Journal of
eISSN: 2379-6359


Case Report Volume 16 Issue 3
Department of ENT and Head-Neck Surgery, Sri Guru Ram Rai University, India
Correspondence: Apoorva Kumar Pandey, Professor Department of ENT and Head-Neck Surgery Sri Guru Ram Rai Institute of Medical and Health Sciences, India
Received: August 02, 2024 | Published: September 6, 2024
Citation: Pandey AK, Anjum F, Ahmed S, et al. Peri-apical granuloma presenting as a chronic cystic swelling in the hard palate: a case report. J Otolaryngol ENT Res. 2024;16(3):58‒60. DOI: 10.15406/joentr.2024.16.00551
A periapical granuloma, also known as a radicular or apical granuloma, is an inflammatory condition at the tip of a nonvital (dead) tooth. This lesion, which often begins as an epithelial-lined cyst, develops into granulation tissue inflammation at the root apex of the affected tooth, usually caused by dental decay or a bacterial infection of the tooth's pulp. While it is a relatively uncommon condition with a wide range of prevalence, the term "periapical granuloma" is used even though it does not contain granulomatous inflammation. This being a rare occurrence in usual clinical otolaryngologic practice, here we present a case report of a 55-year-old female with a lesion over her hard palate for two months.
Keywords: hard palate, cystic swelling, periapical granuloma
The most prevalent periapical lesions include periapical granuloma, periapical cyst, and periapical abscess.1,2 A periapical granuloma is a chronic inflammatory lesion located at the apex of a non-vital tooth. It is characterized by granulation tissue and scar formation, with varying numbers of chronic inflammatory cells such as lymphocytes, plasma cells, mast cells, and macrophages. Unlike granulomatous inflammation, which features a high presence of macrophages (histiocytes) and multinucleated giant cells, a periapical granuloma during an acute flare-up shows significant neutrophilic infiltration alongside the granulation tissue and chronic inflammatory cells.3–6
Clinically diagnosed acute apical periodontitis can sometimes be identified histologically as an acutely exacerbated periapical granuloma. Conversely, a periapical abscess in its quiescent stage may evolve into a periapical granuloma. Therefore, further research connecting the histological types of periapical granuloma with clinical diagnoses could be valuable for dental professionals. Such studies may help predict whether a clinically identified periapical lesion is a periapical granuloma, which is a common consequence of pulpal necrosis. Additionally, examining the histopathological types of periapical granuloma may assist in refining the existing classification of the lesion.
A 55-year-old female presented with a swelling over the hard palate for the last 2 months. It was not associated with pain or difficulty in chewing. On examination, there was swelling over the hard palate around 2X2 cm in dimension, tender to touch on deep palpation, soft, cystic, and compressible. There was no discharge on palpation from the swelling. Dental hygiene was poor and carious teeth were also there. She had a history of coronary angioplasty a few years back and she was on regular follow-up there. CECT neck was suggestive of infective? periapical cyst/ abscess formation along the hard palate in the midline extending into the right superior alveolar process at the roof of the right lateral incisor (Figure 1).
CECT PNS (neck also) revealed a well-defined mild peripherally enhancing hypodense area along the hard palate in the midline extending into the right superior alveolar process at the roof of the right lateral incisor with adjacent cortical irregularity and erosion possibly infective etiology?/periapical cyst/abscess formation. The patient was planned for Incision and drainage (curettage, if needed) under general anesthesia. A ‘U’ shaped incision (Figure 2) was given over the swelling and the irregular mass so found was removed and sent for HPE. Surrounding unhealthy tissue was curetted and suturing was done. The postoperative period was uneventful. Histopathological examination was suggestive of periapical granuloma (Figure 3a, 3b, 3c).
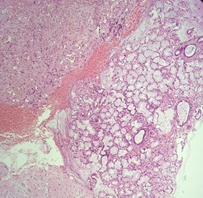
Figure 3a Sections show tissue exhibiting periapical granuloma with adjacent normal salivary gland tissue (H and E, X10).
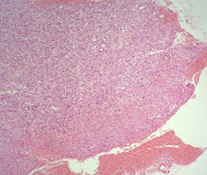
Figure 3b Sections show the proliferation of capillaries admixed with fibroblasts and lympho mononuclear infiltrates (H and E, X10).
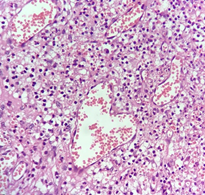
Figure 3c Sections show dilated and congested capillaries admixed with dense mixed inflammatory infiltrates, fibrosis, and foamy histiocytes (H and E, X40).
The patient is being followed up regularly for any complications.
Midline palatal swellings remain very uncommon. In our case report, the patient came to us with a complaint of palatal swelling for the last two months which was majorly asymptomatic. Differential diagnosis included a palatal abscess but the patient had no complaint of pain or fever. A dentigerous cyst was ruled out as a diagnosis based on the location of the swelling and on radiological investigations. Median anterior maxillary cyst remains another differential diagnosis but it has a more male preponderance and is often associated with burning sensation and numbness due to involvement of the nasopalatine nerve. The median palatal cyst was only ruled out based on histopathological examination as it also presents with similar complaints as perialveolar granuloma.
Inflammatory papillary hyperplasia generally presents with poor orodental hygiene and mostly in patients with artificial dentures which was not present in our case. An incisive canal cyst was ruled out on the basis of radiological investigation. Odontogenic keratocyst, a cyst derived from the remnants of the dental lamina with a biologic behavior similar to a benign neoplasm, was also ruled out due to the clinical presentation and the site involved. Moreover, it is commonly found in the male population. As in our case report, most periapical granulomas remain asymptomatic and can be diagnosed by X-ray or CT scan. Surgical removal remains the treatment of choice as was done in our case.
The case report so presented remains of particular interest as periapical granuloma in most cases may remain undiagnosed. As the most cases are asymptomatic and are only found during clinical examination or in severe cases when the patient experiences mild pain while chewing or discharge from the swelling. Surgical excision remains the treatment of choice with follow-up being of utmost importance to prevent recurrence of disease.
None.
The authors declare that there is no conflict of interest to disclose.

©2024 Pandey, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.