Journal of
eISSN: 2373-6445


Research Article Volume 6 Issue 7
1Assistant Professor at Islamic Azad University, Iran
2Psychometry, Shahid Doctor Lavassani Hospital, Iran
3MD, Iran
4MA in Psychology of Family Therapy, Family Reaserch Institute of Shahid Beheshsi University, Iran
5Student of PhD in Psychology, Semnan University, Iran
Correspondence: Seyedeh Samera Hoseini, Student of PhD in Psychology, Semnan University, Iran
Received: February 23, 2016 | Published: December 28, 2016
Citation: Baniasad MH, Zolfaghari Z, Payandan H, Sadeghi N, Davoodi J, et al. (2016) Evaluate the Effectiveness of ECT in Borderline Personality Disorder Resistant to Treatment. J Psychol Clin Psychiatry 6(8): 00411. DOI: DOI: 10.15406/jpcpy.2016.06.00411
Aim: It's different fields of borderline personality disorder and are associated with characteristics of turbulence and emotions of anxiety, anger, depression and risky behaviors such as self-injury and drug abuse. Hospitalization for ECT provides an opportunity to begin treatment, change of previous therapy or management of the crisis. Electroconvulsive therapy is the most effective psychiatric treatment that in this study investigated its effectiveness in patients with borderline personality disorder resistant to treatment.
Methods: The method of this study was Case Series which were selected by available sampling, samples of 10 patients with borderline personality disorder were resistant to treatment and were assessed by using of check list Frequency of behavior- researcher made.
Results: The finding yielded that criteria of sadness, anxiety and restlessness and feeling of absurdity, in evaluation was performed by families to examine the possible changes, after ECT therapy decreased compared to baseline. As well as after ECT therapy verbal and nonverbal expression of affection criterion represents an increase compared to baseline.
Conclusion: According to the findings Electroconvulsive therapy can affect on mood symptoms associated in patients’ borderline.
Keywords:electroconvulsive therapy, borderline personality disorder, resistant to treatment
Borderline personality disorder is the most common personality disorder in psychiatric settings1 and today is one of ten classification of personality disorder.2 The prevalence of BPD in the general population is about one percent. Prevalence rate of this disorder in the general population is approximately 2%, and is estimated in the outpatient mental health clinics, approximately 10% and approximately 20% of patients in psychiatric wards. The scope of this disorder in the clinical populations suffering from personality disorders from is 30% to 60% and is more common in women.3,4 According to DSM-5, this disorder is characterized as "a pervasive pattern of instability in interpersonal relationships, self-image, mood impulsivity that begins in early adulthood and emerges in different situations and environments".3 Rul, Useda, Confort and Doan found that borderline personality disorder is associated with patterns of problematic mood, including uncontrollable anger and emotional instability.5 According to one study, 6.1% of adults in the United States of America during a year of study had borderline personality disorder.4,6,7
Most therapists who have faced in the clinical setting with patients with borderline personality disorder, agree with the fact that the treatment of these patients is difficult.5,6,8 Characteristics of borderline in old Psycho Analytic article and by individuals like Moore, Reich, Oberndorf, Glover, Kasanin and Fine observed and discussed,9 however the term "borderline" was used first time by Stern in 1938. Stern used this term to describe people who were on the border between neurotic and psychotic states; This means that patients who are under intense psychological pressure are affected to psychotic behaviors and thought processes and quickly returned to normal levels of mental function.10 Currently extensive epidemiologic research about BPD show that the clinical course of this disorder is not disappointing, as it was during the 1940s until the early 1990s.11 However, the rate of abandonment of treatment in them are very high and the improvement is variable12 and only a few of them respond to psychiatric drug treatment, education of interpersonal relationships and control critical behaviors.13 Most studies have focused on such treatment and have less attention on electroconvulsive therapy in treatment-resistant patients.
ECT is one of the oldest treatments that have been used in the case of mental illness that its history returns to sixteenth century.14 This method is used in the cases of patient does not respond to any drug treatment or cannot tolerate drug side effects or severe symptoms of psychosis and desire to commit suicide or homicide and the issues that need immediate treatment response.15,16 Also, it looks like a minor surgical procedure that requires a series of preparatory and primary health care.17 ECT is the electrical stimulation of the brain planned for the beginning of the seizure.18 Electrical stimulation resulted in a general tonic activity for about ten seconds and then continues to the general clonic activity for variable time (from several seconds to more than a minute). There is a general consensus on the fact that the duration of the seizure is a determining factor in the efficacy of ECT, but the general belief is changing recently.19,20 Because the 80% of patients with borderline personality disorder have behaviors and suicide attempts, and finally 4% to 9% of them die by suicide, and this is almost 50times higher than the mortality rate for suicide in the general population21,22 as well as other unsuccessful attempts and self-harm of these patients that often leads to maim, brings a huge burden on the healthcare system and family. Therefore put this disease one of the greatest challenges in psychiatry. Also if symptoms of personality disorder persisted a long time, leads to attention deficit in the performance of individual, social, employment and education. These, along with impulsive behavior, instability in relationships and emotional, with rapid changes in mood23,24 and in case of relapse and resistance to treatment routine, to prevent damage to the individual and society need to serious intervention. So we need to deal with the present study examines the effectiveness of ECT for such severe cases of borderline personality disorder.
Instruments
The instruments used in this study include the frequency of behavior checklist, made by the researcher and two-part that was based on the literature review. The first part of the frequency behavior of the checklist, is related to demographic (age, gender, marital status). In the second part 29 questions related to the recording of the frequency behavior, that frequency of behaviors recorded during a month by the family. Its validity was approved by two faculty members. Its reliability was confirmed by Cronbach's alpha coefficient (α ₌ 0/85) and after completion of the pilot 20 checklist by families.
Participants
This study is the type of observational studies, case reports and retrospective which was conducted between 2012 to 2013years in Section of psychiatric Lavasani Hospital at Tehran. The study populations were patients with diagnosis of borderline personality disorder that due to frequent relapses and hospitalization and lack of response to previous treatment, inability of their families in order to control them and have frequent conflicts with the legal system, have been diagnosed as resistant to treatment. Fifteen patients were selected for the sample group through available sampling. Ten patients up to full completion of the project was necessary and sufficient cooperation and five patients were excluded from the study for various reasons, including lack of cooperation with the health system and lack of regular follow up.
Procedure
For one month before the start of ECT, the families of the patients were trained to observe and record the behavior of the subjects and the frequency behavior in frequency of behavior checklist. As well as non-visible symptoms were recorded by interviewing the patients and their families at the end of this month. These frequencies were considered as the baseline. In the next step patients hospitalized in the psychiatric ward and received ECT, in addition to other treatments. Considering the condition of ethical research, after obtaining informed consent from families and do the necessary assessments before electroconvulsive, including examination of complete physical and neurological checkups, medical history of the patient, observation before anesthesia, performing laboratory evaluations include CBC diff, urine analysis, chest radiography, electrocardiography and after discontinuation of drugs that interfere with ECT, was used bilateral ECT under general anesthesia. After the ECT all patients were ventilated with 100% oxygen until the complete return of spontaneous breathing. During ECT patients were followed every week and after the achieve maximum therapeutic response (The order of maximum therapeutic response is after 2 consecutive ECT patient does not feel more improvement.) with conservative drug therapy that was similar in all of them, were discharged. During six months patients repeatedly experienced recurrence of symptoms which sometimes leads to hospitalization in psychiatric wards. But all of the patients were hospitalized only twice, with receiving ECT that during the twice hospitalized they received 24 sessions of ECT (every time during the one-month hospitalization, received 12 sessions ECT.) with the conditions described in addition to conventional therapy.
Since in this study, ECT were considered as experimental variables and change of signs at the end of six months assessed using the frequency of behavior checklist, therefore again asked from families of patients for a month to observe their patients signs and record the frequency of signs in frequency of checklist. Because it was necessary have passed at least one month since the last electroconvulsive to temporary Amnesia and cognitive impairment which is a common side effect of ECT, does not distort the results. Then again patients for six months were followed for recurrence and its relation to therapeutic response that this frequencies were considered as the second baseline (Research design ABA). After collecting data by using SPSS software were analyzed. Also, because the previous treatments for these patients was unsuccessful, can be considered the changes observed in the subsequent behaviors compared to baseline due to experimental variables (ECT).
Results
Demographic information (such as age and history of medications and underlying disease) was extracted from patients' hospital files. Information about the apparent Seizure (observed tonic and clonic contractions by psychiatrist) and the actual seizure (study ECG strip in terms of spike & sharp waves by psychiatrist) and hemodynamic variables by using Pulse Oximetry monitoring, non-invasive measurement of blood pressure and ECG monitoring by anesthesia technicians were collected and recorded in relevant forms. According to information obtained; Participants in the study were aged between 49-19years and the mean age of them was 32years old. In addition 6 patients (60%) were married, 4 patients (40 percent) were single. For entering the study, were considered criteria for subjects which including the following:
The exclusion criteria consisted of;
In this study data analysis method is descriptive. The results from checklist, related to before and after the experimental variable were compared with each other via charts. For each subject a graph was plotted and analyzed that in this graphs observed behaviors on the horizontal axis and the frequency related to them, was plotted on the vertical axis (Figures 1-4).
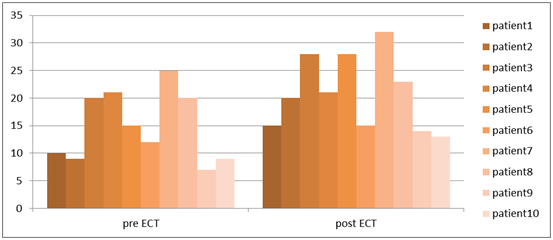
Figure 4 Comparison of frequency of criteria "verbal and nonverbal affective expression" before and after ECT.
According to the behavior of the subjects in checklist, frequency of behaviors indicate significant decline. However, some behaviors showed a more significant decline. As specified in the above graphs, Frequency of criteria "sad", "anxiety and restlessness" and "feeling of emptiness", among behaviors in the checklist, in each of the ten subjects after ECT has decreased compared to baseline. In addition among behaviors in the checklist the criterion of "verbal and nonverbal affective expression" represents an increase compared to the baseline (Figures 4).
The purpose of this study was evaluate the effectiveness of ECT in borderline personality disorder resistant to treatment. The results of this study showed that frequency of behavior in all criteria was significantly reduced, however, it is different amount of this reduction from one patient to another and from behavior to another behavior. But it is clear that all subjects showed varying degrees of response to treatment. In all ten subjects criteria of sadness, anxiety and restlessness, feeling of emptiness among behaviors in the checklist after ECT was lower from baseline and this indicate electroconvulsive therapy was effective in improving mood symptoms and reduce anxiety. According to the results it can be said that electroconvulsive therapy, according to results of previous research decreases mood symptoms associated with depression and anxiety in people with borderline personality disorder.25‒27 To explain these findings can be noted to the following factors:
However, inconsistent with findings that suggest ECT effect on along mood disorders in patients borderline 25,27 Farmer et al. 28 claimed the simultaneous presence of borderline personality disorder and depression, reduces the response to ECT.
Finally, with regard to the above issues and the goals of study was looking for, it can be said ECT can affect on mood symptoms in patients borderline. On the other hand since currently does not exist a study that examined the effects of ECT on patients suffering from personality disorders and personality traits, and the few studies have assessed personality (using personality assessment tests) before and immediately after completion of treatment with ECT sessions, believe that ECT clearly does not effect on personality traits18 But eventually a general look at the collection of symptoms and behavior, and changes can be considered as criteria for evaluation of the effectiveness of a therapeutic approach.
The limitations of this study; was small sample size and drop in the number of samples. In addition, because the study is an experimental design within the group and the sample is not representative of population, so there is no possibility of generalizing the results. Also for that further to realize to effectiveness of ECT in the treatment of patients with borderline personality disorder, long-term follow-up is recommended to be done about the outcome of treatment.
None.
Author declares there are no conflicts of interest.
None.

©2016 Baniasad, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Eating Disorder Week is observed from 23 February 2026 to 01 March 2026 to increase awareness of eating disorders and their psychological impact, and to promote early intervention and recovery. This initiative highlights the role of psychology and clinical psychiatry in understanding and treating eating disorders.
Researchers are encouraged to submit relevant research articles, reviews, and clinical findings. Submissions received during this week will receive a 30–40% publication discount in the Journal of Psychology & Clinical Psychiatry (JPCPY).
.
World Eating Disorder Week is observed from 23 February 2026 to 01 March 2026 to increase awareness of eating disorders and their psychological impact, and to promote early intervention and recovery. This initiative highlights the role of psychology and clinical psychiatry in understanding and treating eating disorders.
Researchers are encouraged to submit relevant research articles, reviews, and clinical findings. Submissions received during this week will receive a 30–40% publication discount in the Journal of Psychology & Clinical Psychiatry (JPCPY).
.