Journal of
eISSN: 2379-6359


Research Article Volume 11 Issue 5
1Phoniatric Unit, Otorhinolaryngology department, Ain Shams University, Egypt
2Phoniatric Unit, Otorhinolaryngology department, Cairo University, Egypt
3Physical medicine and rehabilitation department, Menoufia University, Egypt
4Phoniatric Unit, Otorhinolaryngology department, Menoufia University, Egypt
Correspondence: Eman Ezzat Abd El Wahed Ismail, Phoniatric Unit, Otorhinolaryngology department, Faculty of Medicine, Menoufia University, Menoufia, Egypt, Tel +2-01007106778, Fax 002-048-2222303
Received: September 07, 2019 | Published: September 19, 2019
Citation: Baraka M, ElDessouky H, Labeeb AAA, et al. Laryngeal complaints and videolaryngoscopic laryngeal alterations in rheumatoid arthritis patients and its association with disease activity and duration. J Otolaryngol ENT Res. 2019;11(4):216?223. DOI: 10.15406/joentr.2019.11.00438
Background: Rheumatoid arthritis (RA) is an autoimmune systemic disease with a wide clinical presentation. The laryngeal manifestations are often masked by the articular disability often experienced in the early and late stages of the disease.
Objective: Association between different laryngeal complaints and videolaryngoscopic laryngeal alterations in patients with RA, and disease activity and duration.
Patients and methods: A retrospective study was conducted on 79 patients with RA. All subjects were recruited from the out-patient clinic of physical medicine, rehabilitation, and rheumatology in Al-Menoufia University Hospitals during the period from March 2015 to March 2017. All patients were subjected to both phoniatric and rheumatological assessment.
Results: Patients with phonasthenic symptoms and globus pharynges had significantly (p=0.01, 0.008 respectively) higher disease duration than patients without. No significant association found between rheumatoid arthritis duration and different videolaryngoscopic laryngeal alterations, patient’s self-assessment of the impact of laryngeal complaints on their lives, and auditory perceptual assessment (APA) of patient’s voice characters. As regards rheumatoid disease's activity no significant correlation has been established (p>0.05) with different laryngeal complaints except for patients in remission who had higher prevalence of intermittent dysphonia than patients with low activities. Rheumatoid disease's activity had no significant association with different laryngeal findings except those with moderate activity; they had significantly higher prevalence of vocal folds nodules than patients with high activity and patients in remission.
Conclusion: A significant association between the disease's duration and presence of laryngeal complaints, dysphonia, and its persistence has been established. Also, patients with phonasthenic symptoms and globus pharynges had significantly higher disease duration than patients without. Rheumatoid diseases activity had significant association with different laryngeal complaints in patients with remission that had higher prevalence of intermittent dysphonia than patients with low activities. No significant association between the disease activity and different laryngeal findings that has been found except for patients with DAS-28>3.2, they had significantly higher prevalence of rheumatoid nodules.
Keywords: disease's duration, laryngeal complaints, rheumatoid arthritis larynx, videolaryngoscopic findings, rheumatoid nodules
RA, rheumatoid arthritis; EAMs, extra-articular manifestations; DMARD, disease-modifying anti-rheumatic drugs
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease of unknown cause. The main feature of this disease is persistent symmetric polyarthritis (synovitis) that involves mainly the peripheral small joints but can affect any synovial joint in the body and can cause extra-articular manifestations (EAMs). RA is characterized by repeated attacks of remissions and exacerbations with variable outcomes ranging from leaving no damage to a severe disability and even death.1 RA affects mainly women between 30 and 50 years of age. The prevalence of RA in the adult population through the world is approximately 0.5% to 1% and its incidence is about 20 to 50 cases per 100,000 people.2 Being more incident in females than males with three times more in females makes sexual hormones explain one more etiological theory of RA.3 Complications of RA can begin to develop within several months since the appearance of the clinical symptoms, so immediate referring to rheumatologists or their consultation are necessary for the beginning of treatment with disease-modifying anti-rheumatic drugs (DMARD).4
Laryngeal manifestations in patients with RA are usually benign and subclinical. Early symptoms are dysphonia/change of voice character, and globus pharynges/sense of sticky foreign body in the throat. Afterwards, patients experience odynophagia, sore throat, dry irritative cough and dyspnea.5 About 66% of the laryngeal symptoms in patients with RA are related to cricoarytenoid joint (CAJ) involvement. Cricoarytenoid arthritis is a potential cause of acute obstruction of the airway, compromising vocal fold (VF) mobility and causing edema, which sometimes requires tracheostomy.6 Rheumatoid nodule is another highly specific laryngeal findings of RA that may be mild and diagnosed only through videolaryngoscopy (VL) or through histopathology, or until it becomes exuberant, in a bamboo shape.7 Voulgari et al.,8 reinforced the need for more prospective studies in different communities on the laryngeal involvements in RA.
In Egypt, the knowledge regarding RA manifestations in the larynx, as well as its respective statistical data is limited. The condition is, however, rather uncommon and the precise diagnosis is difficult to settle.5 VL is a minimally invasive clinical tool that allows the clinician to identify the etiology of voice disorders through providing images of the larynx in high resolution. Although VL is a standard technique in otolaryngology, there is little information on using VL for laryngeal involvement in patients with RA. A large part of the papers on this topic are limited to case reports or are associated with small patient samples.9 Early recognition and initiation of treatment are crucial in sparing the laryngeal chronic deformities and can be life threatening. Treatment consists mainly of administration of high doses of steroids systemically or locally into the CAJ.5 The aim of this study was to assess the association between different laryngeal complaints mainly dysphonia and laryngeal changes upon videolaryngoscopic examination of patients with RA on one side and disease activity and duration on the other side.
A retrospective clinical cross sectional study was conducted on 79 patients with RA. All subjects were recruited from the out-patient clinic of physical medicine, rehabilitation and rheumatology in Al-Menoufia University Hospitals during the period from March 2015 to March 2017.
Inclusion criteria: patients had to be definitely diagnosed as having RA according to the American colleague of rheumatology (ACR) criteria 2010,10 at least 20years old at the time of symptoms onset and under medical treatment for at least one year.
Exclusion criteria: Patients with; previous orotracheal intubation for 24 hours or more, documented head and neck cancer, head and neck radiotherapy, reflux or allergic laryngitis/pharyngitis, laryngeal surgery, central or peripheral neurologic disorders, and those having collagen disease other than RA are excluded from the study.
Every patient has been subjected to both phoniatric and rheumatological assessment as follows:
Phoniatric assessment was carried out on the basis of precise phoniatric interview including: identification data (name, age, sex, marital status, occupation, vocal demand, and special habits as smoking), data of RA (time of onset, its duration, extra-articular manifestations, and therapy), laryngeal complaints (dysphonia, cough, difficulty of breathing or swallowing, phonasthenic symptoms or globus pharynges), and elfperception ofb the voice via voice capacity self-assessment questionnaire using Arabic version of Voice Handicap Index (VHI),11 self-perception of the voice.
VHI questionnaire is divided into 3v domains; nfunctional, physical, and emotional. Each domain contains 10 questions with their scores range from 0 to 4 (0=normal, 4=severe affection). The final score based on summation of the 3 domains' scores (0= absent, 0-30= mild, 31-6-= moderate, and 61-120= severe). The higher the score, the more severe is the voice handicap. The auditory perceptual assessment (APA) of the patients’ voice quality was performed by three different experienced speech pathologists of not less than 10 years of experience. Evaluation was performed evaluations and taking the mean value for the study using the modified GRBASI scale for voice perceptive-auditory analysis12 as shown in (Table 1).
Overall grade (G) of dysphonia . |
|
Character (quality): |
R - roughness; B - breathiness; A - asthenia; S - strain I - instability. |
Absence or presence and degree of severity according to 4-point scale as follows: |
0 - absent; 1 - mild; 2 - moderate and 3 - severe . |
Register: Habitual register: |
modal, Falsetto or fry. |
Presence or absence of register break Pitch |
overall increased, decreased or diplophonia. |
Loudness: |
loud, soft or fluctuating. |
Glottal attack: |
normal, soft or hard. |
Associated laryngeal functions: |
Cough, whisper and laugh. |
Both loudness and pitch levels were scored on a 7-point scale: |
severely reduced (1), moderately reduced (2), mildly reduced (3), normal (4), mildly elevated (5), moderately elevated (6), and severely elevated (7 |
Breathiness, leakiness, irregularity and overall grade, were rated on a 4-point scale: |
normal (0), mild (1), moderate (2), and severe (3) |
Diplophonia was evaluated on a 4-point scale: |
none (0), occasional (1), frequent (2), and constant (3) |
Table 1 The modified GRBASI scale for voice perceptive-auditory analysis
VL was performed using a digitalized Videolaryngoscopic system manufactured by Italian Inventis company (M-900-01003-0001- High Light model plus-LED), Invisia's MediCam plus camera with Charge-Coupled Device (CCD) sensor of high sensitivity 1280×960pixels, rigid oral 90-degree angle telescope model Hipp E 2690, fiber-optic light cable 4.8×1800mm, and autoclavable with Storz adapters on both sides. The software used is Inventis Daisy software system 3.6.3B3 with Visia module developed by Inventis Company. The data gathered from patients' laryngeal complaints, APA, VHI and VL were tested for possible correlations with RA duration and activity.
Rheumatological evaluation of the patients was carried out through delicate clinical examination, assessment of the disease activity using DAS-28 covering 28 joints that entails tenderness and swelling in 28 joints, and global visual analog scale (VAS) with assessment range 0–10, and concentration of C-reactive protein, hemoglobin, platelet counts, serum creatinine, and urine analysis for assessing urinary protein excretion.
Statistical analysis: Analysis of data was done by DELL computer using Statistical Package for the Social Sciences (SPSS), Version 23 (SPSS Inc., Chicago, IL, USA) as follows: Description of quantitative variables as mean, and standard (SD). Description of qualitative variables, as number or frequency and percentage, through student's t-test, Chi-Squared (χ2), Fisher's exact test, and P-value (< 0.05 was considered significant difference, >0.05 was considered non-significant difference, while < 0.001 was considered a highly significant).
In the current study, the mean age of the studied patients was 47.11±8.72 years and mean RA disease duration was 10.10±7.53years. Most of the patients were females (female: male ratio was 78:1). Also, 88.6% of the patients were housewives while, 6.3% were teachers and 5.1% worked in other jobs. A significant relation has been established between disease's duration and presence of laryngeal complaints regarding dysphonia (p=0.021) and its persistence (p=0.034). Also, patients with phonasthenics symptoms and globus pharynges had significantly higher disease duration than patients without (p=0.01, 0.008 respectively). On the other hand, no significant association has been established (p>0.05) between the disease's duration and laryngeal complaints regarding cough, dyspnea or difficulty of swallowing. In addition to, no significant association between the disease's duration and patient’s self-assessment of the impact of laryngeal complaints on their lives has been detected. As regard VHI, there was a highly significant relation between the disease's duration and VHI score as those who had moderate score of VHI had had longer disease duration (the longer the duration, the more the voice affected by self assessment). These patients had significantly longer disease duration than patients with mild VHI (p<0.001), (Table 2).
Variables |
Duration |
Test of sig |
P value |
Presence of laryngeal c/o: Absent |
7.73 ± 5.96 |
U=2.30 |
0.021* |
Cough: Absent |
10.26 ± 7.60 |
U=1.01 |
0.31 |
Change of voice character (dysphonia): Absent |
8.83 ± 7.17 |
U=2.30 |
0.021* |
Persistence of dysphonia: Persistent |
14.10 ± 8.34 |
U=2.21 |
0.034* |
Dyspnea: Present |
10.10 ± 7.53 |
------ |
------ |
Difficulty of swallowing: Absent |
10.17 ± 7.65 |
U=0.01 |
0.99 |
Phonasthenic symptoms: Absent |
8.26 ± 5.88 |
U=2.52 |
0.01** |
Globus pharynges: Absent |
7.64 ± 5.92 |
U=2.67 |
0.008** |
Impact of complaint on patient’s life: |
9.80 ± 7.31 |
F=1.52 |
0.22 |
VHI: Mild |
4.35 ± 9.16 |
U=4.87 |
<0.001** |
Table 2 The association of rheumatoid disease duration with different laryngeal complaints and different patient’s self-assessment scores
U =Mann Whitney test. *= significant= P value < 0.05, ** highly significant= p<0.001
As regarding APA; 62 patients had percept as having voice changes. Twenty two patients had mild dysphonia and roughness, 17 had mild voice instability, 13 had straining, and 3 had mild breathiness. Fifteen patients had low pitched voice [9 mild reduced (3), and 6 moderately reduced (2)]. No patients had leakiness, diplophonia, or asthenia. There was no statistical correlation between different parameters of APA and both disease duration and activity (Table 3).
APA parameters |
Activity |
Fisher’s Exact test |
P value |
||||
Low |
Moderate |
High |
Remission |
||||
Grade of dysphonia |
0 |
6(75.0%) |
21(70.0%) |
18(75.0%) |
12(70.6%) |
3.38 |
0.17 |
1 |
2(25.0%) |
9(30.0%) |
6(25.0%) |
5(29.4%) |
|||
2 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
3 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
Roughness |
0 |
6(75.0%) |
21(70.0%) |
18(75.0%) |
12(70.6%) |
3.38 |
0.17 |
1 |
2(25.0%) |
9(30.0%) |
6(25.0%) |
5(29.4%) |
|||
2 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
3 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
Straining |
0 |
7(87.5%) |
25(83.3%) |
20(83.3%) |
14(82.4%) |
3.12 |
0.11 |
1 |
1(12.5%) |
5(16.7.0%) |
4(16.7%) |
3(17.6%) |
|||
2 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
3 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
Voice instability |
0 |
7(87.5%) |
23(76.7%) |
19(79.2%) |
13(76.5%) |
3.04 |
0.35 |
1 |
1(12.5%) |
7(23.3%) |
5(20.8%) |
4(23.5%) |
|||
2 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
3 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
Breathiness |
0 |
8(100.0%) |
29(96.7%) |
23(95.8%) |
16(94.1%) |
3.79 |
0.27 |
1 |
0(0.0%) |
1(2.3%) |
1(4.2%) |
1(5.9%) |
|||
2 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
3 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
Pitch |
1 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
1.06 |
0.48 |
2 |
0(0.0%) |
3(10.0%) |
1(4.2%) |
2(11.8%) |
|||
3 |
1(12.5%) |
3(10.0%) |
3(12.5%) |
2(11.8%) |
|||
4 |
7(87.5%) |
24(80.0%) |
20(83.3%) |
13(76.4%) |
|||
5 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
6 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
7 |
0(0.0%) |
0(0.0%) |
0(0.0%) |
0(0.0%) |
|||
Table 3 The association of rheumatoid disease activity and APA parameters
Also, RA disease duration hasn't been significantly correlated with different video-laryngoscopic findings (rheumatoid nodules, posterior laryngitis, diffuse laryngitis, and glottic gap and VF immobility). In our study, no significant association has been established (p>0.05) between rheumatoid disease's activity and different laryngeal complaints as dysphonia, cough, dyspnea, difficulty of swallowing, phonasthenic symptoms and globus pharynges except for patients in remission who had higher prevalence of intermittent dysphonia than patients with low activities (p=0.01). Also patients with low activity had significantly higher moderate scores of VHI index than both patients with high activity and those in remission (p=0.01 and 0.04 respectively) (Table 4).
|
Activity |
Fisher’s Exact test |
P value |
|||
Low |
Moderate |
High |
Remission |
|||
Presence of laryngeal complaint: |
1 (12.5) |
15 (50.0) |
10 (41.7) |
6 (35.3) |
3.79 |
0.28 |
Cough: Absent |
8 (100.0) |
30(100.0) |
22 (91.7) |
15 (88.2) |
3.84 |
0.24 |
Change of voice character (dysphonia) |
4 (50.0) |
17 (56.7) |
17 (70.8) |
13 (76.5) |
3.02 |
0.38 |
Persistence: Persistent |
2 (50.0) |
4 (30.8) |
4 (57.1) |
4 (57.1) |
3.44 |
0.11 |
Dyspnea: Absent |
8 (100.0) |
30(100.0) |
24(100.0) |
17 (100.0) |
--- |
----- |
Difficulty of swallowing: Absent |
8 (100.0) |
30(100.0) |
23 (95.8) |
15 (88.2) |
3.66 |
0.18 |
Phonasthenic symptoms: Absent |
5 (62.5) |
21 (70.0) |
17 (70.8) |
10 (58.8) |
1.02 |
0.84 |
Globus pharynges: Absent |
2 (25.0) |
16 (53.3) |
13 (54.2) |
6 (35.3) |
3.35 |
0.36 |
Impact of complaint on patient’s life: |
3 (37.5) |
22 (73.3) |
21 (87.5) |
17 (100.0) |
13.99 |
0.009** |
VHI: Normal |
3 (37.5) |
22 (73.3) |
21 (87.5) |
13 (76.5) |
17.79 |
0.03* |
Table 4 The association of rheumatoid disease activity and different laryngeal complaints and VHI scores
The current study showed that, rheumatoid disease's activity has no significant association (p>0.05) with different laryngeal findings as presence or absence of VL findings, posterior laryngitis, diffuse laryngitis and glottis gap except those with moderate activity that had significantly higher prevalence of VF nodules than patients with high activity (p=0.002) and patients in remission (p=0.01) (Table 5) (Figure 1-3).
|
Activity |
Fisher’s Exact test |
P value |
|||
Low |
Moderate |
High |
Remission |
|||
Videolaryngoscopic findings: |
1 (12.5) |
7 (23.3) |
3 (12.5) |
0 (0.0) |
4.95 |
0.14 |
Reumatoid nodules: Absent |
6 (75.0) |
16 (53.3) |
22 (91.7) |
14 (82.4) |
10.63 |
0.01** |
Posterior laryngitis: |
1 (12.5) |
8 (26.7) |
6 (25.0) |
2 (11.8) |
1.77 |
0.65 |
Diffuse laryngitis: Absent |
8 (100.0) |
30 (100.0) |
22 (91.7) |
17 (100.0) |
3.29 |
0.32 |
Glottic gap: Absent |
4 (50.0) |
17 (56.7) |
16 (66.7) |
14 (82.4) |
4.19 |
0.23 |
VF immobility: Absent |
8 (100.0) |
30 (100.0) |
24 (100.0) |
17 (100.0) |
----- |
----- |
Table 5 The association of rheumatoid disease activity and different Videolaryngoscopicindings
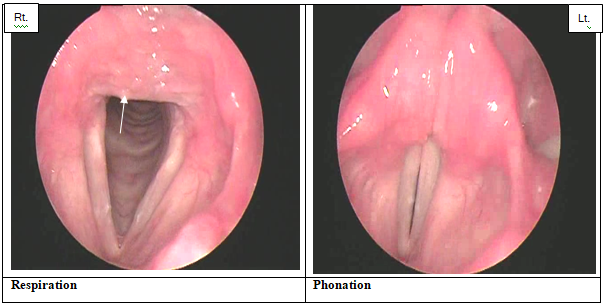
Figure 1 55years old female complaining of globus pharynges with severs posterior laryngitis and edema (15 years’ duration and moderate activity).
In the current study a significant association has been recorded between disease's duration and presence of laryngeal complaints regarding dysphonia (p=0.021) and its persistence (p=0.034). Also, there was a significant relation between presence of phonasthenic symptoms and globus pharynges and disease duration. No significant association has been found between the disease duration and laryngeal complaints regarding cough, dyspnea, or difficulty of swallowing. Laryngeal involvement has been described to be more likely present in RA patients with disease duration longer than ten years in the literatures.6,13 A study made by Beirith et al.,14 concluded that the long duration of the disease is not a risk factor regarding the laryngeal involvement or presence of laryngeal complaints. Another study made by Bozbas et al.,15 on a total of 82 subjects consisting of 42 patients with RA and 40 non-RA patients in the control group with a mean disease duration 6.2±6.3years. They found that no correlation is established between the disease duration and presences of laryngeal complaints. Eighty-six patients with RA were recruited from the Rheumatology and Rehabilitation outpatient of Assiut University Hospital by Gamal et al.,16 to assess the impact of RA on the health-related quality of life (QoL) of patients, using the 36-item short form (SF-36) and they found that, the quality of life is impaired in Egyptian RA patients and disease duration was the most significant predictor. They recommended routine assessment of the health-related QoL in those patients to detect and monitor the impact of the disease and medications used on different aspects of their quality of life.
As regards VHI patients who reported moderate VHI scores had significantly longer disease duration than patients with mild VHI scores (Table 2). Against our results a study made by Beirith et al.,14 that detected lower VHI results in patients with RA duration (6.36±10.82) in contrast to the control group patients (13.15±13.78). The prevalence of results higher than 15 points - cutting point utilized by Speyer et al., suggesting dysphonia, was 42.3% lower in patients with RA when compared to the control group; however, this data was not statistically significant (p = 0.064). De Castro et al.,17 agreed with our finding as they concluded that, despite the lack of statistical significance, patients with complaints of dysphonia had RA for longer durations. They also analyzed acoustic measures that revealed the worse results in patients with RA for longer than 10years.17
The present study indicated that rheumatoid disease's duration has no significant correlation with different video-laryngoscopic findings (rheumatoid nodules, posterior laryngitis, diffuse laryngitis, glottic gap, and VF immobility). In agreement with us the study made by Castro et al.,17 in which no statistical correlation was found between VL findings and duration of disease or complaint of dysphonia. Also, Voulgari et al.,8 reported that, 13 (27.75%) of their subjects had disease duration of less than 15 years, of whom 11 (84.6%) had normal VL findings while the 34 (72.3%) patients with disease duration longer than 15 years, 18 (52.9%) had some type of change seen upon VL (p= 0.025). Overriding arytenoids was the main laryngoscopic finding in a study made by Castro et al.,17 in contrasted to only five patients had positional asymmetry. Other frequent findings were arytenoids edema, anterior phonatory gap, and angiodysgenesis. That were reported in the current study in 62,28,14 patients respectively even with no statistical significant with the diseased duration. In a study made by Bozbas et al.,15 they concluded that the disease duration was not found to be correlated with the laryngeal involvement as in the previously conducted studies.6,13
In this study, no significant association has been found (p>0.05) between rheumatoid diseases activity and different laryngeal complaints as presence of laryngeal complaint; cough, dyspnea, difficulty of swallowing, phonasthenic symptoms and globus pharynges. Except for patients in remission who had higher prevalence of intermittent dysphonia than patients with low activities (p=0.01). Patients with low activity had significantly higher moderate scores of VHI index than both patients with high activity and patients in remission (p=0.01 and 0.04 respectively), (Table 4). These results may be explained by longer duration of the disease in the group of patients in remission included in our study. Results of Kosztyła-Hojna and Kuryliszyn,18 study supported a relationship between the presence of dysphonia and activity of rheumatic process. Features of dysphonia were registered more frequent in 29 (58%) patients, in the group of patients with DAS-28 ≥3.2, in comparison with the group with mild activity of RA, in which voice disorders were observed only in 3 (13.64%) patients. Supporting our results another study in which no clear associations were found between the activity of RA scored by the patient as well as by the rheumatologist on one hand, and the severity of the voice disorder or the VHI total score on the other hand.19 Against our result a study made by Castro et al.,17 that revealed a statistical correlations between VHI (physical and total) scores and RA state of activity, and VHI (all domains) scores and complaint of dysphonia. This may be explained by the fact that the VHI is a self-perception vocal handicap index. All RA patients with voice impairment in study conducted by Fisher et al.,20 had active disease as defined by a DAS-28 score >3.2, and participants with active disease had significantly higher VHI-10 scores (p=0.0261). Higher VHI-10 scores were seen in patients with a DAS-28>3.2 suggesting a relationship with disease activity.
The current study showed that, rheumatoid diseases activity has no significant association with different laryngeal findings on VL assessment as presence or absence of VL findings; posterior laryngitis, diffuse laryngitis, glottic gap, and VF immobility. Except those with moderate activity, they had significantly higher prevalence of VF nodules than patients with high activity and patients in remission, (Table 5). In a study made by Voulgari et al.,8 74.3% of the patients of his study with DAS-28 > 2.6 had some type of disorder seen upon the VL (p = 0.713). A wide range of laryngoscopic findings has been described in a study made by Castro et al.,17 overriding arytenoids was the main laryngoscopic finding in their study, and five patients had positional asymmetry. Other frequent findings were arytenoid edema and angiodysgenesis. However, statistical correlation was identified only between RA activity and the laryngostroboscopic finding of overriding arytenoid cartilages. Indeed, overriding occurs as a consequence of cricothyroid arthritis and ankylosis, and such finding develops as the disease progresses. Hah et al.,21 did not find an association between RA and organic laryngeal lesions/subjective voice discomfort except in the participants with laryngitis. In the study made by Bozbas et al.,15 no correlations were found between the nasopharyngeo laryngoscopic findings and disease activity.
The current study concluded that a significant association has been established between the disease's duration and presence of laryngeal complaints, dysphonia and its persistence. Also, patients with phonasthenic symptoms and globus pharynges had significantly higher disease duration than patients without. While, rheumatoid disease's activity hasn't been significantly associated with different laryngeal complaints and different laryngeal findings except for patients in remission who had higher prevalence of intermittent dysphonia than patients with low activities. Also, for patients with DAS-28>3.2, they had significantly higher prevalence of VF nodules.
The study protocol had been approved by Ethical Scientific Committee of Menoufia University and informed consents were taken from all subjects before their enrollment in the study.
Would like to express my deepest thanks to all subjects for their cooperation.
No conflicts of interest declared.
This research was carried out without funding.

©2019 Baraka, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.