Journal of
eISSN: 2379-6359


Clinical Paper Volume 13 Issue 2
1St. Paul’s Hospital Melleniun Medical College, Etiopía
2General Teaching Hospital, Orlando Pantoja Tamayo, Cuba
Correspondence: Carlos Juan Puig González, St. Pablus Medical Melleniun Colloge, Addis Abeba, Etiopía, Tel +251961032042
Received: March 09, 2021 | Published: March 25, 2021
Citation: González CJP, Chong JCP, Bolano LC. Low grade mixofibrosarcoma in the mandible: A case report. J Otolaryngol ENT Res. 2021;13(2):18-20. DOI: 10.15406/joentr.2021.13.00484
Introduction: The term myxofibrosarcoma (MFS) and myxosarcoma refers to a neoplasm of connective tissue of fibroblastic origin, formerly called malignant fibrous histiocytoma.
Objective: To describe the clinical characteristics and the surgical medical procedure carried out.
Clinical case: 61-year-old male patient, with a history of relative previous health and a 2-year history with a lesion in the marginal gingiva. Bulging of both cortices and with an extension of the lower right to the left first premolar. Therefore, they are admitted for a better study and treatment.
Conclusions: It is a relatively rare tumor, of large size and wide dissemination at the lymph node levels of both the right and left hemi necks, drawing attention to its anterior location, the dissemination to levels IV and V of both necks, making it necessary to modify the management of the neck in our patient.
Keywords: myxofibrosarcoma, myxosarcoma, malignant fibrous histiocytoma
Malignant fibrous histiocytoma, named for O'Brien and Stout in 1964 and known today as myxofibrosarcoma (MFS) or myxosarcoma, is a connective tissue neoplasm of fibroblastic origin.1 This neoplasm was classified by Weiss as a low-grade tumor if it had a myxoid origin; intermediate grade, to that of mixed origin (myxoid and cellular) and of high grade to the tumor of cellular origin.2 Angervall redefined these terms, excluding from this classification myxoid lesions with lipoblastic, myoblastic or chondroblastic differentiation.1,2 MFS is an extremely rare histological subtype of soft tissue sarcomas of the head and neck. It is estimated that it appears in this region in less than 1% of the cases.3 Zhenjiang et al.4 report only 20 cases from 1975 to 2014, with a lower incidence those located in the mandible.4 Other authors include these tumors in the thyroid gland, paranasal sinuses, maxilla, nasal cavity, pyriform sinuses, and larynx.1–4 This tumor is considered one of the most aggressive and usually appears between the 5th and 7th decade of life. Some authors observe it more frequently in males and others do not find differences regarding sex.5 The location that occurs with the highest incidence is the upper extremities, trunk, retroperitoneum and mediastinum and with less frequency they are reported in the skin, heart and abdominal wall. Taking into account the infrequency of the presentation of this type of tumor with few reports in the specialized literature, the following work is presented with the aim of describing the medical and surgical procedure performed in a patient with myxofibrosarcoma in the mandibular region.
Clinical case
A 61-year-old male patient with a previous history of good health that began with a nodular lesion on the marginal gingiva, asymptomatic and slow but continuous, more than two years ago. In the last six months, this mass in the anterior region of the mandible continued to grow rapidly, with bulging of both cortices and infiltrating it from the first lower right premolar to the left. The mass rested on the lower lip without infiltrating it, with an exophysical pattern that made it relevant outside the oral cavity, for which the Maxillofacial Surgery service of St. Paul's Hospital Milennium Medical collage, in Addis ababa, Ethiopia was admitted. in 2021 for better study and treatment.
Physical exam
Personal and family pathological history: Anamnesis was performed in search of association with genetic alterations or syndromes implicated in the nature of these soft tissue tumors, such as: Li-Fraumeni syndrome, type 1 neurofibromatosis, Familial Adenomatous Polyposis, Gardner syndrome and others that are considered high risk. Intraoral examination: exophysical lesion, located in the anterior region of the mandible, of approximately 10 cm, which extended from the left first premolar (34) to the right first premolar (44), with a time of 18 months of evolution, of friable, bulging and grasping of the alveolar and mandibular bone, with mobility of the dental structures, central and lateral incisors in the bucco-lingual and mesio-distal direction (Class III According to Miller).6
Extraoral physical examination
Lymphonudules palpable bilaterally, in levels I, II, III, IV and V, which was visible in level I. They were rounded, approximately three cm in diameter, with a hard stone consistency and a tendency to fixation (Figure 1). After obtaining the confirmatory biopsy result (Number SP20-3561), such as low-grade myxofibrosarcoma, the surgical procedure was performed, which progressed well in the immediate postoperative period. After seven days, he was discharged and continued the follow-up by outpatient consultation until completing eight months after the surgery. At this time he continues treatment with radiotherapy.
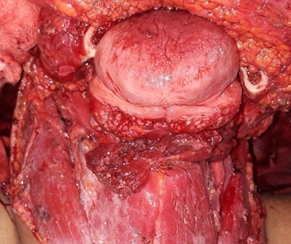
Figure 1 Surgical exeresis of the tumor and bilateral neck dissection with levels I-IV.
After obtaining the confirmatory biopsy result (Number SP20-3561), such as low-grade myxofibrosarcoma, the surgical procedure was performed, which progressed well in the immediate postoperative period. After seven days, he was discharged and continued the follow-up by outpatient consultation until completing eight months after the surgery. At this time he continues treatment with radiotherapy.
Diagnostic studies performed
Hemoglobin: 10 g / L
Coagulogram: normal
Serology: negative
HIV: Negative
Negative COVID test
Renal profile: creatinine: 87 mmol / L
Glomerular filtration: 110ml / min
Liver profile: normal (Figure 2)
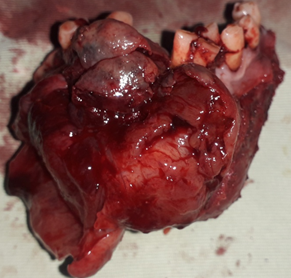
Figure 2 Segmental mandibulectomy: where we observe the size, shape and adherence and infiltration of this region in the bucco-lingual direction by the tumor.
Surgical procedure
Taking into account that it is a locally disseminated disease without lung involvement with the possibility of local treatment, classified as a T4a N1 M0 Stage IV, surgery was planned as the main form of treatment due to the impossibility on the part of the institution and other centers of the country to offer preoperative radiation therapy. A U-shaped or apron incision was made for the approach to the neck, with dissection of the superficial fascia, identification of nerve and vascular structures and emptying at different levels I-V bilaterally. For the mandibular region, we use an apron, bevel or pull thought flap as a way to remove the tumor, giving it a correct surgical margin (2.5 cm) and placement of the reconstruction plate, so that once the surgical treatment is finished, indicate chemotherapy adjuvant.
Myxofibrosarcoma is one of the most aggressive soft tissue neoplasms, it was reported in the literature for the first time in 19511. It usually appears in advanced ages, between the 5th to 7th decade of life, with preferences for the upper extremities, trunk and retroperitoneum and mediastinum,2,4,5 although localized in the skin, heart, and abdominal wall are also reported.5, 7 In the head and neck it is extremely rare, it appears in other anatomical locations such as: thyroid, parotid glands, paranasal sinuses, maxilla, nasal cavity, piriform sinuses, temporal fossa and larynx, among others.1,3–5 According to the classification of the soft tissue sarcomas of the World Health Organization in 2013, MFS belongs to tumors of fibroblastic and myofibroblastic origin.2 Regarding the diagnosis, it is necessary to clarify that we only obtained it through imaging techniques (conventional x-rays of the oblique lateral and anteroposterior jaw type) and the biopsy report of the Department of Pathological Anatomy of the Hospital without the possibility of performing other diagnostic techniques such as immunohistochemistry and in situ hybridization techniques. Important to evaluate the marking and identification of the same by the presence of the MET gene and the polysomy of chromosome 7, factors that are related to tumor progression, possible local recurrence and metastasis, depth, association with the epithelial variant and the histological grade among other elements necessary to define behavior and treatment.
Diagnostic differentiation is necessary with low-grade fibromyxoid sarcoma, myxoid liposarcoma, myxoma, nodular fasciitis, spindle cell lipoma as well as peripheral nerve sheath myxoma, which are tumors with histological similarities to MFS and with the need for immunohistochemical analysis for correct diagnosis.8 Low-grade MFS has a lower malignant potential, with a better prognosis, so metastases are rare, compared to high-grade. An overall survival range of 52% to 65% is reported at 5 years. 6 Recurrence of these low-grade tumors increases metastatic potential and presents as a high-grade tumor. Different studies report that there is a relationship between positive margins and local recurrence.7, 8 The experts of the European Society of Medical Oncology (ESMO) and those of the Global Cancer Systems (NCCN) of the United States of North America, present surgery as the first line of treatment in localized adult sarcomas and mention monoblock recession with negative surgical margins as standard for treatment.9
There are controversies in the treatment of neck dissections. But the truth is that the presence of metastatic lymphadenopathy to the neck is related to a high rate of relapse in metastatic sites, indicative of greater biological aggressiveness and poor prognosis in the overall survival of the disease. Recently 3 studies show the benefit and the long survival period after this treatment. One of the aforementioned studies was carried out with 2,127 patients, of which 75% had palpable lymph nodes at the time of diagnosis and a period of evolution greater than 3 years after the neck dissection was performed.9–11
There was a tumor of low frequency, of great size and wide dissemination at the lymph node level, both of the right and left hemicnecks, which draws attention to its anterior location and the spread to levels IV and V of both necks, for which it was necessary modify the treatment. Performing an exhaustive neck hollow.
None.
None.
The Authors do not refer to Conflict of interest.

©2021 González, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.