has operated since 2011 under the pseudonym Altostrata. It has been a pivotal resource for promoting the understanding of the complexity of psychotropic treatment and withdrawal, providing guidance and insights to avoid negative consequences.20
Differentiating psychological and physical dependence
Understanding the difference between psychological and physical dependence is essential, particularly when discussing psychiatric medications. Critics often claim that these medications do not cause dependence because individuals do not display typical addictive behaviors. However, this view fails to recognize the complex nature of dependence.
Substances like opioids, stimulants, and alcohol are well-known for causing both psychological and physical dependence. Similarly, recognizing the type of dependence that psychiatric medications can cause is crucial for accurate diagnosis and effective treatment planning. This nuanced understanding is vital for providing better care and support to individuals who rely on psychiatric medications.21,22
The physical dependence on a drug manifests through tolerance, where increasing doses are necessary to achieve the same effect, and withdrawal symptoms, such as nausea, sweating, tremors, and seizures when the drug is discontinued. In contrast, psychological dependence is characterized by an emotional need for the drug to attain emotional well-being or to avoid psychological discomfort, leading to compulsive drug-seeking behavior despite adverse consequences. The key differences between the two reside in their symptoms: physical dependence involves bodily symptoms like nausea and seizures, while psychological dependence involves emotional and cognitive symptoms such as cravings, anxiety, and compulsive behavior.21–23 Individuals experiencing psychological dependence may feel that their emotional stability is closely tied to the consumption of the substance, leading to a persistent and compelling urge to use it.24
This form of dependence also brings about significant behavioral changes. People may engage in drug-seeking behaviors, repeatedly using the substance despite being fully aware of the negative consequences. This compulsive behavior highlights the powerful hold that psychological dependence can have on an individual’s actions and decisions, often overriding rational thought and self-control.
On the other hand, physical dependence is primarily associated with bodily symptoms that arise when the substance is not available. They can include nausea, tremors, and seizures, indicating the body’s adaptation to the presence of the drug and its subsequent struggle without it. In contrast, psychological dependence is characterized by emotional and cognitive symptoms.21–24
However, in clinical practice, these two types of dependence may not be so easy to distinguish and separate, as they often may present as a hybrid phenomenon (e.g., withdrawal signs and symptoms may present along with obsessive thoughts about using a particular substance, even when a typical full-blown picture of psychological dependence cannot be established). Therefore, we could argue that the two entities may blend in a synergic dynamic that contributes to the use of substances and pharmaceuticals (speculation). Among the psychiatric drugs commonly used, probably benzodiazepines have a higher chance of causing psychological dependence.24–26
Also, a critical aspect of withdrawal from substances and psychiatric medications is that it manifests in different ways, as its signs and symptoms may vary with time and among individuals. It is pivotal to acknowledge these multiple clinical features so that we can distinguish among pure signs and symptoms of withdrawals, Post-Acute Withdrawal Symptoms (PAWS), Protracted Withdrawal Syndrome (PWS), Kindling, and symptoms of Relapse into the original and recurring psychiatric symptomatology.
Post-acute withdrawal symptoms (PAWS) and protracted withdrawal syndrome (PWS) from psychiatric medications
The terminology surrounding withdrawal symptoms following the cessation of substance use can be quite complex, particularly with terms like "Post-Acute Withdrawal Symptoms" (PAWS) and "Protracted Withdrawal Syndrome" (PWS). Therefore, Understanding the distinctions and similarities between these terms is essential for effective clinical practice and research.7,27–29
PAWS encompasses a range of symptoms that may persist long after the regular acute withdrawal phase has concluded.30–50 The syndrome includes essentially the symptoms present in the period of acute withdrawal, like anxiety, depression, sleep disturbances, and cognitive impairments. They can continue in a modified pattern for weeks or even months after stopping substance use.50,51 PAWS is often associated with various substances, including opioids and benzodiazepines, and is recognized as a significant factor contributing to relapse among individuals in recovery.50,51 There is also evidence that it is associated with withdrawal from psychiatric medications, although there is less awareness regarding it.8,17 The debilitating nature of these symptoms can elevate the risk of relapse, as individuals may turn to injudicious use of medications and substances in an attempt to alleviate their discomfort.50,51 It is imperative to manage this phase meticulously, as improper and hazardous pharmacologic interventions can result in complications, including the kindling phenomenon. Therefore, a comprehensive understanding and effective management of PWS are essential to prevent additional complications and ensure a smoother and more sustainable recovery trajectory.7,27–29
Protracted withdrawal syndrome (PWS)
In contrast, PWS refers to a more persistent set of withdrawal symptoms that can manifest after the acute withdrawal phase, following the discontinuation of substances and psychiatric medications, as previously stated for PAWS.52,53 Research indicates that PWS can last for months or even years and may involve severe mood disturbances, cognitive deficits, and other psychological issues.52,53 Although both PAWS and PWS describe essentially the same set of withdrawal symptoms, PWS is typically associated with more problematic and chronic trends.54
In summary, both PAWS and PWS refer to prolonged withdrawal symptoms, but a chronic trend characterizes PWS.
As already stated, while these syndromes, like kindling, have been stressed more with withdrawals from alcohol, benzodiazepines, and other potentially addictive substances, there is enough evidence to state that they can occur with psychiatric medications as well.8,17
Differentiating relapses in mental health syndromes from psychiatric medication withdrawals
Relapses into active mental health syndromes and withdrawals from psychiatric medications often present with overlapping symptoms, complicating accurate diagnosis and treatment. Relapses are usually characterized by the return of symptoms of a mental health disorder after a period of improvement, triggered by multiple psychosocial factors.8,17 They typically mirror those of the initial episode, such as depressive symptoms in major depressive disorder or psychotic symptoms in schizophrenia. In contrast, withdrawal symptoms are more chronologically closer to the reduction or discontinuation of psychiatric medications and can be both psychological and physical, often emerging within days of dose reduction.6,7,32,55
More specifically, typical withdrawal symptoms include anxiety, mood swings, and physical complaints such as dizziness and flu-like symptoms. Distinguishing features include the temporal onset, with withdrawal symptoms appearing shortly after medication changes, whereas relapses can occur independently of such changes.6,7,8,17,32 Moreover, withdrawal symptoms often are characterized by a wave-like pattern, with periods of intensity followed by resolution, while relapses tend to present with a steady progression of symptoms.8 Additionally, withdrawal symptoms usually improve rapidly upon reinstating the medication, whereas relapses may not respond as quickly to treatment adjustments. As already stated, withdrawal symptoms can also include new physical symptoms not previously experienced by the patient, while relapses generally involve a recurrence of previous mental health symptoms.8
Obviously, in clinical practice, it is often challenging to differentiate between relapses and withdrawal symptoms. Still, it is essential for appropriate clinical management since it may affect both the clinician’s and patient’s perceptions of the course of the illness and how to plan for treatment by targeting the individual's real needs with safe, effective, and least invasive interventions, which may include aggressive and extended biological treatment.8
Individualized tapering to avoid bad outcomes, including kindling
Having stated so far, the difficulties in assessing the clinical status and needs of individuals who have stopped or are in the process of withdrawing from psychiatric medications is not surprising that clinicians frequently misinterpret withdrawal symptoms as relapse. For example, antidepressant withdrawal symptoms manifest with a variety of signs and symptoms, impacting both physical and mental health.6–8
In his vein, we need to consider that withdrawal symptoms typically emerge following dosage reductions and may include atypical neurophysiological signs such as electrical sensations (often described as “zaps”), sudden dizziness, pain, nausea, and insomnia. In the absence of other medical explanations, these symptoms likely indicate withdrawal syndrome. Patients often describe these symptoms as novel and exceptionally severe, in contrast to the more consistent pattern observed in relapse.8 This pattern is also reported for other psychiatric drugs. For benzodiazepines, withdrawal symptoms can include anxiety, irritability, tremors, sweating, and, in severe cases, seizures. Antipsychotic withdrawal may present with symptoms such as insomnia, agitation, psychosis, and motor disturbances. Mood stabilizers like lithium can cause withdrawal symptoms, including mood swings, irritability, and physical symptoms like tremors and nausea. Stimulant withdrawal often manifests as fatigue, depression, and increased appetite, while muscle aches, sweating, nausea, and diarrhea characterize opioid withdrawal.8
When planning for tapering and withdrawal in a clinical setting, it is imperative to implement a small reduction schedule to avoid complications. For example, a 5-10% reduction of the current dose (not the initial dose) per month should be seriously considered. Also, while some reductions might cause mild discomfort for a few days, patients should not endure significant withdrawal symptoms for extended periods. Therefore, if symptoms do not improve or worsen after a few days, a slight dosage increase can often resolve these symptoms, as recommended. This immediate adjustment helps preserve the individual’s potential for more tolerable withdrawal and encourages a positive prescriber-patient relationship.8,17 This method, known as exponential taper, involves progressively smaller reductions and can span many months to several years, depending on the individual’s tolerance. Therefore, systematic reductions are highly effective in minimizing withdrawal symptoms, making them essential for harm reduction in psychotropic medication management. Additionally, it is crucial to maintain a consistent dosing schedule when tapering off medication. Skipping doses can lead to fluctuations in drug levels, which may provoke kindling reactions. For example, a patient tapering off benzodiazepines should follow a meticulously planned schedule, reducing the dosage gradually and consistently to avoid sudden drops in medication levels. This systematic approach helps to prevent the nervous system from becoming overstimulated and reduces the likelihood of severe withdrawal symptoms.8,32,33
As already mentioned, to manage psychiatric medication withdrawal and prevent kindling, it is crucial to distinguish between side effects, relapses, and withdrawal symptoms. In reality, Individuals may already experience adverse drug reactions such as insomnia, sexual dysfunction, activation, and allergic reactions once tapering begins, which could be mistaken for withdrawal symptoms, leading to inappropriate treatment and prolonged suffering.17,30
Also, a daily diary is vital for monitoring and distinguishing these symptoms. By recording daily medication doses and symptoms, patients and clinicians can identify specific patterns and differentiate between adverse drug reactions, withdrawal symptoms, and relapses. While questionnaires and symptom-tracking scales can be helpful, they often fail to capture the daily chronology and course of symptoms necessary for accurate evaluation and treatment. Understanding symptom patterns through daily monitoring allows for a more person-specific treatment plan. It also helps untangle polypharmacy's complexities, ensuring a more effective and safe withdrawal process. Therefore, a personal diary should complement withdrawal scales.17,31
In addition, it is crucial to recognize that once the kindling phenomenon is established, the nervous system becomes markedly more sensitive to changes in dosage or the introduction of new psychotropic medications. This heightened sensitivity means that many individuals may exhibit severe reactions even to minimal doses of psychoactive substances. These reactions can manifest as either activation or paradoxical responses, where the expected effects of the substance are reversed. Increasing or reinstating medication using only a tiny fraction of the original dosage is recommended to prevent kindling reactions. For instance, if a patient is withdrawing from 20 mg of citalopram, reintroducing just 1 mg can often alleviate withdrawal symptoms without triggering severe reactions. This modality of careful titration stabilizes and helps minimize the development of kindling.17
Moreover, this hyper-reactivity is not limited to psychotropic medications alone. Small amounts of alcohol can provoke significant responses, as can antibiotics, which may interfere with neurotransmitter systems. Additionally, certain herbs and foods, particularly those containing psychoactive compounds, can trigger similar reactions. Supplements, such as caffeine and B vitamins, with their stimulating properties, can also exacerbate this sensitivity. Furthermore, sensory stimuli, including sound and light, can act as potent triggers, leading to overstimulation of the nervous system. Understanding the range of substances and stimuli that can affect individuals with kindling is essential for managing and mitigating potentially adverse reactions.17
Furthermore, It cannot be stressed strongly enough that withdrawal from psychiatric medications can be a psychologically disorienting and isolating experience. The emotional challenges individuals face during this time can be overwhelming. For example, many individuals experience a profound shock upon realizing they no longer have a pharmacologic safety net. This realization can trigger intense feelings of abandonment, helplessness, and existential fear. This heightened emotionality is often misdiagnosed by clinicians, who may mistakenly interpret it as a relapse following discontinuation (Figure 1).19,34
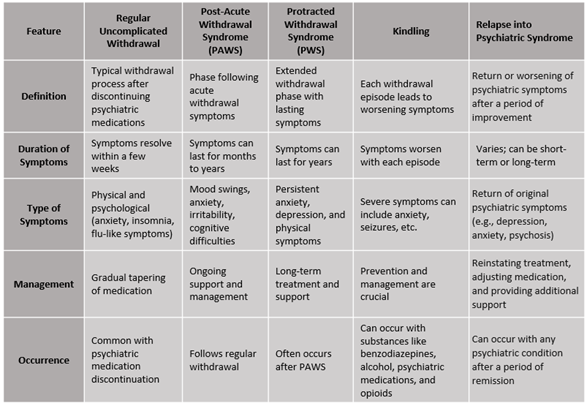
Figure 1 Comparative table summarizing the key features of Withdrawal Syndrome (PAWS), Protracted Withdrawal Syndrome (PWS), and Kindling.
Support from healthcare providers
Support from medical professionals is crucial for managing symptoms and preventing complications. Healthcare providers play a vital role in several critical areas of the process. Regular monitoring of medication changes helps timely identify and manage adverse drug reactions (ADRs) and withdrawal symptoms. Close observation allows for prompt adjustments to treatment plans, reducing patient discomfort and risk.8,17,37
To minimize withdrawal risks, practices such as irregular dosing and abrupt medication changes need to be avoided. Consistent dosing schedules and gradual transitions between medications lead to safer withdrawal experiences.8,17
Customizing tapering plans to each patient’s unique needs helps reduce the risk of complex withdrawal syndromes. Prolonged symptoms beyond the acute phase are often due to withdrawal rather than relapse, as already stated. Proper awareness and training on tapering techniques are essential for safely discontinuing drug use. Understanding the importance of gradual dose reductions and recognizing when adjustments are needed are fundamental aspects of personalized tapering and withdrawal interventions.29,35,36,38 Medical manuals should include a diagnostic framework for psychotropics-related complex withdrawal syndromes, providing guidelines for identifying these conditions, distinguishing them from relapse, and implementing appropriate treatment strategies.17,29,35,36,38,39
Role of therapists
Therapists play a pivotal role in managing the psychological aspects of withdrawal and kindling, employing various therapeutic approaches to assist patients in navigating the emotional and mental challenges associated with withdrawal.40,43–45 Several therapeutic strategies may be applied. For example, Cognitive-behavioral therapy (CBT) is fundamental in addressing anxiety, depression, and other psychological symptoms during withdrawal. By using the principles of CBT, therapists help patients identify and alter negative thought patterns and behaviors, providing practical tools and strategies that foster symptom management and a sense of control over mental health.40,41
Additionally, therapists can develop individualized treatment plans tailored to each patient’s unique history of substance use and withdrawal experiences. These plans often incorporate coping strategies, stress management techniques, and lifestyle modifications to support long-term recovery, enhancing treatment effectiveness and improving patient outcomes. Supportive counseling offers patients a safe and confidential space to express their fears, frustrations, and hopes.40,41 It is crucial for emotional support and building a trusting therapeutic relationship. As part of it, psychoeducation empowers patients by educating them about the withdrawal process, potential symptoms, and coping mechanisms, reducing anxiety and promoting a sense of control.41–45 It also emphasizes the importance of adhering to tapering plans and the risks associated with abrupt discontinuation.42
In addition, family therapists can help individuals understand the purpose and potential effects of their medications, address any concerns or misconceptions, and monitor the impact of these medications on family dynamics. By working closely with prescribing physicians, family therapists ensure that the treatment plan is holistic and considers the emotional and relational aspects of the client’s life. This collaborative approach enhances medication adherence and promotes well-being and family cohesion.56
Peer support offers unique benefits in helping people during withdrawal from psychiatric medications:
Peer specialists use their lived experiences to support others facing similar challenges. They provide emotional support, share coping strategies, and help navigate recovery.18,48,49
In the context of psychiatric medication withdrawal, peer specialists play a crucial role. Their unique insights and empathy make them invaluable allies.18,48,49 Peer support offers exceptional benefits in helping people during withdrawal from psychiatric medications. One key benefit is the shared experiences and understanding it provides. In peer support groups, individuals can openly share their struggles and gains with others who have faced similar challenges. This mutual understanding fosters a sense of community and belonging, which can significantly reduce feelings of isolation.17,19
Additionally, peer specialists provide practical advice and encouragement. Their firsthand experience managing withdrawal symptoms and adhering to treatment plans makes their guidance particularly practical. They can offer tips and strategies that have worked for them, making the journey more accessible for those currently going through it.46,47 Seeing peers who have successfully navigated withdrawal and achieved recovery can be incredibly motivating. These role models demonstrate that recovery is not only possible but sustainable. Their stories provide hope and inspiration, showing that a fulfilling life beyond medication is attainable.50
Peer specialists can also bridge the gap between patients and professionals, offering insights that might not be apparent to those who haven’t experienced firsthand withdrawal. This collaboration can enhance the overall treatment plan, ensuring it is more empathetic and tailored to the individual’s needs. By combining therapists’ expertise with peers’ lived experiences, individuals withdrawing from psychiatric medications receive comprehensive support. This holistic approach addresses their psychological journey, making recovery more manageable and hopeful.17,19,45
Case vignette: Mark's journey to safe antidepressant withdrawal
Withdrawal from psychiatric drugs requires a combined effort from professional therapists, peer specialists, and support networks. The principles of recovery serve as valuable guidelines in the context of therapeutic freedom. The vignette is fictitious but reflects a likely scenario during the withdrawal phase. It exemplifies a patient’s withdrawal process and illustrates how the team can work together.
Vignette: Mark, 35, has been on fluoxetine (Prozac) for years to manage depression. He is aware that stopping abruptly the medication can cause severe mood swings and flu-like symptoms. To prevent kindling, his psychiatrist, Dr. Parnasio, recommends a slow taper over several months, with regular monitoring and support. Mark also engages in psychotherapy to develop coping strategies and address underlying issues. However, Mark’s mother is not in favor of the withdrawal and tends to interfere with the treatment.
Dialogue and narrative:
Initial consultation:
Developing a tapering plan:
Educating about complications:
Engaging in psychotherapy:
Addressing family concerns:
Family Counseling Sessions:
During family counseling:
Support from Peer Specialists:
Ongoing monitoring and adjustments:
Team member approaches:
Through a collaborative approach involving his psychiatrist, therapist, and peer support specialists, Mark successfully navigates the withdrawal process. The slow tapering plan, combined with regular monitoring, psychotherapy, and peer support, helps him avoid kindling and manage withdrawal symptoms effectively. Keeping a daily diary plays a crucial role in distinguishing between side effects, withdrawal symptoms, and relapses, ensuring a safe and supportive journey towards discontinuing his medication. Family counseling sessions help address concerns and ensure that Mark’s mother understands and supports the treatment plan, fostering a supportive environment for his recovery. Mark’s newfound independence and open communication with his mother strengthen his resolve and support system.
The urgency of addressing kindling in SUD treatment cannot be overstated. Its profound impact on patient outcomes requires a multifaceted approach integrating education, specific and meticulous treatment, and interdisciplinary collaboration. By increasing awareness and understanding of kindling among healthcare providers and patients, we can foster informed decision-making and timely interventions that mitigate the risks associated with withdrawal.
Tailored treatment approaches, including individualized detoxification protocols and gradual tapering, are essential for managing withdrawal symptoms effectively. Close monitoring and collaboration among healthcare providers ensure that patients receive comprehensive care that addresses their physical and psychological needs.
Holistic care that addresses psychosocial factors, co-occurring mental health conditions, and social support networks is vital for comprehensive patient care. Integrating these elements into treatment plans can provide a more supportive and effective recovery process.
Promoting research opportunities and offering continuing medical education (CME) programs will keep healthcare providers updated on best practices. This ongoing education is essential for maintaining high standards of care and ensuring that providers are equipped to handle the complexities of SUD treatment.
Workshops and training can build confidence and competence in managing withdrawal symptoms, including kindling. These educational initiatives will equip healthcare providers with the skills and knowledge to support patients effectively.
Policy advocacy is necessary to integrate kindling into clinical guidelines and secure funding for related research and education initiatives. Interdisciplinary collaboration with specialties such as primary care and neurology will enhance our understanding and management of kindling, leading to more effective treatment strategies.
Networking among patients and providers is crucial for developing awareness and support. Engaging with professional organizations' online support groups and various peer support networks can provide valuable resources and connections. These networks facilitate the exchange of knowledge, experiences, and best practices, enhancing the overall quality of care.
Finally, involving patients and peer support specialists in educational sessions can provide valuable insights and enhance patient-centered care. Peer support can offer practical advice, encouragement, and motivation, creating a sense of community and belonging that is crucial for recovery.
By implementing these strategies, we can bridge the knowledge gap, improve the management of psychiatric drug withdrawal, prevent kindling, and ultimately enhance patient outcomes and quality of care.
None.
None.
The authors declare that there is no conflict of interest.

©2024 Maviglia, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.