Journal of
eISSN: 2379-6359


Case Report Volume 11 Issue 1
1Fellow in Head and Neck Surgical Oncology, Regional Cancer Centre, India
2Additional Professor, Dept of Head and Neck Surgical Oncology, India
Correspondence: Deepak Janardhan, Fellow in Head and Neck Surgical Oncology, Regional Cancer Centre, India, Tel 0-9961319859
Received: June 26, 2018 | Published: January 2, 2019
Citation: Janardhan D, Varghese BT, Kumar S. Salvage hemilaryngectomy for radio-recurrent laryngeal carcinoma in an elderly patient. J Otolaryngol ENT Res. 2019;11(1):1-3. DOI: 10.15406/joentr.2019.11.00398
Background: Recurrence after radiation therapy in early glottic cancers is around 5-35% and is usually within the first two years. Among these, one third is amenable to conservative laryngeal surgery which has shown a local control of 65-96% and a five year disease specific survival of 93%.
Case report: A 78 year old gentleman, a chronic smoker, who was diagnosed with T1aN0 carcinoma glottis, and had received radical radiotherapy; developed recurrence at the 10 month of followup.This was excised by Transoral laser Microsurgery. However after 1 year, it recurred again. A planned Open Partial Laryngectomy was carried out with achievement of adequate margins on final pathology report. He is disease free at 4th year of followup after the open partial laryngectomy.
Summary: Carefully selected patients with adequate lung function and no laryngoeophageal dysfunction can be considered for salvage conservation laryngeal surgery irrespective of their age, as locoregional control and Disease free Survival results are comparable with that of total laryngectomy, with superior functional outcome due to larynx preservation.
Keywords: radiorecurrence, partial laryngectomy, salvage surgery
Recurrences after Radical radiotherapy in early glottic cancers are around 5-35%1 and are usually in the first two years. Of these, one third are amenable to conservative laryngeal surgery which has shown local control of 65-96%2–4and five year disease specific survival of 93%,5,6 if carefully selected.But issues pertaining to decannulation and swallowing are unpredictable, leading to completion surgery in 2.5%.7,8 Moreover the overall complication rates and fistula formation after salvage conservative surgery is 8-20%.4–6 Decision on conservation in a salvage setting requires exact tumour mapping imageologically due to unpredicatable disease spread especially submucosally, multifocal, with superadded treatment sequelae like chondronecrosis and post radiation changes. Hence, once evaluated and found suitable, patients with adequate lung function and laryngoesophageal dysfunction free can be considered for salvage conservation laryngeal surgery based on the extent of the disease as in the case reported. Remarkable quality of life without the stigma of permanent stoma with comparable locoregional control and Disease free Survival provides an impetus for attempting conservation salvage laryngeal surgeries, instead of Total laryngectomy, as discussed in this case report.
78 year old male, a chronic smoker for more than 55yrs, diabetic for last 10 years and hypertensive for last 6 years was diagnosed to have carcinoma glottis T1a N0 M0, for which he was treated with radical radiotherapy using 5250cGy/ 15 Fr (hypofractionation protocol) in December, 2012 at our centre. He was under regular follow up once in 3 months. 10 months later, he presented with persistent hoarseness and irritant cough of 2 months duration in Jan 2014.
Nasopharyngolaryngoscopy (NPL) showed proliferative growth involving the anterior half of the left vocal cord for which a Transoral microlaryngeal CO2 LASER excision under frozen section control was done on 24/03/2014 with a presumptive diagnosis of post radiation therapy (RT) recurrence. The Histopathology report of the excised mass with adequate microscopic margin was that of moderately differentiated squamous cell carcinoma. During the subsequent follow up he again developed recurrence at the same site and the nasopharynglaryngoscopy (NPL) showed proliferative growth involving the entire left true cord with mobile vocal cords He was advised total laryngectomy and primary TEP as a salvage option in view of the history of failed conservation attempt and the old age.
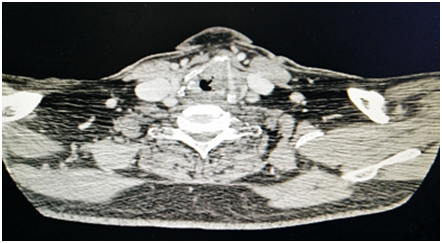
However he refused surgery and defaulted further follow up visits till the growth progressed further. Nasopharynglaryngoscopy (NPL) showed proliferative growth filling the anterior half of the left Vocal Cord reaching up to the anterior commissure (AC). A Computed Tomogram (CT) scan (Figure 1) showed Irregular thickening in left vocal cord involving anterior commissure and a paraglottic extension falling just short of the lamina of thyroid cartilage with 8 mms of subglottic extension. This time he reluctantly consented to undergo total laryngectomy and further expressed his strong desire to retain voice and consented for a voice preservation attempt during surgery.
With the unsolved dilemma of choosing between two difficult options of Total laryngectomy considering his age, second recurrence, anterior comissure (AC) involvement, subglottic extension, co-morbidities and possibility of recurrence with conservation attempt, a possible Conservative laryngeal surgery in view of mobility of vocal cords, relatively limited disease, good pulmonary reserve -with the keenness and motivation of the patient and his relatives, he was planned for vertical partial laryngectomy with consent for conversion to total laryngectomy if required.
Left extended vertical partial laryngectomy was done on February 2015 with frozen section control for margins. Intra operatively there was a proliferative growth involving left true cord and false cord. The AC was free and there was limited subglottic extension. With access to the tumour by a laryngo-fissure, the entire left true cord, false cord, ventricle, left and half of the lamina of thyroid cartilage was removed with preservation of the Left arytenoid cartilage and entire right hemilarynx. The resultant raw area was lined by the ipsilateral strap muscles and a planned protective tracheostomy was done.
Post operatively he had minimal aspiration for 1 week necessitating nasogastric feeding for 2 more weeks and oral feeding with semisolids was initiated after a period of 1 more week. Swallowing exercises were advised all throughout. Ryles Tube was removed on the 1st month. Tracheostomy decannulation could be done after 1 week postoperatively.
He was followed up every 2 week for first 2 months and then every month the latest being on 15/1/2016 with an intelligible voice, without any aspiration and a Mucosalised hemilarynx and adequate airway (Figure 2).
T1, T2 Carcinoma Larynx are treated with radiotherapy or endo-laryngeal laser excision / open partial resection. After treatment with radiotherapy, the rate of recurrence in patients with T1 tumors of the larynx range from 5% to 35%. Disease recurrence after primary nonsurgical therapy usually occurs within the first 24 months.10–13
Evaluation of the larynx after initial treatment remains challenging because of Post radiotherapy changes which include fibrosis, edema, and soft tissue and cartilage necrosis. The growth pattern of recurrent laryngeal carcinomas is different from that of primary carcinomas making per-operative tumour mapping difficult. Many recurrences present with multiple tumour foci, very often localized below an intact mucosa, and further they may be masked by the post-treatment edema and fibrosis.14,15
In cases of a proven recurrent tumor, the assessment of exact tumor extension may be extremely demanding, particularly in cases where voice-preservation salvage surgery is considered. The combination of endoscopy and baseline, post treatment and follow-up CT, MRI or by functional imaging with fluorodeoxy glucose–positron emission tomography (FDG-PET) can help improve early detection of recurrent laryngeal carcinoma.16
These patients can be stratified by stage at initial presentation or at the time of recurrence, and by the initial treatment used. For patients with initial tumors at its clinical stages I or II that have been treated by radiotherapy alone, endoscopic laser surgery, open partial laryngectomy, near total or total laryngectomy may be used, depending on the extent of the recurrent disease. Any stage beyond this precludes the 1st two options. In any case the recurrent tumour should be within its clinical stage 2.
Vertical Partial procedures are most often used for T1 tumors that involve the anterior commissure. Patients selected for conservation surgery of the larynx must have adequate lung function to cope with possible (micro) aspiration of food during the post-operative period.
Perioperative tracheostomy though used to be a norm, recent trend towards avoiding such procedures have been attempted17 with 100% LRC, 97% 5 year survival rates and 100% laryngeal preservation rates. Survival rates decline significantly in salvage scenarios.18
VPL, for T1 offers LRC of 89-100%. This drops to 75% when anterior commissure is involved8.Local recurrences further drops the 10 year survival rate from 63 to 31%.8 VPL for T2 Lesions offer 74-86% LRC, where subglottic or supraglottic extension and vocal fold mobility impairment were attributed for the grave outcome.19 Salvage VPL offers 55-100% LRC, with similar functional outcome as of primary cases.20–22 Decannulation and swallowing functions’ optimizing were found to be comparable in salvage and primary cases,21 even though literature reports conflicting results. The only parameter always adversely affecting the prognosis of laryngeal conservation procedures is involved resection margins during salvage surgery. Advanced age and associated comorbidities are clinical variables that often are contraindications for conservation procedures. For these patients, total laryngectomy is a safer alternative with less morbidity and mortality. This unique report is presented because, in-spite of his advanced age, in a tertiary care high volume setting, we are able to individualise the salvage decision to achieve a disease free period, till date, that is around 4years with a remarkable quality of life.
Routine partial laryngectomy procedures have dwindled in numbers in the recent past, due to the organ preservation strategies adopted. Conservation laryngeal surgeries still remain a valid option in carefully selected salvage setting patients, with adequate lung function with no laryngoeophageal dysfunction, irrespective of their age, as locoregional control and disease free survival results are comparable with that of total laryngectomy.
None.
The author declares there is no conflict of interest.
Involvement in the salvage surgical team.

©2019 Janardhan, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.