Journal of
eISSN: 2379-6359


Research Article Volume 11 Issue 1
1Head and Neck Division, Department of Otolaryngology, Italian Hospital Buenos Aires, Argentina
2Residents, Department of Otolaryngology, Italian Hospital Buenos Aires, Argentina
Correspondence: Carlos Santiago Ruggeri MD, Department of Otolaryngology, Italian Hospital Buenos Aires - Gascon 450, CP1181, CABA, Argentina
Received: June 11, 2018 | Published: February 6, 2019
Citation: Ruggeri CS, Lopez S, Molachino R, et al. Transoral treatment of stageg T3 laryngeal cancer. J Otolaryngol ENT Res. 2019;11(1):60-64. DOI: 10.15406/joentr.2019.11.00411
Objectives: To determine the local control rate and disease-specific survival rate in patients with staged T3 laryngeal cancer treated with electrocautery, radiofrequency or CO2 laser transoral microsurgery as well as the incidence of complications and tracheostomy, gastrostomy or enteral nutrition requirement in these patients.
Study design: Descriptive and prospective.
Methods: Twenty seven patients with T3 laryngeal cancer were treated with electrocautery, radiofrequency or CO2 laser microsurgery at the Italian Hospital of Buenos Aires between August 2009 and december 2016.
Patients with T3 tumors were classified according to the 2002 American Joint Committee on Cancer (AJCC) TNM staging system. These tumors caused vocal cord fixation, pre-epiglottic or paraglottic space involvement, focal infiltration of the thyroid cartilage or postcricoid invasion.
Results: The initial local control rate was 44.44% (12/27), local control with rescue treatment was 59.25% (16/27). The specific survival was 59.25% (16/27). The rate of preservation of the larynx was 44.44% (12/27). The average follow-up time was 5 years. Four patients had serious complications: esophageal, glottic and esophageal stenosis (postadjuvant treatment with (QT/RT) and two had postoperative bleeding.Two patients needed a postoperative tracheostomy (7.40%) and 25 were able to feed orally (92.59%). The mortality due to complications was 3.7% (1/27).
Conclusion: In patients treated by a transoral approach, for T3 staged laryngeal cancer, the initial local control rate was 44.44% (12/27), and local control with rescue treatment was 59.25% (16/27). The specific survival was 59.25% (16/27), and the rate of preservation of the larynx was 44.44% (12/27). Transoral sugery, in selected patients with T3 staging laryngeal cancer represents other therapeutic option to preserve the function of the larynx and has oncological results similar to other treatments. The use of radiofrequency or cautery to resect the tumor reduces the costs of treatment
Keywords: larynx cancer, T3, transoral surgery
Patients with staged T3 laryngeal cancer can be treated in different ways. Traditionally, tumors with dvanced T were treated by total laryngectomy. The morbidity of surgery, together with the impact on the quality of life caused by total laryngectomy they made other therapeutic strategies to emerge. In selected patients with T3, partial surgeries by external approach or the use of chemotherapy and concurrent radiotherapy (QT/RT) protocols can be oncologically valid options that can preserve the function of the larynx.From the results published by Steiner in 1993, transoral resection is a therapeutic alternative, to treat patients with staged T3 laryngeal cancer with similar rates of local disease control than other treatments and with a high rate of preservation of laryngeal function.
Objectives
Study design
Descriptive and prospective.
We included 27 patients with T3 staged laryngeal cancer who were treated by a transoral approach with microscope, assisted with radiofrequency, cautery, and CO2 laser with superpulse at the Italian Hospital of Buenos Aires, between August 2009 and December 2016.
We excluded patients with previously staged Tis, T1, T2 and T4 laryngeal cancer, those who were treated by external surgical approaches, or who had a postoperative follow-up of less than 1 year.
The collected data in the patients were: age and sex, TNM staging and histology of the lesions, type of surgical resection, need for tracheostomy, nasogastric tube feeding or gastrostomy, time of hospitalization, complications, local control rate and disease specific survival rate, associated treatments, and follow-up time. They were recorded in a Microsoft Office Excel 2010 Table. Squamous cell carcinomas were staged according to the TNM classification of the AJCC of 2002.
Were considered T3 when to be tumors caused vocal cord fixation, paraglottic or preepiglottic space invasion, erosion of the internal table of the thyroid cartilage, or postcricoid area invasion. Suspension laryngoscopes of different diameters and bivalve laryngoscope were used to resect supraglottic tumors and cancer with extension to the hypopharynx. We also use electrocautery or radiofrequency equipment in monopolar mode with 24 cm scalpel, or CO2 laser with superpulso, straight and angled forceps and micro-scissors, conventional dissectors for laryngeal microsurgery and microscope with 400 mm lens and magnifications of 6x, 10x, 16x, 25x.1–5
The patients were operated under general anesthesia with conventional endotracheal tubes for laryngeal microsurgery and protected tubes for use with CO2 laser.
The surgical technique consisted of resecting the tumor by sectors, until visualizing with the microscope that the margins were free of disease. In some patients the internal perichondrium of the thyroid cartilage was dissected to enlarge the deep margin.6,7
Intraoperative biopsies of the superficial and deep margins were performed to confirm that the exeresis was complete. Alll patients were admitted to the postoperative period in the intermediate or intensive therapy unit according to their comorbidities. Since the year 2014, a functional swallowing study (FEEST) was performed in the patient's room, 24 hours after surgery to evaluate the swallowing alteration that might have caused the surgery and the need or not for feeding through a nasogastric tube.
We treated 27 patients with staged T3 laryngeal cancer, 24 men and 3 women. The average age was 67.4 years. They were evaluated by laryngofibroscopy, computed tomography of the neck, thorax, abdomen and pelvis with contrast, and others patients with PET/CT. All patients underwent a biopsy under general anesthesia, prior to surgical treatment. The histology of all tumors was squamous cell carcinoma. Eighteen patients had tumors located in the glottis and 9 in supraglottis Figure 1.
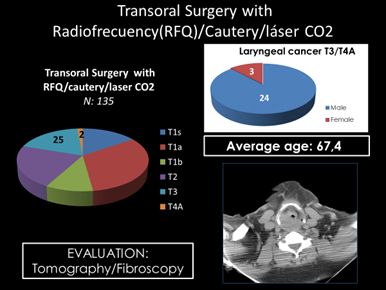
Figure 1 Twenty-six were N0M0 and 1 supraglottic cancer was N2b (staging by posoperative histopathology).
Eighteen were T3 staged because they had the fixed vocal cord and paraglottic space invasion, 5 by paraglottic space invasion,1 by preepiglottic space invasion, another by paraglottic and preepiglottic space compromise and 2 were staged T4a in the postoperative period by to find a extension to trachea and through the cricothyroid membrane.8
Two patients were previously treated with concurrent chemotherapy and radiotherapy, and another 2 with radiotherapy for laryngeal cancer.
In another patient a transoral resection for a T2 staged cancer had been performed, 5 years before. In 5 patients postoperative concurrent QT/RT was indicated In one because the deferred studies of the intraoperative biopsies of the margins that had been negative, were positive for cancer, in two others because T4a was staged in the postoperative (extension to trachea and through the cricothyroid membrane), in another patient who had a history of several negative biopsies performed at another center and it was decided to make a excisional biopsy but without margins control.9,10 He also had a history of kidney transplant and was immunosuppressed and preferred not to have surgery again to expand the margins of the previous resection. The fifth patient had nodal metastases in the neck (N2-b), diagnosed by the histopathological study of the surgical piece of the selective neck dissection Figure 2 & Figure 3.
One of the operated patients had a previous tracheostomy performed in another center and only in two patients of our series it was necessary to perform a postoperative tracheostomy for complications.
Twenty-five were able to feed orally. One of the patients who received posoperative QT/RT had a laryngeal and esophageal stenosis as a complication. A total laryngectomy was indicated, which he did not accept and lives without disease with a tracheostomy and gastrostomy.11,12
The longest feeding time for NTF/G occurred in patients with supraglottic tumors or in those who received before or after the surgery RT and/or QT. The average hospitalization time was 5.2 days. Two patients had minor complications: prelaryngeal cervical abscesses that produced at 12 days average of surgery and drained spontaneously, and 4 had serious complications: esophageal, glottic and esophageal stenosis (post-adjuvant treatment with QT/RT) and two had postoperative bleeding. A patient had a bleeding 10 hours after surgery, an emergency tracheostomy was performed and the laryngeal artery was ligated in the operating room, resolving the hemorrhage.13–18
The patient died 48 hours later due to cerebral anoxia due to the aspiration of blood. Another had a hemorrhage 7 days after the surgery, being externated. It was explored in the operating room and the bleeding site was not detected, so both superior laryngeal arteries were ligated. He returned to bleed the next morning, so it was decided to perform an angiography. It was detected the artery that caused the bleeding, which was a branch of the lower thyroid and was embolized. During the course of the study, while the patient was bleeding, had a cardiorespiratory arrest, he had a tracheotomy and was reanimated. He evolved satisfactorily and was discharged with the closed tracheostomy. The mortality due to complications was 3.7% (1/27) Figure 4.
Ten patients died (5 due to cancer of the larynx and 5 due to other causes), one was lost from follow-up and 16 live. Three of the 16 live with a total laryngectomy and one with a tracheostomy / gastrostomy (post adjuvant QT/RT). Initial local control was 44.44% (12/27), local control with rescue treatment was 59.25% (16/27). The specific survival was 59.25% (16/27). The rate of preservation of the larynx was 44.44% (12/27). The average follow-up time was 5 years (Figure 5).
The transoral surgical treatment assisted with CO2 laser of malignant laryngeal tumors is has become the treatment of choice in many centers around the world, especially in patients with early T (Tis, T1 and T2). In advanced tumors (T3) transoral resection is an effective treatment, but due to the multiple therapeutic options (concurrent chemotherapy and radiotherapy, partial laryngectomies, and total laryngectomy) there is no global consensus on its indication. Reference hospitals around the world use one or other of these options ith similar results of local control.
The studies published by Wolf in 1991 showed that the use of chemotherapy induction followed in the patients who responded (tumor size reduction of 50% or more) of radiotherapy, achieved local control rates similar to those obtained by laryngectomy total, but 61% of the patients in the group treated with chemotherapy and radiotherapy conserved the function of his larynx.19 The concept arose of healing with preservation of function and that treated patients had the best quality of life.
This concept came to the surgeons and led to the development of external surgical techniques such as supracricoid laryngectomies that in selected cases allow to avoid a total laryngectomy.9 These techniques represent an advance in the concept of healing with a better quality of life but they require a tracheostomy and nasogastric tube feeding or gastrostomy for a time that is sometimes lengthy. In the early 1990s, Steiner published the results of the CO2 laser-assisted transoral technique.16–18 The results obtained in terms of survival and local control were similar to those obtained with external surgeries.
For these studies and the technological advances produced, the transoral resection technique assisted with CO2 laser it spread, being at present in some centers the treatment of choice for patients with laryngeal cancer in early stages, and a alternative in advanced T staged. The advantages of surgery over radiotherapy are to avoid radiant treatment in tumors initials since 25% of patients with malignant laryngeal tumors can have a second primary tumor in the head and neck that could require radiotherapy, and also avoid irradiate the contralateral healthy vocal cord. The advantages of transoral resection compared to partial laryngectomies by an external approach are: avoid tracheostomies, reduce feeding time by nasogastric tube or by gastrostomy and decrease the hospitalization time (most frequent 24 hours in the common room vs 7 to 10 days in intermediate therapy for external techniques).
The possibility of performing assisted transoral resections with other equipment such as electrocautery or radiofrequency is mentioned in a few works.3–15 An experimental study shows that the damage produced in the tissues by the CO2 laser (2-3W, superpulse, spot of 0.5-0.8mm) and with electrosurgery with microelectrodes was the same in the cut mode, and the damage was greater in coagulation mode.2 Unlike the CO2 laser the radiofrequency or electrocautery scalpel allows to work with different angles and coagulate vessels larger than 0.5mm without changing instruments. It has the disadvantage that the surgeon must work with both hands through the laryngoscope.
Several studies describe the robotic surgical technique using the da Vinci system and report the use the monopolar scalpel connected to the cautery unit to perform transoral laryngectomies20–21 The therapeutic options for T3 staged tumors have similar results. Sessions obtains a total and specific 5-year survival of 54% and 67% respectively for T3 treated by total laryngectomy.14
In 2003, the preliminary results of a randomized study were published that compared the results of treatment of advanced laryngeal cancer with inductive chemotherapy followed of radiotherapy, chemotherapy and concurrent radiotherapy and radiotherapy only (RTOG91-11). Local control of 78% and laryngeal preservation of 88% in advanced tumors were reported, with 2 years of follow-up. In this study, tumors with advanced N and lower T were considered advanced.6 The treatment with concurrent QT/RT was superior to the other therapeutic modalities, and the authors concluded that this combination should be considered the best treatment option. At 5 years the same study showed no differences in survival between the different treatments that included chemo and/or radiotherapy; patients treated with concurrent QT/RT
they were dying from chronic toxicity.
The 5-year survival without total laryngectomy was 46.6%, the locoregional control 68.6%, the global survival 55%, and survival without disease: 39% .7 With transoral surgery assisted with CO2 laser Ambrosch reports a local control of 68% and a laryngeal preservation rate of 87% in 70 T3.1 In a multi-center study on CO2-laser assisted transoral treatment of carcinomas of the larynx T2-T4, stage III-IV report a local and locoregional control of 82% and 77% and a specific and total survival of 68% and 75% respectively at 2 years of follow-up. With 5 years of follow-up, local and locoregional control, specific and total survival were respectively: 74%, 68%, 58% and 55%.
45 Patients out of 117 received postoperative treatment with radiotherapy.8 Vilaseca reports that T3 cancer by fixation of the vocal cord or by tumor focal infiltration of the thyroid cartilage were independent factors of poor prognosis in the multivariate analysis.20–22 Treatment with concurrent QT/RT should be considered as an initial option in voice professionals since in general the preservation of the voice is better with this therapeutic than with the transoral resection.
In patients treated by a transoral approach, for T3 staged laryngeal cancer, the initial local control rate was 44.44% (12/27), and local control with rescue treatment was 59.25% (16/27). The specific survival was 59.25% (16/27), and the rate of preservation of the larynx was 44.44% (12/27). Two patients needed a postoperative tracheostomy (7.40%) and 25 were able to feed orally (92.59%). Transoral sugery, in selected patients with T3 staging laryngeal cancer represents other therapeutic option to preserve the function of the larynx and has oncological results similar to other treatments. The use of radiofrequency or cautery to resect the tumor reduces the costs of treatment.
The authors appreciate the assistance of all children who participated in this work.
Authors declare that there is no conflict of interest.

©2019 Ruggeri, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.