Journal of
eISSN: 2379-6359


Case Report Volume 10 Issue 1
University of Illinois Hospital and Health Science System, USA
Correspondence: Jamie A Spitz, Division of Plastic and Reconstructive Surgery, University of Illinois Hospital and Health Science System, Chicago
Received: April 24, 2017 | Published: February 19, 2018
Citation: Spitz JA, Bradford P, Hwang L, Ellis MF (2018) Surgical Management of Zygoma Fractures in Patients with Pre-injury Facial Asymmetry. J Otolaryngol ENT Res 10(1): 00312. DOI: 10.15406/joentr.2018.10.00312
Background: Deformational plagiocephaly (DP) is often treated with simple, conservative measures as an infant to correct calvarial deformities, however facial characteristics may persist into adulthood. We present a series of patients with pre–injury asymmetry and zygoma fractures that required alternative approaches to reduction and fixation due to their inherent calvarial deformities and/or facial scoliosis.
Methods: Four consecutive cases of zygoma fractures requiring alternative reconstructive techniques were reviewed. Each patient was counseled on their inherent asymmetry and offered creative solutions to minimize deformity. Operative interventions ranged from simple open reduction and internal fixation to implant based malar augmentation.
Results: Four patients with facial asymmetry underwent repair of traumatic zygoma fractures. Patient 1 had a remote history of DP with a cranial index 106%. Patients 2–4 did not have plagiocephaly but did display varying degrees of facial asymmetry. The timing of the first evaluation and surgery varied from 1 week to 10months. Patients 1 and 2 underwent camouflaging malar reconstruction using either autologous fat grafting or porous polyethylene implant placement. Patients 3 and 4 underwent traditional fixation with variable amounts of reduction. All patients achieved excellent facial symmetry or complete reduction of the ZMC congruent with their goals. There were no cases of postoperative complications related to lower lid position, nerve dysfunction, or infection.
Conclusion: When patients with facial asymmetry have traumatic injury of the ZMC standard options may require modification to meet patient goals. Careful consideration of pre–injury appearance, reconstruction requirements, and thoughtful surgical planning allow for successful outcomes.
The zygomaticomaxillary complex (ZMC) can account for up to 40% of midface fractures. They are the second most common facial fracture following nasal bone fractures.1 These fractures commonly stem from assault, motor vehicle accidents, and athletics.1–3 The ZMC is an important component of facial structure as it defines midface width and malar projection. The ZMC is often referred to as a tetrapod with the four legs representing facial buttresses. When these buttresses are fractured and unstable, the midface can take on a widened and flattened appearance altering facial aesthetics. Current surgical modalities to repair the fracture(s) and/or restore facial symmetry include reduction with or without internal fixation, or camouflaging procedures like fat grafting and implant placement.2–6 Most people have some degree of facial bony and soft tissue asymmetry.7,8 Skeletal asymmetries of less than 3% often go unrecognized due to overlying softtissue.9 To date, the literature surrounding the surgical management of adult patients treated for ZMC fractures with preinjury facial soft tissue and bony asymmetry remains scarce and illdefined. Etiologic factors contributing to preinjury facial asymmetry may include deformational plagiocephaly, congenital disorders, other acquired causes, or idiopathic processes.8,10 Often, trauma patients are not aware of their preinjury facial asymmetries until they critically examine themselves after the accident has occurred. Patients may desire to have their preinjury facial asymmetry addressed at the time of operative bony fixation of their ZMC fracture. We present a case of a patient with preinjury facial asymmetry that sustained a traumatic ZMC fracture to illustrate our management strategy for this unique patient population.
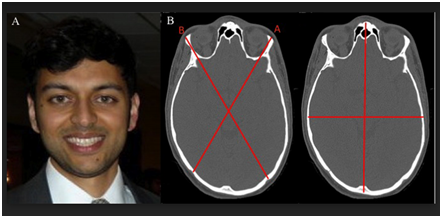
A 29year old male was involved in a motorcycle accident that resulted in a right orbital floor fracture, nasal bone fractures, and right zygomaticomaxillary buttress fracture. He was initially managed at an outside institution and had an attempt at right zygoma fixation and was referred to us for secondary reconstruction 4 months postoperatively. Upon presentation we identified multiple facial bony and soft tissue asymmetries, not all consistent with his fracture pattern. Therefore we had the patient provide a preinjury photograph, which was consistent with preinjury facial asymmetry (Figure 1A), and evaluated his oblique cranial length ratio (OCLR) and cranial vault asymmetry index (CVAI), which were both abnormal. His OCLR was 106% (normal<105%) and the CVAI was 6.1% (normal<3.5%) (Figure 1B). On exam he had right enopthalmos, palpable step off’s at the right orbital floor as well as nasal bones as a result of his injury (Figure 2A). His CT scan after the trauma was consistent with a right orbital floor fracture, nasal bone fractures, plated right zygomaticomaxillary buttress fracture, and malar asymmetry with the left side projecting more than the right (Figure 2B). However, on exam his right eyebrow was superior to the left, right ear lobule inferior to the left, left malar flattening, upper lip, lower lip, and chin deviation to the left. The latter was not consistent with his injury pattern, and likely a result of his remote history of DP. The patient was counseled on the facial aesthetic changes as a result of the trauma and his inherent facial characteristics. The patient desired improvement of his intrinsic malar symmetry in addition to open reduction internal fixation (ORIF) of his right orbit and nasal bones. His treatment consisted of orbital floor reconstruction with alloplastic mesh, nasal bone reduction, and contralateral malar implant placement. Intraoperative navigation facilitated planning and execution. In the postoperative period, the patient displayed clinical and radiographic improvement of his right orbit and nasal bones and improved malar symmetry (Figure 3A) (Figure 3B).
Facial asymmetry is common, and may be overlooked when treating traumatic ZMC fractures.9 After reviewing our operative experience of traumatic ZMC fractures over a 31month period, 4 out of 21 patients were found to display preinjury asymmetric facial bone structure. This is a 19% incidence of facial scoliosis in patients presenting for operative treatment of midface fractures. We found this incidence relatively high, and believe that it is due to the variety of etiologies responsible for the asymmetry. Deformational plagiocephaly, congenital disorders, acquired causes, or idiopathic processes can contribute to facial scoliosis. Deformational plagiocephaly is often treated with simple, conservative measures as an infant to correct calvarial deformities; however facial characteristics may persist into adulthood in 14% of patients.10 DP leads to a parallelogram shaped head, with anterior displacement of the ipsilateral forehead, cheek, and ear, sagittal displacement of the ipsilateral zygoma, and occasional facial asymmetries.11,12 This played a role in the case presented. Our patient was unaware of a prior diagnosis; however his facial appearance was not consistent with the fracture pattern on CT, which led us to evaluate him for DP that ultimately altered his operative plan in order to achieve his goals. The incidence of DP may be increasing due to the back to sleep campaign that began in 1994.13–15 These patients are now approaching their midtwenties which if the facial characteristics persist into adulthood, coincides with the age group most likely to be involved in trauma.16 It is incumbent upon maxillofacial surgeons to be aware of this special patient population and to counsel them in the perioperative period. Congenital disorders such as Hemifacial Microsomia, Goldenhar Syndrome, Parry Romberg Syndrome, Beckwith Wiedemann Syndrome, Neurofibromatosis, among others may have characteristic bony or soft tissue facial asymmetries that contribute to facial appearance in adulthood. Additional etiologies of facial asymmetry include acquired causes such as prior trauma, surgery, oncologic defects, radiation, and cosmetic.13
The most common cause of facial asymmetry is idiopathic and likely is due to gradual changes throughout craniofacial development.17 Facial asymmetry, ZMC fracture patterns, and patient preferences can present in a various combinations. Therefore we have developed an algorithm that addresses different surgical options for traumatic ZMC fractures in patients with preinjury facial asymmetry (Figure 4). The figure illustrates preinjury right malar prominence followed by a right ZMC fracture. The options postinjury include ORIF to return the patient to their preinjury state, open interal fixation without complete reduction (OIF) in order to improve the postoperative malar symmetry and set back the right ZMC, or contralateral malar contouring to match the prominence of the fractured, more pronounced right side. Additionally, if the fracture occurred on the less prominent side, ipsilateral contouring can be performed in addition to ORIF of the fracture if required for bony stability. We have used this algorithm in managing 3 other patients with preinjury facial asymmetry that presented after sustaining traumatic ZMC fractures. Each patient underwent an individual approach to surgically manage his preinjury facial scolios and new traumatic ZMC fracture. None of these patients were found to have DP, however they all displayed varying degrees of facial asymmetry. Patient 2 was a 19 yearold male referred to our service 2 months following a motor vehicle accident after his traumatic brain injury resolved. Upon review of his CT scan, he was noted to have a right orbital floor and medial wall fracture, right nondisplaced parasymphaseal mandibular fracture, non displaced right ZMC fracture, and a zygoma size discrepancy. He desired improvement of his malar symmetry in conjunction with repair of his facial fractures. Therefore, in addition to reconstruction of his right orbital floor and medial wall, structural autologous fat grafting was performed in a supraperiosteal plane to his right midface to enhance the malar projection.
Patient 3 was a 52year old male with preinjury facial asymmetry referred to us following a traumatic bicycle accident with a nondisplaced left zygomaticomaxillary buttress fracture and severely impacted and comminuted zygomatic arch fracture. On exam, in addition to a palpable left zygomatic arch step off deformity, he had asymmetric supraorbital rims with the left more superior than the right, left malar flattening, wide left midface width, and the left ear height was more superior to the right. The patient was counseled on his asymmetric facial bone structure, and he decided to have the zygomatic fracture repaired alone. Patient 4 was a 57 year old male with preinjury facial asymmetry that was intoxicated and fell down seventeen stairs resulting in a left ZMC fracture, loss of vision in his left eye, a C5 spinous process fracture, and subdural hematoma. He was referred to us 2 weeks after the injury following clearance from neurosurgery. At initial consultation, he had bilateral ecchymoses, conjunctival hematomas, prominent left malar projection compared to the right, and a tender left zygomaticomaxillary buttress and zygomatic arch to palpation with step off deformities. His fracture pattern involved his lateral and inferior orbital walls and rims, medial and lateral maxillary buttresses, and a comminuted zygomatic arch fracture.
Upon counseling this patient on his preinjury facial scoliosis preoperatively, he was unaware of any asymmetries and desired an improvement if possible without performing additional surgery. Therefore, this patient was managed with fixation alone of the left ZMC without formal, restorative reduction. Postoperatively, he had improved malar symmetry. All 4 of our patients with preinjury facial asymmetry that sustained traumatic ZMC fractures were managed in unique ways in order to fulfill their postoperative aesthetic goals in line with their individual fracture patterns. There were no complications postoperatively, and all patients were satisfied with their final outcome. We believe that our patients may have a higher level of postoperative satisfaction being educated and involved in the surgical decision making than if they were all treated with standard approaches to their fractures. Not all 4 patients were aware of their asymmetries prior to experiencing facial injury, nor did they all choose to address this surgically. However following traumatic facial fractures, people often critically examine themselves and may acutely recognize characteristics that have been present for years and are isolated from the traumatic fracture. Patients may need to be educated regarding the preexisting facial asymmetries that are not directly resulting from the facial trauma. We presented a variety of techniques to manage patients with preinjury facial asymmetry that are being evaluated for operative repair of zygoma fractures. Perioperative counseling is imperative in order to best serve this unique group of patients. Patient goals must be clarified and the risks and benefits of the various treatment options presented. Surgical treatment provides a unique opportunity to repair fractures and restore or correct facial asymmetry.
Traumatic ZMC fractures represent a large fraction of facial trauma, and significant facial asymmetry is common in the general population. We present an algorithm to approach patients with preinjury facial asymmetry that can be modified according to their unique fracture patterns and postoperative goals to achieve a successful outcome.
None.
Author declares that are no conflicts of interest.

©2018 Spitz, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.