Journal of
eISSN: 2373-6445


Research Article Volume 9 Issue 6
Department of Psychology, University of Occidente, Mexico
Correspondence: Jorge Alexandro Benitez Contreras, Department of Psychology, University of Occidente, Mexico, Av del Mar 1200, Flamingos, 82149 Mazatlan, Sinaloa, Mexico
Received: October 13, 2018 | Published: December 20, 2018
Citation: Contreras JAB, Loera MRC. Analysis of the implementation of psychosocial rehabilitation and its development in patients with schizophrenia. J Psychol Clin Psychiatry. 2018;9(6):696 ? 703. DOI: 10.15406/jpcpy.2018.09.00619
Schizophrenia, for many years, has been taken as one of the incurable diseases of importance, mainly due to its worldwide prevalence and in its particular early onset, chronicity and relationship with personal, labor and social disabilities. The main objective of the study was to perform an intervention to patients with schizophrenia, from the model of psychosocial rehabilitation and describe the impact generated in their social, personal and work life and those around them (family, neighbours, people with whom they are forced to cross on a daily basis, etc.), to define the susceptibility and feasibility of success in Morelos and Mexico society. The methodology used was a qualitative approach, with exploratory and descriptive scope, following the cognitive-behavioral current. The interviews and observation were the techniques used for the data collection supported in the log (field journals), the Valencia et al.1 scale and reports at the end of each module of the intervention together with the criteria and assessment of the team of health with which the project worked in the health center. The results of the research indicate that patients diagnosed with schizophrenia and who attend a process of psychosocial rehabilitation considering areas such as work, social, economic, sexual and family, which show significant changes in their conduct and behavior mainly in family and work. In conclusion, in the present work it was found that a method that favors the improvement of quality of life is the model of psychosocial rehabilitation, where the patient works from a multidisciplinary perspective, different areas and levels of their person to achieve a better expectation from a personal, cognitive, work, social, economic, sexual, family and group aspect.
Keywords: schizophrenia, psychosocial rehabilitation, cognitive-behavioral
Serious mental disorders (SMI or TMG for their initials in Spanish) such as depression, autism, bipolarity, schizophrenia and other types of psychosis, suppose differential levels of clinical involvement and psychosocial performance, involuntary internment in units of prolonged psychiatric care is the therapeutic alternative more appropriate to ensure intensive treatment of the deficits generated by the mental disorder. However, these units have been historically related to the genesis of chronicity and to the progressive increase in the difficulties of social reintegration, including authors such as Muñoz & Manzano2 where they mention that the key to minimizing these risks and maximizing the possibilities of rehabilitation is to introduce measures such as, for example, creating environments that are as close as possible to the natural environment, compartmentalizing the units and/or favoring individualization. The World Health Organization,3 WHO by its initials, has estimated that there are more than 21 million people with schizophrenia in the world and that the majority live in less developed countries. In Mexico it has been reported an approximate number between 500,000 and 700,000 patients with schizophrenia, where new cases range from 2.4 to 5.2 per thousand inhabitants, that is, each year increases the figure between 0.24 and 0.52% and where about 32% of patients hospitalized in hospitals in Mexico, had a schizophrenia diagnosis.4,5 Due to the nature and chronicity of the disease, patients need to take lifelong medications, as well as receiving some form of intervention other than pharmaceutical to improve their Psychosocial functioning (FPS for their initials in Spanish) to reduce the number of relapses as well as improve personal, family and social relationships.5 For the clinical psychology and for the psychotherapy of patients with schizophrenia, it is of vital importance to consider the use of the medications since only when the patient is clinically stable can one intervene psychotherapeutic level, therefore the drugs included in the Pharmacological treatment are part of the fundamental basis of treatment, which must be complemented with other types of therapeutic interventions. In the last fifty years, an endless number of therapeutic modalities have been developed for this type of patients, among them a great diversity of therapies, treatments or psychosocial interventions.6–16 It was found that in Mexico and Latin America there are few controlled studies comparing the effectiveness of any therapeutic modality in patients with schizophrenia. Therefore, in the present investigation, results of the work are presented in patients with psychiatric diagnosis of schizophrenia of the Centro Integral de Salud Mental (CISAME) in Cuautla, Morelos, Mexico considering the psychosocial rehabilitation from a cognitive-behavioral approach, which included a total of three workshops that were carried out during the course of ten months in which the relevance of psychosocial rehabilitation was identified.
This study was of a qualitative nature with exploratory-descriptive scope. The sample was for non-probabilistic convenience. The exploratory study was carried out with the objective of examining a little-studied research topic or problem, which has been studied in a limited way; descriptive studies specifies the properties, characteristics and profiles of people, groups, communities or any other phenomenon that undergoes an analysis. It was decided to use the qualitative approach since this perspective seeks to understand the perception of participants (patients) about the phenomenon that surrounds them (schizophrenia and its rehabilitation). Also, it was used since "it is advisable to select the qualitative approach when the subject of study has been little explored, or research has been done in a specific social group, in a scant way".17 With the exploratory scope, the aim was to examine the problem and clarify doubts about the effects of psychosocial rehabilitation in patients diagnosed and treated for schizophrenia. This helped as the exploratory scope serves "to prepare the ground for future research",17 therefore, it will create a familiarity with the phenomenon and the type of intervention to be used, creating the possibility of identifying promising variables, future priorities and definition of viable concepts and practices within the socio-cultural context. On the other hand, the study had a descriptive scope because it sought to specify properties, characteristics, processes own that arose from the exploration of the technique to be employed in the designated group.17 Being a descriptive study, he limited himself to determining the dimensions of the features found (schizophrenia before psychosocial rehabilitation) and then describing them. The present investigation was carried out following the cognitive behavioral current (also known as emotive behavior or CBT) under the principles of a psychosocial treatment in the Centro Integral de Salud Mental (CISAME) in Cuautla, Morelos, Mexico where there were individuals previously diagnosed with schizophrenia and who are currently incarcerated in said institution taking into account that they are not carrying out at the time, any type of psychosocial rehabilitation technique.
Twenty-three people with a previous diagnosis of paranoid schizophrenia participated, who receive treatment and are treated at the CISAME in Cuautla. As inclusion criteria, it took people with a diagnosis of schizophrenia who are in established and consolidated treatment, which have been channeled and are registered in CISAME Cuautla. On the other hand, as an exclusion criterion, patients who abandoned partial or complete therapy (must meet 80% of attendance at the sessions), were not enrolled in CISAME in Cuautla or did not meet the TMG criteria of schizophrenia together with its established and consolidated treatment previously given. As an instrument to support the study, it was decided to use the psychosocial intervention model, which is made up of two important characteristics:
The Psychosocial Functioning Scale instrument was used,1 which serves to evaluate the treatment and finally, describe the results of patients treated by the same researcher.
Psychosocial functioning was evaluated through five areas of operation:
Finally, psychosocial functioning was evaluated through the levels of psychosocial functioning that the patient reports in a continuous satisfaction-dissatisfaction, with respect to their role performance.18 The scale of psychosocial functioning is made up of two sections. An informational that includes sociodemographic data, housing conditions and family composition and an evaluation that allows assessing the functioning of the patient in the five areas mentioned above. The scale includes 64 items: 7 in each area and a rating system that includes 5 levels of operation:
The scale was designed in the Division of Epidemiological and Social Investigations of the Mexican Institute of Psychiatry by Valencia, Rojas, González, Ramos and Villatoro (1989) and has a high degree of validity and reliability for use in Mexico. The scale can be applied by an interviewer previously trained in its management through a direct interview with the patient. The application time is approximately 30 to 45 minutes. The duration of the intervention program was ten months, with a frequency of one weekly session, considering subprograms as follows
The intervention was carried out in groups, as an optimal size of five to twenty-five users. The program has a hierarchical and sequential development. It was found optimal and, therefore, it was recommended that the cognitive differentiation exercises be maintained for the following modules to achieve an over-learning of basic cognitive strategies. Likewise, the exercises and tasks related to the daily memory module were introduced from the initial moments of the program. The frequency of team meetings depended on the degree of development and maturity of the team and patients (in no case was less than one weekly meeting). Interprofessional coordination spaces were also created among the different workers. The sessions had a duration of five to six hours following an approximate structure like the one shown below:
O'Brien,19 indicates that it is not convenient to look at the therapy, the unconscious aspects of the patient, so it is not necessary to use psychodynamic approaches that include interpretations and that lead to unnecessary confrontations. The therapy must be oriented "to the here and now" of the patient's life, as proposed by Malm20 providing a "healthy social group experience".
This section explains how twenty-three people with a previous diagnosis of paranoid schizophrenia participated, who receive treatment and are treated in the Centro Integral de Salud Mental (CISAME) in Cuautla, Morelos. With respect to the application of the Valencia et al.1 tests it was found that those participants who met all the inclusion criteria established in the study showed a different perception within their areas, changing their behavior, perception and, mainly, the style and quality of life in which the patients were. We measured, according to the tests, the five main areas in which the affected patient is located, demonstrating in such a way the change in their behavior and the impact on their lives according to the results obtained. The work area showed that, in spite of perceiving it as satisfactory, not only was this position maintained at the end of the investigation but, unlike the beginning, they were able to explain and justify their level of satisfaction instead of just relying on monosyllabic responses like “yes” and “no”. This represents, to a certain extent, that patients were able to maintain their work and improve their performance in it thanks to the knowledge and skills developed during the course of the intervention, allowing the subject to understand their limits and abilities as well as to potentiate the necessary skills for the understanding of their current situation and the possible repercussions, and importance, in the future for themselves of those around them. Therefore, the fact that they could measure their own context in the work area allowed some measure to use it as an occupational therapy, at the same time as developing (or obtaining) tools that allow the patient a better adaptation to the environment that surrounds him, fostering social and work relationships, in addition to the sense of commitment and importance of having and maintaining a job for his own personal and family well-being. It should be emphasized that these same patients are the ones who expressed, understood and could explain the reason why this area is necessary in their life. Therefore, it was found that in the work area, patients 1001, 1011 and 1012 (who met all the inclusion criteria of the research) are those who represent the changes in the work area in this way mentioned above (Figures 1−6).

Figure 1 Level of psychosocial functioning of the work area of patients with more than 80% of attendances.
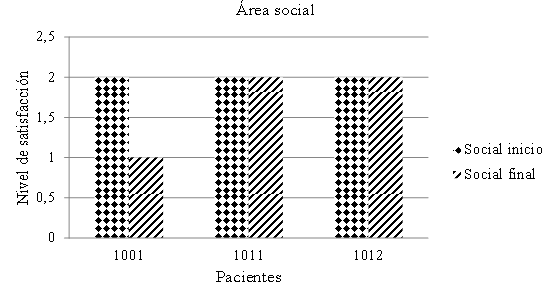
Figure 2 Psychosocial functioning level of the social area of patients with more than 80% of attendances.

Figure 3 Psychosocial functioning level of the economic area of patients with more than 80% of attendances.
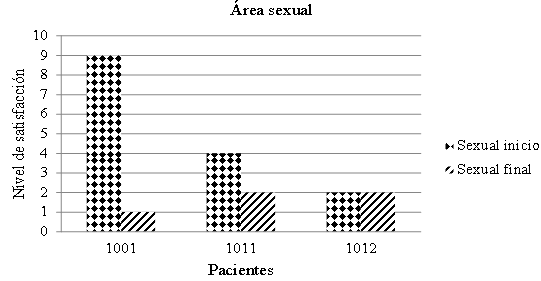
Figure 4 Psychosocial functioning level of the sexual area of patients with more than 80% of attendances.
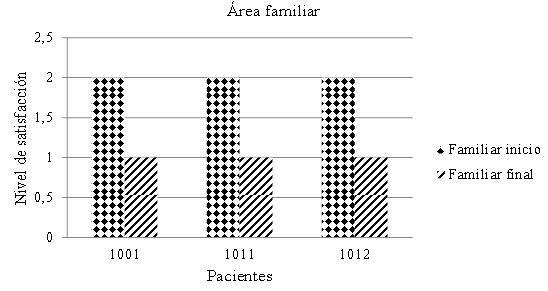
Figure 5 Psychosocial functioning level of the family area of patients with more than 80% of attendances.
From the field of health, one of the aspects derived from the increase in life expectancy that most concerns both the aging individuals themselves and those responsible for the planning and management of resources is the increase in the number of people who present progressive losses of functional capacity and come to need care and long-term care. Perhaps, of the situations that ends in the loss of personal independence, one of the most alarming are the degenerative brain diseases that cause cognitive deterioration syndromes or dementia, such as schizophrenia. The severity of the disabilities that these illnesses provoke in the person must not be ignored, which is immersed in a progressive deterioration of their mental and physical faculties due to the deterioration and lack of stimulation caused by the symptoms of schizophrenia, as well as in a progressive need for care, which has been provided exclusively by their family or legal guardian. It is necessary to take into account, on the other hand, a new phenomenon that, not because it is emergent, must be reduced in importance, both in its qualitative and in the quantitative dimension. It is about the number of people with intellectual disabilities who have also seen their life expectancy lengthened and who begin to experience, at a younger age than the rest of the population, demential processes.
That said, patients, as well as their families, have noticed a difference in motivation and the perception to develop their daily activities with greater ease and fluency, allowing a continuous and positive development in the evolution of their independent cognitive functions. In addition, the same patients have been able to use functions of a greater degree of concentration, which are reflected when making decisions, obtaining and maintaining a job, planning their own future, organizing their ideas and behavior in an appropriate manner and even, to have a better awareness of the disease by creating different methods of coping with the symptoms of schizophrenia. In the same way, it was found in common, mainly with the health personnel of CISAME, that the structure, method and diverse and specific activities were what caused the significant change. The conditions to affirm that schizophrenia is not a natural disease but cultural and historical are not comprehensible without posing a history of subjectivity. Each patient presents a completely different life story, which creates a different perception of what the pathology is, how it is lived, the attachment to the treatment and the effects that they have had during the course of their life after having started with the symptoms and be diagnosed correctly. Whatever the case may be, the importance of schizophrenia and its evolution in each patient must be highlighted because it is part of its history, no other person or patient will have the same history, much less the same development of life. More importantly, it is worth noting that not knowing the exact cause of this pathology is a primary factor in why all aspects of the patient should be included in what the disease is and how it is taken from his perspective and from those who surround. That is why, within what was observed during the intervention, it is stressed how cognition affects affectivity, perception and other aspects of behavior in such a particular way. Therefore, the clinical picture presented by these people tends to be characteristic and specific, both with positive symptoms and negative symptoms, which can be chronic and easy to identify; this altering everything that is related to his life and that of those around him. In other words, we speak of people to whom each relapse causes a subsequent deterioration with high possibilities of inability to recover the normal level of activity, a higher level of vulnerability to permanent stress, probability of prolonged hospitalization and approximately one third of his life will live only in a "normal" way. Within the present work, it was found that both the patients and their respective relatives created a higher level of awareness regarding the disease, being able to create a better attachment to psychiatric treatment and, on demand of all, understanding the importance of having a multidisciplinary work where other aspects could be worked apart from pharmacological treatment. However, patients still have side effects due to the medication but this has not been a factor in stopping their activities, but rather, thanks to the development of their other areas worked during the sessions, it has served as motivation and they have been able to create strategies for a positive development towards the evolution of the pathology. It is important to emphasize the value and difference between those patients who attended constantly and those who were not regular in the sessions. It is evident that patients, having a diagnosis of schizophrenia, are faced with a life-long situation, that is, a chronic pathology in which psychiatric treatment and intervention will be needed for life. Therefore, as mentioned above, the evolution presented by each patient will be unique and individual, so the treatment was carried out according to the moment of the patient's evolution that, from a psychiatric perspective, could be: psychotic episode, interepisode without residual symptoms, interepisodic with residual symptoms and of continuous evolution. It was of the utmost importance to work in coordination with the psychiatrist, who referred and channeled patients who did not present positive symptoms or a history of violence, thus allowing them to approach and work with them in an appropriate manner. A determining factor for psychiatric therapy to have optimal results is the attachment to treatment, which is usually complicated in this type of population for multiple reasons, among them: economic, family support, possible psychotic outbreaks, among others.
One of the objectives of this research is to improve the functionality of the patient, it is the reinsertion into the society of the subject, and however the exclusive use of medication does not always achieve this result and, contrarily, can become a constant pattern where the patients do not present the positive symptoms but their life is governed by the negative symptoms and the monotony of the routine and absolute dependence to the psychiatric therapy and the pharmacological treatment. Therefore, the major challenge for psychiatry is not only limited to the technical aspects of the disease, but also to the contemplation of all aspects related to the condition, from prevention to social reintegration. However, patients and family members explain how, despite having psychiatric support and medication, it has not always been enough for them to have a favorable evolution and adherence to treatment. They have gained a better understanding of the importance of having psychiatric treatment but, at the same time, they have realized that there are other options that favor their situation and, in addition, allow them to develop skills and obtain tools that they cannot always obtain only of psychiatric intervention. This does not mean that the medications are not useful, but on the contrary they accept the reality of what is the pharmacological treatment, expressing that it is a starting process to generate an initial sensation of well-being but, as part of the suffering, it can be something that also encourages isolation and sedentary lifestyle by aggravating the negative symptoms present in schizophrenia (and even, in some cases, due to side effects of pharmaceutical treatment), therefore it was satisfactory for them to know that the medication works but that it generates better results when it receives support from other areas of health such as psychology, nursing and social work. Therefore, in the mental health care of people with psychotic disorders, the development of psychosocial interventions is necessary. In recent years, several controlled studies have presented cognitive behavioral therapy as a promising intervention in the treatment of schizophrenia. This therapy assumes that emotional problems are a consequence of non-adaptive learning, therefore interventions try to establish adequate behavior patterns, aiming to improve coping mechanisms that develop skills to deal with stressful situations and symptoms; and methods of cognitive restructuring. Even being the medication, mainly the neuroleptics, a treatment of first choice in schizophrenia and other psychotic disorders, presents a series of limitations in order to offer an answer to the complexity and heterogeneity of the problems and needs of the people who present these diagnoses: The psychiatrist is forced to prescribe different modalities and combinations of medications, sometimes by trial and error, until the patient responds positively by a reduction in the severity of the positive psychotic symptoms, often undesirable side effects appear of the medication, many patients do not present an adequate adherence to the prescribed treatment, circumstance that is related to an increase in the probability of the appearance of new psychotic episodes. On the other hand, an adequate adherence to treatment does not guarantee the disappearance of the residual psychotic symptoms, each psychotic episode is associated with an increase of the residual positive symptoms and the deterioration of the social functioning of the patient, an adequate compliance of the pharmacological treatment does not constitute sufficient guarantee that relapse will not take place and is not the therapy of choice to improve personal competence and social functioning, among others. It should be noted that within the study, all patients managed to link the objectives of each session with their current situation according to the context of the schizophrenia disorder and how and why it is necessary and beneficial to have this type of care at the same time with psychiatric therapy. The disadvantage is that both staff and patients would like to continue with the psychological process, however, there are no staffs or specialist in the area who can continue with this task, creating a demand from patients and family members for the continuation of psychological therapy, both for them and for the respective family members.
In the same way, it is imperative to highlight that in the CISAME of Cuautla, psychological care is available for all patients, but due to the very nature of the work environment, that is, accessibility of patients to attend therapies, timetables and available spaces for the sessions, trained personnel, among other reasons, it is necessary to remember the value and importance of a continuous treatment. The professionals who work in mental health, mainly those who have direct contact with patients and their families, should have and develop a set of specific skills that, perhaps working in other health areas, would not be the main thing, but all the professionals dedicated to taking care of the health of the people must take into account their profile and of which they should never forget and continue the practice on a daily basis. What is tried to emphasize is the fact that the worker within the unit must have the skills and psychic maturity to be able to offer a quality, efficient and reliable service. On the other hand, you must also have the corresponding preparation and studies to provide the necessary care and support required by the patient who enters the unit at the time they have interaction with any of the staff. So, under ideal conditions, the unit should have a program or type of training that it is constant to know how to adapt to the situation at hand, should receive some type of training during the time you are working in the unity. Within what was studied during the intervention it was discovered that on the one hand, the staff is aware of the necessary characteristics and the effort required to be able to fulfill their tasks in a pleasant and helpful way, creating a healthy work environment and attention that undoubtedly, helps the patient and family member to feel welcome and comfortable in the unit. On the other hand, the staff recognizes that it is necessary and requires greater preparation, training and scientific skills to help in the treatment, specifying the mode of intervention and care that is necessary to provide the patient.
In the present investigation, aspects related to psychosocial rehabilitation were analyzed in a group of patients with schizophrenia, in which their respective relatives also participated, who attended the scheduled sessions within the intervention project. Through interviews it was possible to intervene with this population, where the patient's background and the current status regarding evolution and adherence to treatment were known in patients diagnosed with schizophrenia, their respective family members and the workers of a health mental unit in the state of Morelos, Mexico to identify the benefits and problems experienced by each of the patients involved in the study on a day-to-day basis. The present investigation was carried out with the hypothesis that the relatives and, mainly, the patients who come for psychiatric attention to the Centro Integral de Salud Mental (CISAME) of Cuautla, Morelos for the diagnosis of schizophrenia, they would obtain positive results in terms of the reduction of symptoms characteristic of schizophrenia, through learning and meeting specific objectives per session would allow them to improve all their personal areas as well as an increase in the quality of life, decreasing the symptomatology and promoting a culture of continuous care and treatment for a better functioning and life prognosis. Regarding the group of people with whom it was working, differences could be observed. It was identified that due to the involvement in the activities, and the constancy in the intervention, allowed significant changes in an individual and group, considering the principles of psychosocial rehabilitation where it can be said that each patient had a level of evolution at different times always and when it has the interest and adherence to treatment, the support or indicated social/family network and a constant level of psychological development towards the improvement and reasons of the psychological and psychiatric treatment. Considering the above, these figures were used as a reference for analysis and comparison with those that did meet all the criteria and that have the possibility of being taken into account for future research. The work area was the one with the biggest changes, since the participants, at first, did not have a job because they thought they were unable to obtain/maintain it or because the family did not believe that "it was the right thing" or "to know if they were in their abilities to be able to work ". These reasons do not coincide with the reason expressed mainly by the patients and that the lack or low level of satisfaction in the workplace was due to the discrimination they suffered at the time that their potential employers knew about their current status, say that they had a clinical diagnosis of schizophrenia. It is identified the need to have different support programs for the job market for all patients (not only those with schizophrenia, but with any health problem in general) who are discriminated against or abused due to ignorance of the other subjects in society. Currently, according to the discourse of patients and staff of the health center, people from Mexico lives where the belief of the psychologist, psychiatrist or any special treatment that does not count "a normal person" is synonymous with "rarity" or “odd” and therefore, something different from what should be kept away from them by various individual beliefs. It is an arduous job that is still pending in the work area, where both patients and those who are in contact with them understand that they are able to continue to feel and grow, and therefore with basic needs (as well as special needs) like any other subject in life. The fact that they can have a job, develop in it and feel useful and productive again is a window of opportunity unmatched for them, and that should be addressed in other future research lines possibly with projects on awareness and maturity as people, families, society and small, medium and large companies that wish to obtain workers suitable for a given position, among other characteristics that will be discovered as work progresses in these areas.
Serious mental disorders, such as schizophrenia, represent a complex problem not reducible to simple psychiatric symptomatology, but generate alterations in other aspects of psychosocial functioning that result in different levels of involvement in community integration. The main objective of the research was to perform an intervention to patients with the diagnosis of schizophrenia from the model of psychosocial rehabilitation and describe the impact generated in their lives to be able to define the susceptibility and feasibility of treatment success in them. The results indicate that there are significant clinical changes regarding the level of satisfaction in different areas, mainly in the area of work and family, followed by the social and psychological areas, as well as an evolution and maturity in their person that is they were reflected in behavioral changes such as the reduction of the same negative symptoms of the pathology, as well as the perception in the patients, their relatives and the health personnel of the CISAME.
For the clinical psychology and for the psychotherapy of patients with schizophrenia, it is of vital importance to consider the use of medications since only when the patient is clinically stable can one intervene psychotherapeutic level, therefore the medicines are the fundamental basis of the treatment which must be complemented with other types of therapeutic interventions. It is evident the need to translate in a simple and clear way, the set of heterogeneous factors that influence the origin, development and/or manifestation of this serious mental disorder and that with this integration of data, the understanding, the causality, the objective diagnosis and optimal treatment, which allows the best approach to individuals with schizophrenia, achieving greater integration and attention to families, society and all those around the individual, increasing the commitment and awareness of the state in which the subject is found. With the program of intervention carried out, the subject was sought to recover or build meaningful social relationships in all its spheres, where according to the results one can interpret a greater improvement in the social, family and work areas, which will give priority to either to get a job or learn different ways to establish a relationship and / or friendship and that can maintain it. Considering the above, the conclusions of this investigation addresses the case of intervention in patients diagnosed with schizophrenia who were implemented a model of psychosocial rehabilitation with which it was sought to transform the patient's behavior, for the improvement of their life not only from the psychiatric or pharmacological perspective, but also psychosocial. This means that the effort of all the changes and modifications in the behavior of the patient, as well as the possible emotional stability, was mainly due to the integral treatment that was implemented during the research where they had a space in which they were able to know and learn social skills, and emotional regulation to promote their personal and social development, improving their social perception as well as a vision of cognitive development with awareness of the psychological functions involved for the organization of general and specific ideas and concepts in society, providing the patient with greater impulse control and emotional control developed by a higher level of consciousness regarding their own body, their behavior and elements of intrapersonal and interpersonal communication. The results of the study indicated that patients who met the rehabilitation assistance criteria showed significant changes in their behavior. Considering the above, it is possible to infer that those patients who fulfilled all the criteria of the investigation, are patients who, on the one hand, have other people who depend on them and, on the other, since the beginning of the rehabilitation had employment, being able to conclude that the fact of having dependents led them to keep a job, coinciding with the idea that having a job is one of the factors to improve emotional stability and present greater feasibility to change behavior due to a greater attachment to treatment and motivation intrinsic, which in turn creates a feeling of utility and value for themselves.
In the same way, it can be interpreted that the results obtained with them was due to the evolution and unique and individual characteristics, in particular ways that they had in order to identify their needs and importance in the labor and social areas while focusing on work in the other areas that were also part of the research Particularly in the family that was where everyone showed a change towards a higher level of satisfaction as well as being able to express and identify valuable reasons for which it was necessary to make changes in that area, allowing them a development of greater maturity and optimum for the development and evolution of multidisciplinary treatment. Meanwhile, the study also identified that the 43.48% who did not comply with the permanence factor in the rehabilitation, according to the criteria, show that there are factors such as the economic ones for the transfer to the CISAME and the labor instability, which affected the amount of assistance but not the quality of significance of the changes in behavior perceived as a result of the intervention in them. One of the areas where this change in behavior can be observed was mainly in the workplace, where it can be interpreted that the patients did not have a job at the beginning but, during the research process, they were able to obtain and maintain a job, as well as those patients who did meet all the criteria, to be able to create a greater balance and take advantage of the sessions in which they participated, offering them a feeling of usefulness, as well as the modification of his behavior and perception in other areas of his life such as sexual, where there was a better role of identification with his sexuality and the role he plays in his psychosocial and family development, where his behavior and level from maturity to interest and ease to get involved in family matters gave the patient a sense of belonging and importance to himself and others. Therefore, it was found that the patients, relatives and workers of the unit created and/or developed awareness of the needs that are required in people with a diagnosis of schizophrenia through interaction with the family, with the community and society counting on an ethical and professional support from the staff and, more importantly, creating a higher level of disease awareness, mainly in the patients and relatives, who prior to the investigation, believed they had no options, were subject to a pharmaceutical routine exclusively, were unaware of the development of the potential they had and, above all, the patient's prioritization to be able to create their own stability through their knowledge and physical and psychic perception, for the construction of a person of greater maturity and independence.
During the investigation, it was found that the interaction with the staff and the facilities and tools provided by them and the unit were also a determining factor in obtaining positive results for the patients. Emphasis should be placed on the fact that the relevance with which each subject can be involved in personal and group development, in all areas and levels, it is what will allow him to continue advancing as an individual beyond a previously granted psychiatric diagnosis without leaving aside the relevance of the multidisciplinary treatment with which he was working, this in order to reach a global understanding of what it is to remain being a person. The results of the study show that in future research it should be remembered that when working from a psychosocial perspective, it will be necessary to dedicate more time for each patient, space and availability of health specialists as well as patients and family members. To delimit and identify all those problems that may arise for future studies will be an indispensable factor for the development and evolution of the treatment of people with schizophrenia with a psychosocial rehabilitation model approach. Additionally, this research also confirms that the intervention helped to improve adherence to treatment, reducing negative symptoms (which are not usually treated by the medication). Therefore it can be inferred that the results obtained by a psychosocial rehabilitation program with a duration of 40 sessions in conjunction with elements of psychoeducation, cognitive behavioral therapy and multidisciplinary work of social work, nursing, psychiatry and pharmacology, compared to therapies that only apply the elements in isolation, will show optimal results for improving the expectation of quality in the patients’ life. Another of the conclusions that will be important to emphasize is the factor (as it is marked in the literature) of approaching the problem and evolution of the individual pathology of each patient because, mainly from the psychosocial model of speech of a constant process and without a deadline, as well as a psychotherapeutic treatment with a "normal" person, and should be considered for the interpretation and assessment of the data presented and future research.
Therefore, as regards the psychosocial areas where greater relevance has been presented to patients with the diagnosis of schizophrenia under the psychosocial rehabilitation treatment model, it will be understood that the results may be reflected depending on the main stage in which find the person, the level of evolution of pathology, the attachment and permanence to the treatment as well as the levels and areas with which the patient is working and focused mainly due to his own style and quality of life with which he has both individual way as cognitive, labor, social, economic, sexual, family and global. It can be taken as a final conclusion that, to date, psychosocial rehabilitation has begun to take an indispensable and valuable role in different areas of health21−24 where could find a promising field of future research as well as opportunities and interventions for the benefit of all patients diagnosed with schizophrenia (or in case of adaptability at work, in other serious mental disorders). That is why the reader should be reminded of the level of impact and importance that this field has in the work of the psychologist as well as all those health specialists who are involved with patients. The rehabilitation of people with a diagnosis of schizophrenia, or any serious mental disorder, should go beyond satisfying basic needs, so that the staff of every health specialist with these patients should also be involved in constant training activities and learning for the greatest possible optimal use in the treatment work with these patients.
None.
The authors declare that there is no conflict of interest.

©2018 Contreras, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.