Journal of
eISSN: 2379-6359


Research Article Volume 14 Issue 2
Department of ENT Head and Neck Section, Italiano Hospital, Argentina.
Correspondence: Carlos Santiago Ruggeri, Department of ENT Head and Neck Section, Italiano Hospital, Argentina
Received: June 30, 2022 | Published: July 19, 2022
Citation: Ruggeri CS, Latourrette DC. Posterior cordotomy in bilateral vocal cord paralysis. J Otolaryngol ENT Res. 2022;14(2):39-42. DOI: 10.15406/joentr.2022.14.00503
Introduction: Bilateral vocal cords paralysis in adduction when it is irreversible requires treatment due to the inspiratory dyspnea that produces. Different surgical techniques can be used to increase the glottic space.
Posterior cordotomy with partial arytenoidectomy improves dyspnea and is one of the most used surgeries.
Objectives: To determine the resolution rate of inspiratory dyspnea or decannulation, in patients with bilateral vocal cord paralysis in adduction treated with posterior cordotomy and partial arytenoidectomy
Methods: A retrospective and descriptive study was carried out by analyzing the electronic medical records of all patients who had bilateral vocal cords paralysis in adduction and were treated with posterior cordotomy and partial arytenoidectomy between March 2004 and December 2018. The result of the posterior cordotomy with partial arytenoidectomy was determined according to the decannulation rate of the patients who had tracheostomy, according to dyspnea resolution after the cordotomy and by the increase of the postoperative glottic space evidenced by endoscopy.
Results: Nineteen patients were treated by bilateral vocal cord paralysis in adduction. The most frequent cause was a total thyroidectomy (9/19). Eight had a tracheostomy prior to posterior cordotomy. Seven of eight patients who had tracheostomy were able to decannulate, the rest had insufficient glottic space and did not return to control. All patients without tracheostomy (11/19) improved their inspiratory dyspnea and had no limitation for their daily life activities.
Conclusions: The resolution of inspiratory dyspnea in patients with bilateral vocal cords paralysis in adduction without tracheostomy, treated with posterior cordotomy and partial arytenoidectomy was 100% (11/11). In tracheotomized patients the decannulation rate was 87,50% (7/8).
Key words: bilateral paralysis, vocal cords, adduction, posterior cordotomy, partial aritenoidectomy
Bilateral vocal cord paralysis in adduction is rare. The most common etiology is surgical trauma, especially thyroid surgery. The inspiratory dyspnea that this produces, may require an emergency tracheostomy, although this intervention is not the first option or the ideal treatment. Different surgical techniques have been described to improve upper respiratory obstruction, prevailing for its effectiveness and lower morbidity those performed by transoral approach. Posterior cordotomy with or without partial resection of the arytenoid cartilage is the most used surgery to open the upper airway and improve dyspnea.
Drugs and reagents
To determine the rate of resolution of inspiratory dyspnea or decannulation in patients with bilateral cord paralysis in adduction, treated with posterior cordotomy and partial arytenoidectomy.
Descriptive and retrospective.
The electronic medical records of patients who consulted for inspiratory dyspnea or had a tracheostomy due to upper airway obstruction caused by bilateral cord paralysis in adduction between March 2004 and December 2018 were analyzed.
Patients who had bilateral immobility in adduction of the vocal cords caused by fixation of the cricoarytenoid joint or by infiltration by tumors were excluded. The data evaluated in the patients were: age and sex, etiology of bilateral chordal paralysis, presence of previous tracheostomy, type of surgery performed, complications, rate of decannulation and improvement of inspiratory dyspnea. They were recorded in a Microsoft Office Excel 2010 table. In all patients the evaluation of the function of the vocal cords was made by means of rhinofibrolaryngoscopy, and in some with videostroboscopy. Swallowing was evaluated 24 hours after surgery through a functional endoscopic swallowing study. Patients who had no history of previous surgical were studied with contrast-enhanced computed tomography and/or magnetic resonance imaging of the neck and chest. The patients were treated by transoral surgery under general anesthesia.
Suspension laryngoscopes of different diameters, a microscope with a 400 mm lens, with magnifications of 6x, 10x, 16x and 25x and conventional instruments for laryngeal microsurgery were used. The surgeries were performed with cautery (15 watts in cut and coagulation mode), uncontrolled radiofrequency, coblation or CO2 laser in continuous mode with superpulse (5-10 watts).
The surgical technique consisted in performing a posterior cordotomy (section of the vocal ligament and thyroarytenoid muscle in front of the vocal process), vaporization or cauterization of the posterior third of the vocal cord (triangular area between the vocal process, the internal perichondrium of the thyroid cartilage and the free edge of the vocal cords), resection of the middle and posterior third of the ventricular band and the vocal process of the arytenoid cartilage (Figure 1).
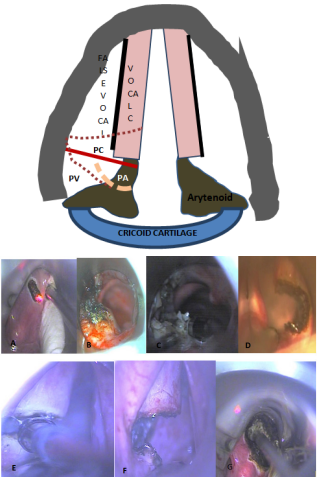
Figure 1 Posterior cordotomy with partial aritenoidectomy.
Posterior cordotomy with partial aritenoidectomy.
A, B, C, D: posterior cordotomy and arytenoids vocal process resection with CO2 laser.
E, F: posterior cordotomy and vocal process resection with coblation and cautery (G). Controls were performed by rhinofibrolaryngoscopy.
Patients were considered to have improved when they had no more dyspnea and they were able to perform activities of daily living without difficulty (absence of dyspnea when walking fastor when climbing stairs) or they were decannulated and the endoscopic control showed an increase in the glottic space.
Nineteen patients were treated for bilateral vocal cord paralysis in adduction. Nine were men and ten women, the youngest was 21 and the oldest 82 years old, the mean age was 61.88 years. The etiology of the paralysis was post-surgical in 13 and due to other diseases in 6 (cancer of the esophagus, lung cancer, giant esophageal diverticulum, bilateral vagal chemodectomy, Parkinson's disease, and post-treatment with chemo/radiotherapy for laryngeal cancer). The most frequent surgery that caused bilateral vocal cord paralysis was thyroidectomy (9/13), followed by cardiac surgery (2/13), and trachea (2/13) (Figure 2). The evaluation of the function of the vocal cords was performed in all patients by rhinofibrolaryngoscopy, in 11 a videostroboscopy and in another a larynx electromyography was also performed. Seven had a tracheostomy prior to posterior cordotomy (referred with tracheostomy performed in other hospitals) and in another it was performed at the same surgical time (history of cardiac surgery and high cardiological risk) (Figure 3).
One patient with a tracheostomy had a history of three previous cordotomies performed in other centers, which failed and could not be decannulated A posterior cordotomy and a bilateral partial arytenoidectomy was performed and after three months the tracheostoma was occluded. Revision surgery was indicated in 3 patients (15.78%) because the glottic space was insufficient to improve dyspnea after initial cordotomy and partial arytenoidectomy. In two a posterior cordotomy and resection of the vocal process of the contralateral arytenoids were performed. Three months were waited for the initial cordotomy to heal and determining the resulting glottic space. Both patients were able to decannulate. Another patient with a previous tracheostomy had insufficient glottic space after surgery and did not return to control.
In 4 patients at the end of the surgical procedure fibrin glue was placed in the cordotomy bed to reduce the formation of postoperative granulomas, and corticosteroids were injected in 8 to reduce the hypertrophic scarring and the consequent reduction of the glottic space. Seven of eight patients who had tracheostomy could be decannulated, the remaining had insufficient glottic space and did not return to control (Figure 4). All the patients without tracheostomy (11/19) improved their inspiratory dyspnea and had no limitation in activities of daily living. In the postoperative endoscopy, an increase in the glottic lumen was observed in all patients. Eight were evaluated 24 hours after surgery with a functional endoscopic swallowing study. Two patients had aspiration so they were fed through a nasogastric tube for an average of 35 days.
The goal of treating bilateral vocal cord paralysis in adduction is to restore airway patency, preserving voice quality as much as possible, and achieve decannulation in patients with tracheostomy. Tracheostomy improves the dyspnea but due to its morbidity it is not the appropriate treatment, should be considered a temporary intervention to solve an emergency. Bilateral vocal cords paralysis in adduction generates a severe deterioration in the quality of life, due to the dyspnea that this produces, and can be life-threatening due to the risk of complete obstruction of the airway. Between 26 and 70% is caused by surgical trauma (thyroidectomy most frequently), followed by prolonged intubation (direct pressure on the nerves due to the high position of the endotracheal tube cuff), malignant tumors of the thyroid, esophagus, trachea, and diseases neurological.1,2
In our study, the most frequent cause was also thyroid surgery. Other causes of bilateral chordal immobility are ankylosis of the cricoarytenoid joint due to trauma or rheumatic diseases, infiltration of the vocal cords due to cancer, sarcoidosis, amyloidosis and fixation by scar tissue (post-surgical, prolonged intubation, gastroesophageal reflux, post radiotherapy). Tracheostomy may be the best option in cases of dyspnea due to bilateral chordal paralysis of recent onset, and with possibilities of recovery, before indicating an irreversible surgical procedure. Dennis and Kashima in 1989 reported that posterior cordotomy with CO2 laser could be performed without prophylactic tracheostomy.3
We agree with the previous author since most of our patients (11/19: 57.89%) were treated without the need to perform a tracheostomy. In our study, only one tracheostomy was performed in the same surgical time as the cordotomy at the beginning of the series, because the patient had a high cardiological risk and we believe that not having a secure airway in the postoperative period would have been risky. The rest of the patients were tracheostomized in other hospitals prior to cordotomy. Different surgeries have been proposed to treat bilateral vocal cord paralysis. Surgeries may attempt to lateralize a vocal cord or section and/or resect tissue from one or both vocal cords. It is important to preserve the anterior and middle third of the vocal cords to reduce the deterioration of voice quality. In our study we did not perform an objective evaluation of the voice before and after cordotomy to quantify vocal quality, but none of the treated patients reported an alteration in their quality of life due to their vocal deterioration.
Laccourreye treated 25 patients with bilateral vocal paralysis in adduction with CO2 laser, 15 were unilateral and 10 bilateral posterior cordotomies. Sixty eight percent (17/25) of the patients Improved with a single surgical time, six patients had revision surgery due to insufficient glottic space and formation of granulomas. The airway was restored in 92% of patients The tracheostomy rate was 8% (2/25).4 Other authors obtained similar results with posterior cordotomy or with unilateral arytenoidectomy to increase the glottic space and to decannulate patients.5 In a multicenter study, they compared various transoral techniques to treat airway obstruction due to bilateral vocal cord paralysis Thirty six patients were treated, 64% with posterior cordotomy and medial arytenoidectomy, 11% with lateral fixation, and 8% with posterior cordotomy only.
Twenty five percent had episodes of dyspnea in the postoperative period and in 9 they performed revision surgeries. Seventy-five percent of the patients improved.6 In our study the failure of the initial cordotomy was 15.78% (3/19) and in two it was posible improve dyspnea with revision surgery. A prospective and randomized study compares patients with bilateral adduction vocal cord paralysis treated by posterior cordotomy with another group treated with a combination of posterior cordotomy and suture lateralization. There was no significant difference between both surgeries regarding respiratory efficiency, voice handicap index scores, and presence of postoperative aspiration.7
One study compared superpulse CO2 laser posterior cordotomy in continuous mode (1-10 watts) with patients in whom the same technique was performed but with cautery (cutting mode, at 20watts). Their conclusions were that the surgeries performed with laser or cautery had the same effectiveness (20% revision surgery for granulomas) and were minimally invasive. There were no statistically significant differences in the objective voice test between both groups.8 In another study they used radiofrequency in cut mode (15-25watt) in 11 patients to perform posterior cordotomy and reported in all an improvement in dyspnea and in exercise tolerance. Two required revision surgery for granulomas and crusting.9 When the vocal cord tissue is resected, it is essential to use equipment and instruments that allow adequate coagulation. Although we did not carry out a comparative study between the various methods to perform tissue resection and coagulation, the use of cautery, uncontrolled radiofrequency, coblation and CO2 laser for us it was similar. Adjuvant measures to surgery can be used, such as the application of topical mitomycin to reduce the proliferation of fibroblasts, corticosteroid infiltration to reduce fibrosis, or the placement of fibrin glue to reduce the granulation tissue.10 Some studies have reported the usefulness of dissecting a mucosal flap before performing the posterior cordotomy and/or arytenoidectomy to cover the surgical defect and decrease the production of granulomas and reduce scarring and consequent reduction of the glottic lumen.11 We had no evidence that fibrin glue placement or corticosteroid injection at the cordotomy site decreased the surgical revision rate.
The inspiratory dyspnea resolution in patients with bilateral vocal cords paralysis in adduction without tracheostomy, treated by posterior cordotomy was 100% (11/11). The decannulation in tracheostomized patients was 87.50% (7/8). Posterior cordotomy and partial arytenoidectomy (vocal process resection) performed by transoral approach with equipment that allows obtaining adequate hemostasis, it is a minimally invasive surgical technique that has excellent results to improve inspiratory dyspnea and the decannulation rate in tracheostomized patients.
The authors received no financial support for the research, authorship and publication of this article.
The authors declared no potential conflict of interest.
None.

©2022 Ruggeri, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.