Journal of
eISSN: 2379-6359


Case Report Volume 17 Issue 2
Correspondence: Nilofer Halim, Department of Oral Medicine and Radiology, Century International Institute of Dental Science and Research Centre, Kerala, India., Tel 8089794270
Received: April 26, 2025 | Published: May 22, 2025
Citation: Halim N. Unusual case of hemifacial microsomia with upper limb defects suggestive of Nager syndrome: clinical and radiological insights. J Otolaryngol ENT Res. 2025;17(2):52‒56 DOI: 10.15406/joentr.2025.17.00566
Craniofacial asymmetry presents significant diagnostic challenges, particularly when associated with syndromic conditions. This case report presents the clinical evaluation and diagnostic approach to craniofacial anomalies through a case study of a 44-year-old male presenting with features consistent with Nager syndrome—a rare acrofacial dysostosis characterized by craniofacial deformities and upper limb anomalies. Clinical and radiological examinations revealed distinct craniofacial abnormalities, including facial asymmetry, micrognathia, maxillary hypoplasia, cleft palate, and limb deformities such as elbow ankylosis and radial hypoplasia. Despite the presence of multiple craniofacial and skeletal anomalies, systemic health parameters were within normal limits, except for elevated random blood glucose levels. This case underscores the importance of a multidisciplinary approach in the diagnosis and management of craniofacial syndromes and highlights the role of dental professionals in identifying such rare conditions. Notably, the patient exhibited normal growth and cognitive development, minimal functional disabilities, and no significant medical dysfunction.
Keywords: nager syndrome, hemifacial macrosomia, craniofacial defects, upper limb deformity
Craniofacial asymmetry poses a significant challenge in clinical practice, particularly for dental professionals who are crucial in diagnosing and managing these complex cases. Facial asymmetry can be associated with various congenital, developmental, or acquired conditions, including craniofacial syndromes such as Nager syndrome, hemifacial microsomia (HFM), and Treacher Collins syndrome (TCS).1 Accurate diagnosis is often complicated by the overlapping clinical features of these syndromes, which may affect the skeletal, dental, and soft tissue structures of the face.2 Early recognition and differentiation of craniofacial anomalies are essential to guide treatment planning and to optimize both functional and aesthetic outcomes. However, the variability in phenotypic expression, the rarity of some syndromic conditions, and the potential for concurrent dental anomalies further contribute to diagnostic complexity.3
Nager syndrome was initially described by Nager and de Reynier in 19484 when they introduced the term acrofacial dysostosis to characterize the condition.4,5 This syndrome is an exceptionally uncommon genetic disorder, with only around 100 cases reported in medical literature. The majority of cases arise sporadically. Nager syndrome falls within a broader classification of conditions known as dysostoses, which primarily affect craniofacial development.6
The presence of affected siblings despite unaffected parents points to possible genetic variability and suggests that an autosomal recessive form may exist, although the precise inheritance pattern remains uncertain.4
Characteristic facial features include down-slanting palpebral fissures, underdeveloped cheekbones (malar hypoplasia), retrognathia and/or micrognathia, glossoptosis, cleft palate, low-set ears with abnormal structure (dysmorphic pinnae), microtia, and abnormalities in the external auditory canal and middle ear. Upper limb anomalies are also common, especially involving the radial side, and may include underdeveloped or absent thumbs, triphalangeal thumbs, radial aplasia or hypoplasia, and radioulnar synostosis.6-9
44-year-old patient reported to the Department of Oral Medicine and Radiology, Century International Institute of Dental Science and Research Centre, Kerala, India with the chief complaint of mobile lower front tooth for 1 year. The present patient was the eighth child of healthy non-consanguineous parents. He was born via vaginal delivery. The pregnancy of the mother was uncomplicated. The mother’s history regarding alcohol, smoking, and drug abuse was negative. There was no history of trauma to the head and neck region or maternal exposure to teratogenic agents were inconclusive. No signs of mental retardation or impairment of cognitive function were seen. Medical history and dental history were non-contributory. A family history of craniofacial disorder was not noted.
General Physical examination: the left upper limb was shorter than the right one, and the patient had a limitation of elbow extension. Lower limbs are normal in size however mild bowing of both legs was seen. Fingers are normal in size, shape, and numbers. No signs of clubbing and cyanosis were present (Figure 1).

Figure 1 Clinical photograph showing asymmetry of the upper limbs, with the left upper limb appearing shorter than the right and exhibiting limited elbow extension. The lower limbs are of normal size with mild bowing observed in both legs. Fingers appear normal in size, shape, and number, with no visible signs of clubbing or cyanosis.
Vital signs were within normal limits. Extra oral examination revealed facial asymmetry (deviation to the left side) with other associated craniofacial abnormalities including a small receding chin indicative of micrognathia, maxillary hypoplasia, depressed frontal bone with prominent eyebrows, exophthalmos, slanting palpebral fissure and a left malar hypoplasia (Figure 2). The mouth opening was normal with a deflection towards the left side. Intraoral examination revealed incomplete cleft palate, and generalized periodontitis with multiple teeth missing (Figure 3).

Figure 2 Facial asymmetry with leftward deviation, micrognathia, maxillary and left malar hypoplasia, prominent eyebrows, and slanting palpebral fissures.

Figure 3 Intraoral view showing incomplete cleft palate, generalized periodontitis, and multiple missing teeth.
On investigation, an orthopantomogram (OPG) was advised. The radiograph reveals significant asymmetry of the mandible, with notable hypoplasia of the left condyle and a marked reduction in the vertical height of the left ramus. The left antegoinial notch appears prominently accentuated, suggesting altered mandibular growth. Despite these morphological changes, the cortical bone appears well-defined, with normal bone density and an intact lower border of the mandible. The glenoid fossa on the left side maintains a normal appearance, without evidence of dysplasia or displacement. In contrast, the right side of the mandible appears structurally normal (Figure 4).

Figure 4 Orthopantomogram showing mandibular asymmetry with hypoplastic left condyle, reduced vertical height of the left ramus, and a prominent antegonial notch. Cortical bone and mandibular border are intact with normal bone density. The left glenoid fossa appears normal; the right mandible is structurally unremarkable.
Radiographic limbs show bony ankylosis of the elbow joint, with associated hypoplasia of the ulna and proximal radius, leading to elbow flexion deformity on the left side (Figure 5). Chest x-rays show no apparent abnormalities: normal lung fields, cardiac silhouette, and bony structures (Figure 6) PA skull view show hypoplastic maxilla, prominent antigoinial notch and deviation of mandible to left side (Figure 7 &Table 1).
|
A. Orbit |
|
O0 Normal |
|
O1 Small size |
|
O2 Poor position |
|
O3 Both small size and poor position |
|
B. Mandible (and TMJ) |
|
M0 Normal mandible-Type I |
|
M1 The mandible and glenoid fossa are small-Type IIA |
|
M2A Short ramus, glenoid fossa is in anatomically acceptable position-type IIA |
|
M2B Short ramus, TMJ is inferiorly, medially and anteriorly displaced with hypoplastic condyle-Type II B |
|
M3 Complete absence of ramus, glenoid fossa and TMJ-Type III |
|
C. Ear |
|
Ear anomaly can be classified into external, middle/atresia and presence of branchial arch remnants/sinus tracts. |
|
Max and Meurmen’s system is used in OMENS |
|
E0- normal ear |
|
E1- mild hypoplasia and cupping with all structures present |
|
E2- absence of external auditory meatus with variable hypoplasia of the concha |
|
E3-malposition lobule with absent auricle |
|
D. Facial nerve-seventh cranial nerve |
|
N0 No facial nerve involvement |
|
N1 Upper facial nerve involvement (temporal zygomatic) |
|
N2 Lower facial nerve involvement (buccal, mandibular, cervical) |
|
N3 All branches of facial nerve affected |
|
N.B Hypoglossal (N12) and trigeminal (N5) nerves can also be affected. |
|
E. Soft tissue deficiencies |
|
S0 normal-No obvious soft tissue or muscle deficiency |
|
S1 mild-Minimal subcutaneous/muscle deficiency |
|
S2 Moderate–between the two extremes S1 and S3 |
|
S3 Severe soft tissue deficiency due to subcutaneous and muscular hypoplasia |
Table 1 OMENS classification for HFM
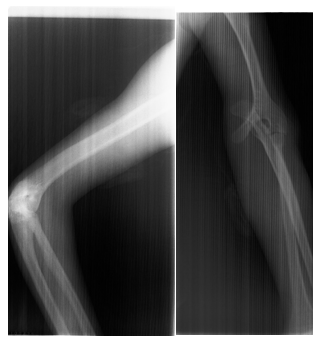
Figure 5 Radiograph of the left upper limb showing bony ankylosis of the elbow joint with hypoplasia of the ulna and proximal radius, resulting in an elbow flexion deformity.

Figure 6 Chest radiograph showing normal lung fields, cardiac silhouette, and bony structures with no apparent abnormalities.
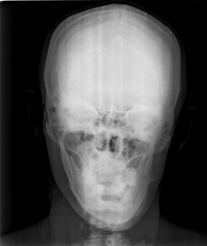
Figure 7 Posteroanterior skull view revealing hypoplastic maxilla, prominent antegonial notch, and mandibular deviation to the left side.
The patient's blood investigation results indicate a Random Blood Sugar (RBS) level of 191.8 mg/dL, which is elevated. However, Clotting Time (CT), Bleeding Time (BT), Platelet Count, Complete Blood Count (CBC), Total Count (TC), and Differential Count (DC) are all within normal limits.
Further investigations show that Rheumatoid Factor (RA factor) is negative, and Lipid Profile, Renal Function Tests (RFT), Liver Function Tests (LFT), and Thyroid Function Tests (TFT) are also within normal range. Additionally, cardiac assessments (ECG), reveal no abnormalities. Medical fitness obtained from the Physician, Dental extractions were done under local anesthesia and advised prosthetic rehabilitation.
This paper aims to highlight the evaluation of patients with craniofacial asymmetry, using a case of Nager syndrome- a rare acrofacial dysostosis characterized by craniofacial deformities and upper limb anomalies—as a model.
Nager syndrome is a congenital condition that presents with abnormalities affecting the craniofacial region and upper limbs, with the severity of these malformations varying from person to person. This case describes a 44-year-old male patient exhibiting distinct craniofacial deformities and limb abnormalities consistent with Nager syndrome, also referred to as Nager acrofacial dysostosis. The notable asymmetry of the mandible, micrognathia, maxillary underdevelopment, and upper limb deformities raise hemifacial microsomia (HFM) as a possible differential diagnosis due to the overlapping clinical features.8,9
Nager syndrome is classified within a group of rare genetic conditions known as Acrofacial Dysostoses (AFDs), which are characterized by skeletal malformations affecting the craniofacial structures and limbs.7,11 The condition arises from defective embryonic development involving the first and second branchial arches and limb buds. However, the underlying causes of these developmental abnormalities remain largely uncertain.4,9 Although most cases are sporadic, Nager syndrome can exhibit both autosomal dominant and autosomal recessive inheritance patterns, with reports of variable expressivity in affected families9,10,12
The primary clinical characteristics of Nager syndrome include.6,7,11-13 Craniofacial features like typical facial abnormalities include down-slanting palpebral fissures, underdeveloped cheekbones (malar hypoplasia), micrognathia, lower eyelid coloboma, ptosis, reduced eyelashes on the inner part of the lower eyelids, cleft or high-arched palate, and ear anomalies such as low-set, rotated, or dysplastic ears, preauricular tags, and atresia of the external auditory canal. It may be noted that the classic auricular and eyelid features were absent in our patient.6-7 Hearing loss- Conductive hearing loss is typical due to ear and auditory canal anomalies, though mixed hearing loss may also occur in some cases.11-12
Upper limb anomalies like common upper limb defects include hypoplasia or absence of the thumbs, triphalangeal thumbs, radial aplasia or hypoplasia, radioulnar synostosis, and shortened forearms. Phocomelia is rarely observed.6,11
Lower limb anomalies: These are usually mild or absent but may include conditions like metatarsus varus, shortened or missing toes, syndactyly, broad hallux, or clubfoot. Severe defects, such as fibular aplasia, are generally linked to lethal cases.11-13
Cardiac anomalies like congenital heart defects, though uncommon, may occur and include septal defects or tetralogy of Fallot.15
Intellectual function: Most individuals with Nager syndrome have normal cognitive development.3 In this patient, characteristic facial features- such as facial asymmetry, left-sided malar hypoplasia, micrognathia, and maxillary hypoplasia- are consistent with Nager syndrome.9 The incomplete cleft palate further supports this diagnosis, as cleft palate is frequently observed in affected individuals.16 Additionally, the absence of intellectual impairment aligns with typical presentations of Nager syndrome, where normal cognitive function is maintained.17
Facial dysostoses are classified into two main categories: mandibulofacial dysostoses and acrofacial dysostoses. Unlike acrofacial dysostoses, mandibulofacial dysostoses, including Treacher Collins syndrome, generally do not involve limb defects.6 Nager syndrome was first distinguished from Treacher Collins syndrome by Nager and de Reynier in 1948 and is thought to arise from developmental disturbances during early embryogenesis, between the third and fourth weeks.6,18-20
In this case, the patient’s upper limb deformities, including shortening of the left upper limb and limited elbow extension, reflect the preaxial limb defects that are characteristic of Nager syndrome.21 The slight bowing of the lower limbs, although not a common feature, may represent an additional skeletal anomaly.9 The normal configuration of the patient’s fingers, with no signs of syndactyly or polydactyly, helps distinguish this case from other acrofacial dysostoses, such as Miller syndrome, which tends to present with postaxial limb defects.22
Radiographic imaging further supports the diagnosis. The orthopantomogram (OPG) reveals mandibular asymmetry, left-sided condylar hypoplasia, and a reduction in vertical ramus height, all of which are indicative of the mandibular underdevelopment typical of Nager syndrome.10 The prominent antegonial notch also points to abnormal mandibular growth, a finding frequently reported in these patients.17 Despite these skeletal changes, the well-defined cortical bone suggests that severe osteodysplastic conditions are unlikely.
Additional systemic evaluations revealed elevated random blood sugar (RBS) levels, potentially indicative of an underlying metabolic disorder, such as diabetes mellitus, which is not commonly associated with Nager syndrome.24
Other laboratory tests, including lipid profile, renal and liver function, thyroid function, and rheumatoid factor, were within normal limits. Chest X-ray and ECG results were also unremarkable, helping rule out cardiac abnormalities, which are sometimes seen in craniofacial syndromes.16
The main differential diagnosis in this case is hemifacial microsomia (HFM), a condition marked by unilateral underdevelopment of facial structures, including the ear, mandible, and associated soft tissues.24 While HFM and Nager syndrome share some clinical similarities, the absence of ear anomalies and the presence of upper limb deformities make Nager syndrome the more likely diagnosis.21 HFM severity can be evaluated using the OMENS classification system, which assesses the involvement of the orbit, mandible, ear, nerve, and soft tissues.25,26 However, the patient’s bilateral limb abnormalities make Nager syndrome a more probable diagnosis in this case.
In conclusion, the clinical, radiological, and systemic findings strongly suggest Nager syndrome as the most likely diagnosis, with hemifacial microsomia as a differential consideration. Genetic testing, particularly for SF3B4 gene mutations, may confirm the diagnosis.27 Early intervention involving a multidisciplinary team- comprising maxillofacial surgeons, orthopedic specialists, and dental experts—is essential for optimizing the patient’s functional abilities and aesthetic outcomes.
None.
The author declares that there are no conflicts of interest.

©2025 Halim, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.