Journal of
eISSN: 2373-6445


Case Report Volume 9 Issue 5
1Department of Neurology, Mohamed V University, Morocco
2Department of Psychiatry, Mohamed V University, Morocco
3Department of Ophthalmology, Mohamed V University, Morocco
Correspondence: Youssouf Benmoh, Department of Neurology, Mohamed V Military Teaching Hospital, Mohamed V University, Rabat, Morocco
Received: August 14, 2018 | Published: September 5, 2018
Citation: Benmoh Y, Alaoui YM, Zaoui K. Cognitive decline and swiss cheese aspect revealing temporal radionecrosis after nasopharyngeal carcinoma radiation therapy: case report and literature review. J Psychol Clin Psychiatry. 2018;9(5):437?440. DOI: 10.15406/jpcpy.2018.09.00566
Background: The radiation therapy effectiveness is certain in naso-pharyngeal carcinoma (NPC) and other head and neck malignancies. In this context, cerebral radionecrosis (CRN) is a late radiotherapy related-side effect. Its incidence is above 5%, when the total dose is less than 60 grays, and the fraction size less than 2 grays. We report a rare case of late cerebral radio necrosis , its clinical manifestation, MRI specific aspect compared to its main differential diagnosis (brain metastatic tumor), and the evolution under specific treatment, with a review of reported cases over the literature.
Case report: 53 years-old man, diagnosed for having nasopharyngeal carcinoma, and was treated by chemotherapy and external radiotherapy. 6 years after later, he presented progressive cognitive decline with phasic and mnesic complaints, associated to balance disorder. Clinical examination objectified dementia detected by Montreal Cognitive Assessment (MoCA) score, with normal Mini Mental State (MMS), associated to pyramidal and vestibular syndrome. Cerebral MRI showed swiss cheese and soap bubble aspect in left temporal lobe, and spectroscopy showed decreased creatinine and N-acetyl-aspartate peak. He was treated as having temporal radio necrosis by hyperbaric oxygen, corticotherapy and anti-platelets. His clinical and radiological condition improved.
Conclusion: We learn that cognitive decline may be the revealing symptom of cerebral radio necrosis. In this case, MoCA test showed more sensitivity. Thus clinician must bear in mind the risk of cerebral radio necrosis (CRN) as much as metastatic or recurrent brain tumor in such situation. The MRI with specific pattern could help in distinguish these entities. Corticosteroid associated to hyperbaric oxygen and anti-platelets improve the course of CRN. The use of promoting agent anti-VEGF Bevacizumab should be clarified by more prospective studies.
Keywords: cerebral radionecrosis ; Swiss cheese; Soap bubble; nasopharyngeal carcinoma; Montreal Cognitive Assessment, Dementia
New strategies have been developed for the improvement of the outcome of head and neck treated cancer, concerning the delivery of radiotherapy, with concomitant chemotherapy, or altered fractionation schedules.1 Nevertheless, an increasing interest stay showed to these treatment-related side effects and their impact on the health related quality of life. Paradoxically the advent of novel treatment protocols is associated to increasing morbidity related to preservation of the organ anatomy without its function, thus many patients were dealing with devastating side effects such as severe swallowing dysfunction, aspiration and speech disorders.2 For these considered reasons, advances were made in radiotherapy, such as intensity-modulated radiotherapy. This technique permits to oncologist to deliver high dose radiation to head and neck tumor with its adjacent high risk area, with concomitant reducing dose radiation for the organs at risk. We report a rare case of late cerebral radio necrosis , its clinical manifestation, MRI specific aspect compared to its main differential diagnosis (brain metastatic tumor), and the evolution under specific treatment, with a review of reported cases over the literature.
53 years-old man in good health, had a previous history of monocular traumatic amaurosis. In 2008, he was diagnosis as having a nasopharyngeal cancer. He was treated by chemotherapy then 33 courses of external radiation therapy, delivering 2 grays in each one. The evolution was favorable with loco-regional tumor control, apart from sequelar bilateral hypoacusis under hearing aid. 6 years after, he presented rapidly progressive symptoms evolving 15 days before his admission. He reported dizziness, with balance disorder, associated to mnesic complaints interesting the verbal memory. He also remarked phasic disorders with difficulties in finding the right words. There was no sign of intracranial hypertension, seizure, fever or other extra-neurological symptoms. Clinical examination found consciousness patient, oriented in space and time, with stable hemodynamic parameters. The neck was supple, with no paresis but a right Babinski. The Romberg was positive and lateralized to left with horizontal nystagmus, bilateral hypoacusis, and right monocular cecity. The mini-mental state examination (MMSE) showed no abnormality, nevertheless the Montreal Cognitive Assessment (MoCA) score was 24/30, with three lost points in memory, two points in attention study and one point while naming. The somatic examination showed no other abnormalities. The clinical syndrome was pyramidal irritation, with dementia and left vestibular syndrome.
The cerebral MRI showed heterogeneous decreased signal intensity in T1, T2 and Flair-weighted images with variable sizes, surrounded by large area of increased signal intensity in T2 and Flair weighted-images with mass effect on the ipsilateral ventricle (Figure 1). The T1 sequences with intravenous gado injection showed heterogeneous gado enhancement corresponding to the area withT2 and Flair decreased signal intensity (Figure 2). This pattern corresponds to the “swiss cheese” and “soap bubble” aspect. The diffusion weited image showed increased ADC with increased water mobility in left temporal lobe (Figure 3). The radiological conclusion was temporal radionecrosis with large vasogenic edema, or the differential diagnosis of cerebral metastasis of the primary nasopharyngeal carcinoma. Thus, a spectroscopy was performed, and showed decreased peak of N-Acetyl-Aspartate (NAA) and Creatinine (Cr), with normal choline peak. The diagnosis of temporal radio necrosis was established. The patient was proposed to hyperbaric oxygen. His Oto-rhino-laryngeal examination was normal, as much s the chest X-ray. So a daily 45 minutes session, were performed for 10 successive days, associated to bolus of methylprednisolone (240mg/d for 10 days), anti-platelet agent (aspirin 160mg/d). The evolution was favorable, with regression of vestibular signs, improvement of memory and phasic troubles with recovering four lost points in MoCA score. The cerebral CT scan showed partial regression of the gliosis with no more mass effect on the ipsilateral ventricle (Figure 4).
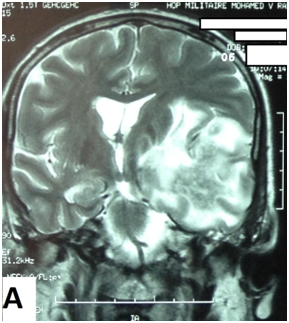
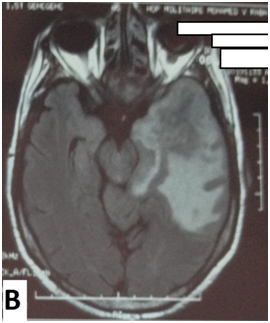
Figure 1 Cerebral MRI in coronal T2-weighted image (A) and axial Flair-weighted image, showing heterogeneous decreasing signal intensity with variable sizes corresponding to necrosis area, surrounded by increased signal intensity corresponding to peri lesional edema with mass effect on the ipsilateral ventricle.
The radiation therapy effectiveness is certain in naso-pharyngeal carcinoma (NPC) and other head and neck malignancies. Knowing the close proximity of inferior and medial temporal lobes to the irradiation field, radiotherapy-related brain damages may occur, especially that the radiation dose is above 65 grays, exceeding the tolerance of the brain tissue. These damages are subdivided to three subtypes related to time of presentation: 1-acute effects (acute encephalopathy during or rapidly after radiation),3 sub acute or early-delayed (somnolence syndrome in up to 12 weeks after radiation)4 and late (months to years after radiation).5 The late effects include radio necrosis, lacunar infarct, parenchyma calcification and white matter changes. Their incidences vary depending on other variables such as concurrent chemotherapy, total dose, fraction dose, time between fraction, the treatment volume, age, arterial hypertension or diabetes and TNM tumor status.6 Radio necrosis incidence is above 5% when the total dose did not exceed 60 grays, and the fraction daily size less than 2 grays.7 The first case of cerebral radio necrosis in extra cranial malignancy was described by Fischer and Holfelder in 1930.8 Nowadays, hundreds cases were reported over the world, where the most common site of malignancy is the nasopharynx followed by the scalp and the sinonasal tract.9 In 80% of cases, the diagnosis of cerebral radionecrosis is established within the 3 years after the last dose of radiotherapy.10 In our patient, this period was 6 years. Three hypotheses sustain radio necrosis mechanism: on one hand the vascular hypothesis suggest endothelial cell damages with extracellular edema and cytokine release leading to demyelination and necrosis. On the other hand the, the glial hypothesis suggests a high sensibility of glial and oligodendrocytes cells to radiation, leading to their direct damages with parenchyma atrophy. The third recent mechanism suggests a host’s immune response with mediation by pro-inflammatory cytokines.11,12 Cerebral radio necrosis symptoms are wide variable and latent. The most common are consciousness changes, seizures, vertigo, dizziness, irritability or memory impairment. In front of such neurological or psychiatric signs, encephalopathy must be ruled out before considering cerebral radio necrosis.10 Patients with temporal radio necrosis have more significant change in their cognitive function, reflected in short-time memory, language, attention, delayed recall, orientation, and executive function. MMSE and MoCA are widely known to evaluate general cognitive function.13 As in brain tumor patients, MoCA has been documented for having more sensitivity in objectifying the decline. This was due to its large screening demanding more assessment of memory, information speed treatment, executive function, attention, new learning and visuo-spatial function.14 In our case, the MMSE was normal, time that MoCA showed cognitive impairment while exploring memory, naming and attention. Thus, we recommended using MoCA as a standard cognitive scale to detect impairment in patients treated with radiotherapy for head and neck cancer. Moreover, temporal radio necrosis causes neuropsychiatric troubles, dominated by irritability, anxiety and depression. Our patient showed no abnormality, using the Hamilton depression scale (HAMD), and Hamilton anxiety scale (HAMA). The real challenge is to distinguish cerebral radio necrosis (CRN) from cerebral metastatic or recurrent tumor (CTM). For this aim, magnetic resonance image with apparent diffusion coefficient (ADC), perfusion imaging and spectroscopy studies showed enough arguments to avoid recourse to surgery with extensive pathological evaluation.15 Typical MRI aspect in gado T1-weighted image is called “Swiss cheese” or “soap bubble”. These two patterns refer to heterogeneous non-enhancing zones inside the area of contrast enhancement (soap bubble), associated to various sizes of necrotic scattered areas (swiss cheese). The second pattern is the increased water mobility in radiation necrosis leading to increase ADC, which did not exist in metastatic or recurrent brain tumor.16\ For spectroscopy, decreased creatinine (Cr) and N acetyl aspartate (NAA) peak are more suggestive of cerebral radionecrosis rather than cerebral tumor where choline (Cho) peak increased. Thus, the Cho/Cr and Cho/NAA are good landmarks to distinguish cerebral radio necrosis from tumor.17 The last argument is the hypoperfusion in CRN, contrasting with hyperperfusion in CTM. The use of PET with 18-FDG or amino-acids is still controversial. Our case illustrates the swiss cheese and soap bubble pattern, concordant with decreased NAA and Cr peak. Concerning therapies, corticosteroid (intravenous relayed by oral therapy) showed enough effectiveness in CRN. This therapy reverses the breakdown of blood-brain barrier with anti-inflammatory and anti-edema action.18,19 Hyperbaric oxygen, anti-platelets and anticoagulant have been used to repair microcirculation and regional blood supply caused by radio necrosis.20,21 An over expressing of Vascular Endothelial Growth Factor (VEGF) was remarked in radio necrosis, and was targeted by humanized murine monoclonal antibody named Bevacizumab. It appears to be a promoting agent against CRN. Nevertheless, the optimal scheduling and treatment duration have not been yet established.22 The recourse to surgery in CRN should be leaded carefully and strictly, and medical treatment should be more used in its stead.
We learn from this case that CRN is late complication of radiation relayed side effects. Its manifestation could be mainly cognitive decline, where MoCA showed more sensibility for its diagnosis. Thus clinician must bear in mind the risk of CRN as much as metastatic or recurrent tumor in such situation. The MRI with specific pattern could help in distinguish these entities. Corticosteroid associated to hyperbaric oxygen and antiplatelets improve the course of CRN. The use of promoting agent anti-VEGF Bevacizumab should be clarified by more prospective studies.
None.
The author declares that there is no conflict of interest.

©2018 Benmoh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.
 World Eating Disorder Week is observed from 23 February 2026 to 01 March 2026 to increase awareness of eating disorders and their psychological impact, and to promote early intervention and recovery. This initiative highlights the role of psychology and clinical psychiatry in understanding and treating eating disorders.
Researchers are encouraged to submit relevant research articles, reviews, and clinical findings. Submissions received during this week will receive a 30–40% publication discount in the Journal of Psychology & Clinical Psychiatry (JPCPY).
.
World Eating Disorder Week is observed from 23 February 2026 to 01 March 2026 to increase awareness of eating disorders and their psychological impact, and to promote early intervention and recovery. This initiative highlights the role of psychology and clinical psychiatry in understanding and treating eating disorders.
Researchers are encouraged to submit relevant research articles, reviews, and clinical findings. Submissions received during this week will receive a 30–40% publication discount in the Journal of Psychology & Clinical Psychiatry (JPCPY).
.