Journal of
eISSN: 2379-6359


Case Report Volume 15 Issue 3
1Apollo ENT Hospital, India
2Sterling Accuris Diagnostics, India
Correspondence: Pankaj Goyal, Apollo ENT Hospital, Pal road, Jodhpur, Rajasthan, India, Tel 9969393528
Received: July 17, 2023 | Published: September 6, 2023
Citation: Goyal P, Kumawat K, Kothari N. Laryngeal papillomatosis in an adult patient: managed with micolaryngeal surgery and CO2 laser. J Otolaryngol ENT Res. 2023;15(2):87-91. DOI: 10.15406/joentr.2023.15.00534
The most prevalent benign laryngeal tumour, squamous papilloma, typically affects the vocal folds and/or epiglottis. It is often associated with human papillomavirus (HPV) infection and can present as a single or multiple lesions. We describe a case of a 24-year-old male who presented with hoarseness and dysphonia for six to eight months. Laryngoscopy revealed exophytic, papillary lesion on the right true vocal fold with creating contact lesion on opposite side. The lesion was excised using carbon dioxide (CO2) laser and histopathology confirmed the diagnosis of squamous papilloma. The patient had no recurrence or complications at six months follow-up. This case illustrates the clinical features, diagnosis, and management of squamous papilloma of the true vocal fold in an adult patient.
Keywords: squamous papilloma; vocal folds; larynx; HPV; dysphonia; CO2 laser
HPV, human papillomavirus; RRP, recurrent respiratory papillomatosis; SML, suspension micro laryngoscopy; KTP, potassium titanyl phosphate
The term "warts in the throat" was first used by Marcellus Donnalus in the 17th century, but it wasn't until Sir Morell Mackenzie developed the term "papillomatosis" for these lesions in 1871 that it gained widespread use.
The growth of benign squamous papilloma at the laryngeal mucosa is called laryngeal papillomatosis. It has a papillary, exophytic growth with a fibrovascular core covered in multilayered squamous epithelium as its defining feature.
Although it can affect any area of the larynx, squamous papilloma commonly develops along the true and false vocal folds. It may appear as a single lesion or multiple lesions, with the latter being more prevalent in children and linked to recurrent respiratory papillomatosis (RRP).3 This illness is frequently connected with human papillomavirus (HPV) infection, particularly HPV types 6 and 11, which can affect the upper digestive tract as well as the entire respiratory tract.1–3 Hoarseness, dysphonia, stridor, dyspnoea, and cough are the most common clinical symptoms of squamous papilloma. Laryngoscopy and histology are used to make the diagnosis. There are various treatment options available, including as, laser surgery, surgical excision, antiviral therapy, electrocautery and cryosurgery.2–4 particularly in cases with multiple lesions and in children, the recurrence incidence is significant. Additionally, in roughly 20% of adult cases, malignant transition to squamous cell carcinoma has been documented.4 Recidivism, on the other hand, has been the most prominent event in its evolution. Additionally, obstructive laryngeal papillomatosis poses a life-threatening risk, making a rescue tracheostomy necessary.5
Therefore, long-term follow-up is recommended for patients with squamous papilloma. Here, we report a case of a 24-year-old male who presented with hoarseness and dysphonia for six to eight months and was diagnosed with squamous papilloma of the right true vocal fold.
A twenty four years old male patient attended our Apollo ENT Hospital at Jodhpur, Rajasthan with complaint of changes in voice for six to eight months. There was no history of vocal abuse. By profession he was a food delivery guy. There was no history of difficulty or pain while swallowing. He denied any discomfort while breathing. There was no history of recurrent fever, nausea, vomiting, loss of weight or loss of appetite. He had no history of smoking, alcohol consumption, or chronic respiratory diseases. There was no history of blood stained sputum. He had no history of sexual promiscuity or genital warts.
On examination he was sitting well with normal blood pressure. His SpO2 was 99% without any support. Oral cavity examination was normal. Rigid laryngocopy revealed a papillomatous pinkish swelling presented over anterior 2/3rd surface of right true vocal fold. This lesion reaches till anterior commissure and involving the anterior 1/3rd aspect of left true vocal fold.(Figure 1A-C) Both the true vocal folds were mobile with normal rest of the anatomical subsites. Patient underwent for computed tomography (CT) scan and it was reported as 8.3 x 8.8 x 7.1 mm nodular mildly enhancing soft tissue noted at anterior part of the right true vocal cord. (Figure 2) The patient was scheduled for microlaryngeal surgery under general anaesthesia.
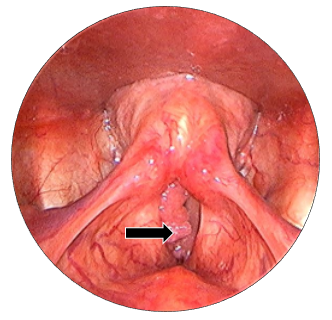
Figure 1C
Figure 1 (A to C) Laryngoscopic view of true vocal folds, showing papillomatous lesion over anterior 2/3rd true vocal fold, involving anterior commissure and left anterior1/3rd true vocal fold. bilateral true vocal folds were mobile.
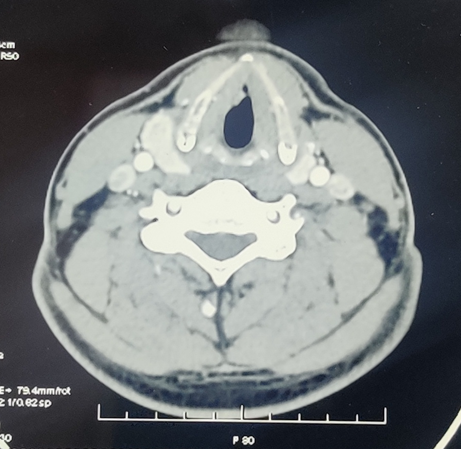
Figure 2 CT scan: 8.3 x 8.8 x 7.1 mm nodular mildly enhancing soft tissue noted at anterior part of the right true vocal cord.
In suspension microlaryngoscopy (SML), (Figure 3) a Lindholm’s laryngoscope is used to expose the entire length of the vocal cords. External pressure can be exerted on the neck to improve the exposure of the anterior laryngeal commissure. The laser was operated using a micromanipulator coupled to an operational microscope. Using the CO2 laser set to ultrapulse mode, 100 mJ/cm2, 10 Hz repetition rate and and 250 m microspot, is used to resect the papilloma, thereby preserving the vocal ligament and normal mucosa at the anterior laryngeal commissure. The surgery is done around a small (6.5mm) endotracheal tube with the laryngoscope placed. Microlaryngoscopic view (Figure 4) showing papillomatous lesion over right true vocal fold. Following the mapping of the papillomas and photographs, cup forceps were used to obtain biopsies, which were then sent for regular pathology. Spot sizes of 0.5-0.8mm provide a comfortable compromise between depth of focus and cutting ability.

Figure 3 Suspension microlaryngoscopy. Surgeon’s both hands are free for using instrumentation during surgery.
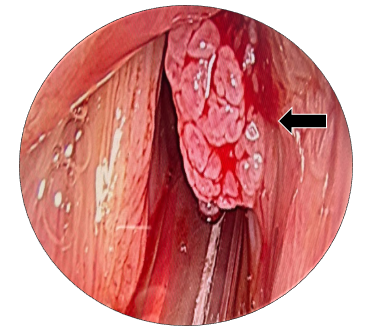
Figure 4 Microlaryngoscopic view of the true vocal folds. Black arrow: papillomatous lesion over right anterior 2/3rd aspect of vocal fold.
Wet swabs, patties, and the cuff of the endotracheal tube may be used to reduce CO2 laser exposure since water absorbs and "neutralises" CO2 laser. The anesthesiologist must keep the FiO2 as low as possible (+/- 30%) to prevent a blow-torch effect in the event that the oxygen in the airways ignites, which will significantly lower the risk of airway fire. To put out a laser fire, it is recommended that a bowl of open water or saline be maintained nearby.
The papillomas were then vaporised using a CO2 laser. Papillomas were removed with a 0.5 to 1mm cuff of surrounding normal-appearing tissue. The submucosal loose areolar tissue (Reinke's space), which is immediately below the papilloma bases, was the target of the excision. Perichondrium and the vocalis muscle were both maintained. (Figure 5) Patient was now in the recovery phase following a successful extubation. On the second day, the patient was sent home with an antacid and antibiotics. The patient was instructed to rest his voice for two weeks in order to promote proper healing around the vocal chord area.
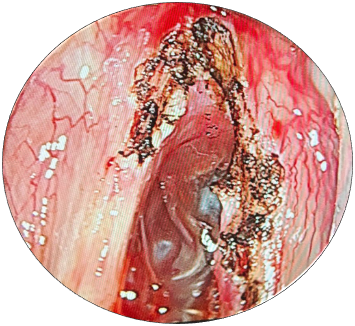
Figure 5 Intraoperative microlaryngoscopic picture after complete removal of papilloma from true vocal folds by CO2 laser.
A histological examination of the specimen was requested. According to the histology report, a papillomatous lesion comprised of multiple finger like fronds with a central fibrovascular core covered by benign hyperplastic stratified squamous epithelium. Basal and parabasal hyperplasia noted. Koilocytic changes noted in upper layers. There was no evidence of dysplasia or malignancy. Overall features suggestive of squamous papilloma. (Figure 6A-D) The postoperative course was uneventful. The patient was discharged on the next day of surgery with oral antibiotics and analgesics. He was advised to avoid voice strain and to drink plenty of fluids. He was followed up at one week, one month, three months, and six months after surgery. He reported significant improvement in his voice quality and had no complaints of hoarseness or dysphonia. Laryngoscopy showed normal healing of the surgical site and no recurrence of the lesion. The patient was advised to continue regular follow-up for at least two years.
A benign growth of squamous papillae in the airways characterises the chronic condition known as laryngeal papillomatosis, which is brought on by the human papillomavirus (HPV). Laryngeal papillomatosis is a rare condition. Derkay stated that there are 1.8 incidences per 100,000 adults annually in the United States.6 According to Cristensen et al., there were 0.2–0.7 cases per 100,000 people in Sweden in 1984.7
It is a benign tumour that primarily affects youngsters, although it is also prevalent in the adult population, with certain series2,8,9 finding a peak incidence in the 20–30 years age range.
The papilloma manifests as an exophytic; branched, pedunculated, or sessile mass, single or several, that is most commonly found on the true vocal folds. Other areas of the laryngeal mucosa may be impacted as well.
Laryngeal papillomatosis is frequently detected after it has progressed in the literature.3,5,10 Our analysis shows an average time of 2 years and 4 months—with extremes ranging from 4 months to 1 year—between the onset of the first symptoms and the initial appointment. The low socioeconomic level in our environment could be used to explain this delay in consultation. Additionally, people with dysphonia frequently downplay the condition in their own minds, and dyspnoea only seldom manifested itself after a protracted period of illness progression.
The primary symptom of the condition in adults is dysphonia. It is an organic dysphonia that is chronic, permanent, and getting worse with time.3,5,11 In contrast to children, adults with laryngeal papillomatosis may have laryngeal dyspnoea of different severity, which can lead to respiratory distress and necessitate an emergency tracheotomy. 5,10,11
This can be explained by the unique anatomical features of the larynx in infants, where an edema of 1mm thickness will shrink the subglottic duct by 50% but an edema of 2.5mm would be required in adults to achieve the same result.17
The larynx can be examined using indirect laryngoscopy or nasofibroscopy, which both allow for visualisation of the papillomas and evaluation of the laryngeal mobility, which is typically intact.3,5 An evaluation of the lesion and a microscopic diagnosis are both possible during the examination while under general anaesthesia. It can be used to spot clusters of lesions that have a raspberry, pink, or greyish appearance.3,10
Papillomas appear as pink or white, sessile or exophytic, pedunculated or broad-based lesions with tiny projections that resemble fronds. Several papilloma clusters can be detected at one or more locations in the airway. Laryngeal papillomatosis has a vascularized core of connective tissue stroma that is covered by many finger-like projections of nonkeratinized stratified squamous epithelium on a histological level.16,17 The expression and synthesis of keratins can vary, and the basal epithelium can range from normal to hyperplastic.17 Cellular differentiation can also be normal or aberrant.
In order to confirm the diagnosis and, especially in adults, to check for malignant change, samples are routinely obtained during endoscopy for histological analysis.
The main method of treatment for laryngeal papillomatosis at the moment is symptomatic.3,10,11 Although several different treatment plans have been created, none of them have been successfully tested. Keeping the airway open and enhancing voice quality are difficult tasks.3
Various techniques are employed to remove papillomas surgically. Debulking and removing the papilloma while preserving the natural structure around it is the goal of surgery.
It is important to take precautions to prevent unintentional tissue damage. An anterior glottic web may emerge as a result of aggressive excision of normal tissue, which can also result in scarring and cause the anterior commissure to rupture. With this, there may be a long-term dysphonia.
Surgical techniques include the use of various lasers, microdebrider and cold-instrument excision.8,19 The modality of choice is determined by the surgeon.
The CO2, potassiumtitanylphosphate (KTP), and pulse dye lasers are only a few of the different types of lasers that we can use to treat this condition.20–23
Laser surgery is one of the more recent approaches to treating papillomas. A carbondioxide (CO2) laser was utilised to treat papillomatosis by 92% of American ENTs, according to a study by Derkay.6 In endoscopic surgery, it is carried out under general anaesthesia12 with the help of microdirect laryngoscopy and the surgical CO2 laser, papilloma excision can be done more thoroughly, completely, and without any bleeding. Removal of obstructive lesions and root ablation of the papilloma have been the main focuses of treatment in an effort to prevent regrowth. The treatment tissue and laser type have an impact on the laser's effect. The interaction of a laser light with a light-activated photosensitizer at a certain wavelength determines the effect.
When compared to cold instruments or the use of a microdebrider, the laser has better visualisation and hemostatic qualities.24 many of the acute airway issues caused by mechanical avulsion are avoided by the comparatively mild postoperative edoema following laser surgery. The use of lasers in laryngeal papillomatosis has some drawbacks, including delayed tissue injury, which can cause interarytenoid scarring and/or fixation, as well as vocal cord stiffness and dysphonia.25
One of the latest treatments for laryngeal papillomatosis, along with the CO2 laser, is the microdebrider.13,14 In fact, a number of medications have been linked to the treatment of RRP in the literature, including bevacizumab (Avastin; Genentech/Roche, San Francisco, CA, USA), aciclovir, propranolol, and indol-3-carbinol. These include cidofovir (Vistide; Merck and Co, Inc., Whitehouse Station, NJ, USA), cimetidine, and ribavirin. Controlling disease progression is the primary objective of adjuvant therapy. Due to the variability of the RRP propensity in each patient, the effectiveness of adjuvant therapy is still unknown.26–31
Since 1998, an additional method of treating recurrence has been intralesional injection of cidofovir following surgical excision of the papilloma.15 However, it continues to be financially out of reach.
The human papillomavirus (HPV) causes laryngeal papillomatosis, which presents as a benign growth of squamous papillae in the airways. Treatment is difficult. Thus, early, proper diagnosis and cautious treatment choices are necessary to limit the risk of recurrence and spread of lesions throughout the airways.
The procedure performed in this case report was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
For the purpose of publishing this case report, the patient's written informed consent was obtained.
None.
The author (s) declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this paper.

©2023 Goyal, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.