Journal of
eISSN: 2379-6359


Review Article Volume 14 Issue 1
1Capitulo de estetica orofacial, Region V Chile
2Instituto Neurobalance, Chile
Correspondence: Constanza Angulo K, Capítulo de estética orofacial, Región V Chile, Avenida Bosques de Montemar 30 of. 613 Vina del Mar, Chile, Tel +57994371372
Received: April 26, 2022 | Published: May 4, 2022
Citation: Constanza AK, Marta AM, Ignacio NC, et al. Facial artery, an essential anatomy in different specialties: a review. J Otolaryngol ENT Res. 2022;14(1):14-20. DOI: 10.15406/joentr.2022.14.00498
The facial artery presents various patterns of anatomical distribution. Its collaterals and terminal branches require permanent review by professionals who perform invasive and minimally invasive procedures in the face territory. The varied anastomoses of the territory of the external carotid and the ophthalmic artery -coming from the Internal Carotid-make it necessary to act with caution against possible complications when minimally invasive procedures are performed such as the injection of "filler" (mainly hyaluronic acid) for aesthetic purposes. That is why the clinical analysis prior to any procedure at the face level makes it necessary to integrate an analysis of the detailed knowledge of the tremendous anatomical variability of the facial artery, which will allow better results, less morbidity, and minimize the risks of vascular complications.
Keywords: Facial artery, Facial flap, Computed tomography
The facial artery (FA) is a collateral branch of the external carotid artery which generally emerges anteriorly, at the limit of the inferior border of the digastric muscle and caudal to the mandibular angle, ascending obliquely anteriorly, giving rise to the blood vessels responsible for supply blood to the face.1 FA describes a course that can be delimited according to its course in arteries: buccal, labial, nasolabial fold, angular nasal, dorsal nasal, and glabellar connection. Previous studies have shown a racial variation in the origin of the branching pattern and distribution patterns.2 However, each patient has individual variations, even in their literalities, left and right.3
Vascular complications of the facial territory will be related to the possible interventions of each specialist, from artery puncture, extravascular compression, and erroneous delimitation of the mucous muscle flap of the facial artery (FAMM), blindness or necrosis.4 For this reason, it is essential to know the course of FA, its ramifications, variations, and anatomical relationships, allowing different surgical actions and minimally invasive procedures with more excellent safety and efficiency, thus minimizing iatrogenesis and complications.
The increase in interventions in the facial territory in the last 15 years has led to a directly proportional relationship to the increase in research and available scientific evidence; Although the general anatomy of the area, including the variations of the facial artery and its branches, have been described previously, to date there is no review of the literature that combines analytical data to estimate the prevalence of anatomical variations of the facial artery more accurately FA.
Due to the above, the objective of this review is to synthesize the existing evidence in the literature referring to studies of the path and anatomical variations, anastomoses, and diameters of the FA, providing reliable evidence that allows various surgical minimally invasive procedures to be carried out safely, and lower morbidity.
A literature research was performed using the keywords: "Facial artery," "Flap," "Computed tomography," "Cadaveric study," and "Anatomy" to identify all articles related to FA. Anatomical descriptions of this artery, variations in its route, and its relationship with different surgical and minimally invasive procedures were reviewed. Those articles that did not specifically contain FA as an element that allowed the analysis of its anatomical variations, path, diameter, and other characteristics were excluded. No language restrictions or publication methodologies were imposed. We used the above exclusion criteria; 107 articles were considered for detailed review. The included bibliography was analyzed and read by two independent reviewers who obtained the most relevant data in this study.
Development
Common Carotid Artery, its bifurcation, and variations
The bifurcation of the carotid artery occurs at different levels with projection on the spine, in a frequency of 55% at the level of C3 and 35% at the level of C4 on the right side, while on the left side, it occurs in a 60% and 40% respectively.1 However, a case of high bifurcation of the common carotid artery C2 and C3, the origin of the ascending pharyngeal artery from the trunk of the common carotid artery, and anomalous branching pattern of the external carotid artery, is reported in the literature. This incidence is 1%.5 the external carotid artery mainly supplies the face, and the oral and nasal cavities, whereas the internal carotid artery supplies the brain and the cranial vault,6 these present multiple anastomoses along their course, generating an intracranial and extracranial communication. The external carotid artery emerges as a division of the common carotid artery, and it presents variations in its origin and course that are not unknown to many.
The FA emerges approximately at the lower border of the digastric muscle and under the mandibular angle as the linguofacial trunk from the external carotid artery in a proportion of 20%, on other occasions, 2.5% of the FA has been seen to emerge forming the thyrolinguofacial trunk or separated from the trunk formed by the lingual and superior thyroid artery.1 An unusual course of the excellent FA arising from the external carotid artery on the mandibular angle is also reported.7 A case is reported in which the common carotid artery independently gives rise to the thyroid artery, lingual artery, facial artery, internal and external carotid artery.1 On the other hand, FA presents unusual branches in some patients, including the ascending pharyngeal, superior laryngeal, tonsillar, sternocleidomastoid, maxillary, or sublingual branches. These abnormalities and differences in the branching pattern of the external carotid artery and anatomical variants of FA are of clinical importance when performing surgical and minimally invasive procedures in the head and neck region.
Facial artery (FA)
The literature describes five main patterns of topographic and morphological distribution of the facial artery, in 47.5%, the FA bifurcates into the superior labial artery and the lateral nasal artery that ends as the angular artery; in 38.7 %, the facial artery ends as the superior alar artery; 8.4% ends in the superior labial artery; 3.8% have an angular branch that emerges below the oral commissure from the trunk of the FA, ending its course as the superior alar artery, and in 1.4% it ends as a rudimentary branch without the presence of superior labial or lateral nasal or angular arteries (Figure 1).8

Figure 1 Anatomical variations of terminal branches of the facial artery, five types A to E. Loukas M, Hullett J, Louis RG Jr, et al. A detailed observation of variations of the facial artery, with emphasis on the superior labial artery. Surg Radio Anat. 2006 Jun;28(3):316-24.
At the same time, its location can vary concerning the nasolabial fold, with FA being medial in 42.9% and lateral in 23.2%; on the other hand, it can cross this groove laterally in 19.6% or medially in 14. 3% (Figure 2).9

Figure 2 Location of the facial artery (FA) about the nasolabial fold (SNL), % distribution. Upper Left FA medial to the SNL. Upper right FA lateral to SNL. Lower Left FA is medially crossing SNL. Lower right AF laterally crossing the SNL.
The FA in its mandibular segment emerges through the mandibular angle anterior to the facial vein and can be found separated from the lingual artery, forming the linguofacial trunk or forming the thyrolinguofacial trunk, in a deep or supraperiosteal layer.6 In the buccal segment, the FA enters the buccal space by being 1 to 2.5 cm behind the corner of the mouth, between the deep buccinator muscle, the modiolar part of the platysma, and the convergence of the muscles of facial expression.10 The FA gives rise to the superior and inferior labial arteries; in 70%, this segment is detached below the oral commissure, 25% above, and 5% at its level.8 Regarding the distribution of the labial arteries, it is described that these can be found in 78.1% in the submucosa, 17.5% intramuscular, and 2.1% subcutaneously, these planes do not vary in 71% in the superior labial artery and 67% in the lower one, however, we must consider that a not lesser percentage varies between the planes.11
The superior labial artery presents four distribution patterns; in 56.7%, the superior labial artery and the alar branch arise directly and separately from the FA (Type I); in 21.7%, it arises directly from the FA and emits an alar branch (Type II), in 15% it is considered a terminal branch of the FA (Type III) and 6.7% have an absence of the superior labial artery (Type IV) (Figure 3).12

Figure 3
Diagrams of the four types of the superior labial artery (SLA)
Type I: ALS and the alar branch arise directly and separately from the Fa.
Type II: ALS arises from the FA and gives an alar branch.
Type III: ALS is the terminal branch of FA.
Type IV: ALS absent.
ANG, angular artery; A, An alar branch; SLA, superior labial artery; ILA, inferior labial artery; FA, facial artery. Lee SH, Gil YC, Choi YJ, Tansatit T, Kim HJ, Hu KS. Topographic anatomy of the superior labial artery for dermal filler injection. Plast Reconstr Surg. 2015 Feb;135(2):445-450.
The FA is renamed the angular artery when it gives its branch forming the superior labial artery; this in the nasolabial fold becomes more superficial approaching the dermis. However, it varies between individuals and has the same laterality. Four patterns of distribution of the angular artery are described in the literature. In 19.3%, the pattern defined as "persistent" is one in which the artery originates at the branch point of the lateral nasal artery from the FA adjacent to the ala of the nose (A); in 31.6%, the "deviated pattern" in which the angular artery traverses continuously from the deviation branch of the FA (B) and ascends vertically in the nasojugal and medial canthal areas, in a 22.8% the "alternative pattern" in which the angular artery originates from the ophthalmic artery in the medial canthal area (C) and in 26.3% the "latent pattern" in which the FA ends in the nasolabial area without a break off a branch (D). A higher frequency of the "alternative pattern" and the "latent pattern" was found when a medial band of the orbicularis oculi could be involved in developing the angular artery (Figure 4).13

Figure 4 Schematic illustrations showing the four displacement patterns of the Angular Artery (AA)
A. Persistent pattern in which the AA originates from the FA LNA branch point adjacent to the alae nasi.
B. Deviation pattern in which the AA continuously traverses from the deviated branch of the FA and ascends vertically to the nasojugal and medial canthal areas.
C. Alternative pattern in which the AA originates only in the ophthalmic artery.
D. Latent pattern in which FA ends around the nasolabial area without emitting AA.
The arrows indicate the route of blood flow in the arteries.
As the angular artery approaches the medial canthus, it emits branches on the lateral face of the nose and connects with the infraorbital artery.14 The dorsal nasal or lateral nasal artery is in the subcutaneous plane. It emerges from the orbit and pierces the orbital septum superior to the medial canthal ligament. It extends below the orbicularis oculi muscle and connects with the contralateral dorsal nasal artery at the origin of the procerus muscle.6 In the glabellar area, both dorsal nasal arteries are related to the supratrochlear and supraorbital arteries.
Some authors classify FA according to its terminal branches. However, they do not describe the definition of the terminal branch, generating some degree of confusion.15 The literature describes the premasseteric artery, the superior and inferior labial artery, the nasal artery, and the angular artery as terminal branches.16 One study classified FA according to its terminal branches into three patterns, finding a predominant nasolabial pattern in 51.8% (Type I), a nasolabial pattern with an infraorbital trunk in 29.6% (Type II), and an 18.6% had a forehead pattern (Type III), at the same time these patterns were subdivided according to their depth and relationship with the facial muscle layer.2
The nasolabial pattern presents two different relationships with the muscle layer; in 37.0% of the FA, it is covered by the platysma and the depressor of the angle of the mouth (Type Ia); when detaching a branch of the inferior labial artery, it is covered by the depressor of the inferior lip. The FA is anterior to the buccal fat pad between the risorius and zygomaticus major in the lateral modiolar region. Superior to the angle of the mouth, the inferior labial artery and the superior labial artery separate from the FA, superficial to the orbicularis oris, before reaching the border of the superior and inferior labial vermillion. The FA then ascends deep to the levator labii superioris and the levator labii superioris y ala nasalis. In the nasal alar region, the inferior alar artery and the lateral nasal artery supply and give off branches that go from the columella and the nose to the elevator lip muscle and the zygomaticus minor. On the other hand, in 14.8% of the nasolabial pattern (Type Ib), all branches of the FA are located deep in the facial muscles. If we refer to the nasolabial pattern with an infraorbital trunk, 16.7% travel similarly to the previously mentioned type covered by the facial muscles (Type IIa). However, the infraorbital trunk advances into the infraorbital area, superficial to the zygomaticus major and deep to the zygomaticus minor. It then turns medially to the nasojugal area along the inferior border of the orbicularis oris and superficial to the Levator labii superioris alaeque nasi muscle, ending as the angular artery. There is a percentage of 12.9% where the nasolabial trunk runs similarly to the first description of the nasolabial pattern. However, the infraorbital trunk is superficial to the zygomaticus major, zygomaticus minor, and levator labii superioris to the infraorbital area and area nasal (Type IIb). When referring to the forehead pattern, 16.7% is not covered by the facial muscles in the upper lip, lateral to the margin of the orbicularis oculi muscle in the nasolabial fold, and in the lateral area of the dorsum of the nose or angular region (Type IIIa). In a smaller percentage, 1.9%, in the forehead pattern, the trunk of the deep facial artery crosses the infraorbital area located next to the main trunk of the FA branches. This additional arterial trunk goes deep into the facial muscles. It joins the branches of the infraorbital artery to the lateral side of the nose (Type IIIb) (Figure 5).2
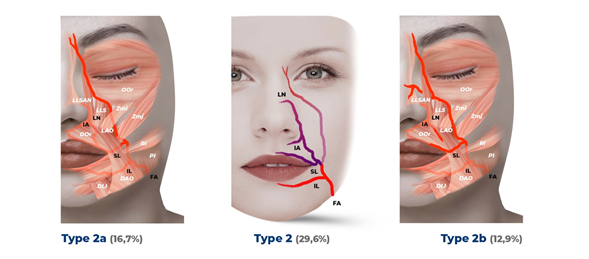
Figure 5.2 Type 2 nasolabial pattern and an infraorbital trunk and subtypes 2a and 2b, the purple and pink colors of the FA branches indicate the nasal and infraorbital trunks, respectively.
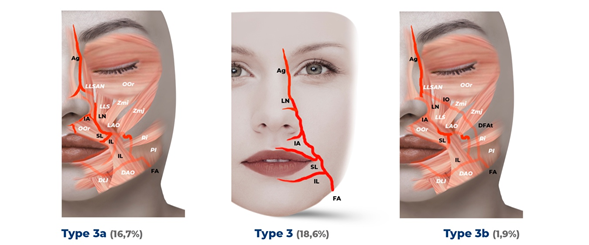
Figure 5.3 Type 3 forehead pattern and subtypes 3a and 3 b.
Facial artery(FA) concerning the layer of facial musculature - the color of the FA that runs below the facial muscles is lighter than that of its superficial path - that runs above the facial muscles. In addition, the exposed points of the FA not covered by facial muscles that are considered to be at risk of some injury are observed.
Branches of the FA: Ag, angular artery; DFAt, deep trunk of Fa; IA, inferior alar artery; IL, inferior labial artery; IO, infraorbital artery; LN, lateral nasal artery; and SL, superior labial artery.
Facial muscles: DAO, depressor of the angle of the mouth; DLI, lower lip depressor; LAO, levator anguli oris; LLS, levator lip superioris; LLSAN, levator labii superioris and alar nasi; OOc, orbicularis oculi; OR, orbicularis oris; pl, platysma; Ri, laughing; Zmi, zygomaticus minor; and Zmj, zygomaticus major.
Distribution of facial vessels in the skin
Arterial perforators give the irrigation of the skin of the face in the deep fascia from the main arteries. Unfortunately, few arterial perforators characterize the lateral area of the face. In contrast, hundreds of arterial perforators in the anterior zone provide vascularization of the anterior facial areas.17
The use of FA skin perforators in surgeries has made it possible to carry out surgical reconstructions that were previously carried out in 2 or 3 stages in just one procedure and provides better aesthetic results, even though, up to now, it is not possible to determine precisely the limits of the skin area irrigated by a perforator, most of them originate between 20 to 60 mm along with the Fa. An article identified a common origin to find the perforations, calling it "point A," which can be determined by drawing the Frankfort line, a line parallel to the plane through the angle of the mouth, and a perpendicular line through these two lines on the side edge. At an acute angle of 45º from the horizontal and at an average distance of 10mm from "point B" (Figure 6).18

Figure 6 By drawing Frankfort's horizontal line and a line parallel to it at the level of the angle of the mouth. A perpendicular line is drawn from the side edge to pass through these two lines. Point B represents the intersection of the parallel line passing through the angle of the mouth and the perpendicular. Point A represents the reference point to locate the area where the facial artery perforators most consistently originate.
On the other hand, it is described that FA perforators are found predominantly between 1 to 2 cm lateral to the level of the oral commissure and are classified into seven main types: posterior area of the horizontal ramus of the mandible, anterior area of the horizontal branch of the mandible, lower labial area, commissural area, and jugal area, which allow it to be a good option when talking about the design of a local flap, even allowing primary closure of the donor site and a hidden scar in a fold naturally.19
The external and internal carotid arteries generate a collateral blood supply through multiple anastomoses. The FA in its labial segment as the superior labial artery gives off small-caliber and superficial ascending branches that can travel superiorly to anastomose with the inferior alar, columellar, and anterior septal branches. Then, at the nasolabial fold level as the angular artery, the subcutaneous injection of filler in the nasolabial fold near the alar base can cause alar and cheek necrosis. One way of distribution for ocular embolism is through propagation in the artery angle and its anastomoses with the dorsal nasal branches.20 the thirteen branches of the ophthalmic artery, the central retinal artery, and the medial and lateral posterior ciliary arteries provide blood supply to the retina.6 This collateral blood supply can lead to visual compromise as a complication resulting from filler injection and obstruction of the ophthalmic artery or branch of the FA that anastomoses to the ophthalmic artery, limiting the blood supply to the central retinal artery, resulting in possible blindness. Information about the anastomosis pattern between the ophthalmic artery and the FA in the dorsum of the nose and the glabellar area is vital to prevent serious complications.4 The dorsal nasal artery is the bilateral terminal branch of the ophthalmic artery and anastomoses directly and indirectly with the supratrochlear, angular nasal, and supraorbital arteries. In addition to the dorsal nasal, supratrochlear, and angular arteries, the supraorbital artery sends branches that anastomose with the frontal branch of the superficial temporal artery at the junction of the middle and lower transverse thirds of the forehead (Figure 7).20

Figure 7 This schematic depicts a perforating angiosome (blue) bounded by constricting anastomotic vessels (arrows), which join adjacent perforators to form a continuous network. The area inside the bluish circle represents how the spasm of these strangulating arteries could limit the necrosis of this territory after the embolism in the main trunk of the perforator (blue dot and red arrow).
In the analysis of the anatomy and distribution of FA, a conceptual definition called angiosome emerges as a functional unit of an anastomotic throttling vessel around a perforating angiosome whose characteristic is the control or limitation of vascular flow to adjacent sites (Figure 8).

Figure 8 Diagram showing the functional angiosome with the pattern of necrosis that occurs at the interface of anastomotic vessels in flaps: (upper image) joined by strangulation vessels, (middle image) true anastomoses, where effectively, the first two territories are joined as a single one, (lower image) where the perforator has been affected with a toxin that has initiated the spasm of the surrounding strangulation vessels that connect with adjacent anastomotic territories.
Text with permission: Ashton MW, Taylor GI, Corlett RJ. The role of anastomotic vessels in controlling tissue viability and defining tissue necrosis with special reference to complications following injection of hyaluronic acid fillers. Plast Reconstr Surg. 2018;141(6):818e-830e.
Along with this, there are two types of anastomosis. Accurate anastomosis is one in which the vessels that join territories do not lose their caliber, and the anastomosis due to strangulation decreases its caliber (Figure 9). Are described in: (1) the glabella region of the forehead between the supraorbital and supratrochlear branches of the ophthalmic artery; (2) the nasal bridge between the terminal and lateral angular nasal branches of the facial artery and between the dorsal nasal branch and the ophthalmic artery; (3) at the nasal tip between the lateral nasal branches of the facial artery and a branch to the nasal columella from the superior labial artery; (4) across the upper and lower lip near the midline between the labial arteries; and (5) between the lateral branches of the facial artery as it runs through the nasolabial fold, connecting with small perforations that emerge from the cheek on the parotid gland and the masseter of the transverse branch of the superficial temporal and maxillary arteries.21 The latter has been shown to play an essential role in controlling the tissue viability, delaying blood flow to adjacent vascular territories when an intravascular injection of hyaluronic acid is accidentally produced, preventing it from traveling to adjacent territories. It is the primary determinant of the location and extent of tissue necrosis after inadvertent intra-arterial injection of hyaluronic acid.21

Figure 9 Schematic diagram showing the most frequently affected hyaluronic acid emboli sites (shaded purple) that coincide with choke anastomoses between branches of the facial and ophthalmic arteries. Text with permission: Ashton MW, Taylor GI, Corlett RJ. The role of anastomotic vessels in controlling tissue viability and defining tissue necrosis with special reference to complications following injection of hyaluronic acid fillers. Plast Reconstr Surg. 2018;141(6):818e-830e.
The facial artery muscle mucosal flap (FAMM) was first described in 1992 by Pribaz.22 It is widely used for head and neck reconstruction due to its versatility, minimal donor site morbidity, and ample arterial supply. Corresponds to a flap of the inner cheek made up of mucosa, submucosa, part of the buccinator muscle, facial artery, and the most profound plane of the orbicularis oris muscle that allows us to repair surgical defects in sites of the oral cavity, oropharynx, intranasal lining and orbit, as well as aid in the treatment of mandibular osteoradionecrosis.23 The facial nerve branches are found more profound than the FA, which conditions a lower risk of the VII nerve function. Rarely is the facial vein incorporated into the flap since venous drainage is possible through the buccal plexus found in the submucosa.24
A width of the flap between 2.5 and 3 cm is considered as it provides certainty of finding the FA centered along the flap; for this, it is crucial to delimit it correctly, knowing the anatomy and variables related to the FA, at the same time it can be reduced the risk using a Doppler ultrasound or by directly palpating the area.
The surgical technique is initially described respecting limits already defined in the literature; anteriorly, it is 1 cm posterior to the oral commissure; posteriorly, it is delimited by the orifice of the Stenon duct; inferiorly, the base of the flap is 2 to 3 cm long and is centered between the second and third molars, it continues the trajectory of the artery facial to the gingivolabial sulcus superiorly.25 The dissection begins 1 cm lateral to the oral commissure, sectioning mucosa, submucosa, and the buccinator muscle to identify FA or any branches. Generally, the superior labial artery is identified. First, the flap should be elevated with the layer below the FA, and the FA must remain attached to the adjacent tissues along its entire length23 followed proximally to identify the FA before ligation. The dissection is then deepened laterally to the FA, in the plane between the deep facial fascia and the oropharyngeal fascia along the entire vertical length of the flap24. If the inferior base flap of the facial vessels is considered when they enter the face through the anterior border of the masseter muscle, its vascularization is antegrade and the pivot point is located between the second or third molar. When the upper base flap is taken, its vascularization is retrograde through the angular artery, continuation of the FA; it can also be based on the superior labial branches and other anastomotic branches of the infraorbital vessels and its pivot is located at the level of the tuberosity.23,26
Other branches of the FA are functional when talking about flaps; one of them, the inferior labial artery - the main blood supply for the vermilion - is used in the vermilion crossed labial flap to treat congenital cleft lip defects or trauma minor in soft tissues. The location of the FA is an essential factor to consider when making the labial flap, the vertical distance between the inferior labial artery and the border of the vermilion. In most cases, the inferior labial artery is in the submucosa, and in a smaller percentage, it is found in the superficial muscular layer of the orbicularis oris. Another factor to consider when designing the flap is the vertical distance between the inferior labial artery and the midline epithelial surface of the lower lip of 2.42± 1.67 mm. A 1 cm incision from the corner of the mouth, a 4 mm deep dissection continuing towards the midline in the same plane to end 1 cm before the contralateral corner gives us a safety range at the time of design. Of flap;27 This anatomical knowledge added to the use of a Doppler ultrasound would provide preoperative security of the viability of the flap.
On the other hand, the nasolabial region where the superior labial artery is located is also considered an ideal donor area, given its abundant blood supply. The facial artery is approximately at 43º12 from the angle of the mouth and branches of 12 mm following a tortuous path between the mucosa and the orbicularis oris muscle, from 6.7 to 6.9 mm from the lower red border of the upper lip, generating anastomosis in the midline and giving 4 to 7 superficial septal branches and 2 to 4 deep ones in the upper lip.28 This area can be used advantageously given the excellent circulation, freedom of flap design, wide rotation arc, color, and texture to reconstruct other defects (Figure 10).29

Figure 10 Anatomy refers to the pedicled nasolabial flap from the superior labial artery. FA, facial artery; ILA, inferior labial artery; LNA, lateral nasal artery; OM, orbicularis oris muscle; RM, risorius muscle; SB, septal branches; SLA, superior labial artery; ZM, zygomaticus major muscle.
Over the years, the face undergoes numerous structural changes, generating signs of facial aging. As a result, many people are inclined to improve their appearance acquired over the years through minimally invasive procedures as an option to traditional plastic surgery. There are multiple alternatives when choosing the dermal filler to use, among which we find autologous fat, biodegradable dermal fillers (hyaluronic acid), and biodegradable collagen stimulators (calcium hydroxyapatite), poly-L-lactic acids (PLLA) and products non-biodegradable (polymethylmethacrylate and methylmethacrylate).
In recent years, the need to correct the inevitable effects of age at the facial level has given way to minimally invasive procedures, which have increased significantly, especially the injection of different types of dermal fillers, in 2017 it was generated an increase of 312% compared to the year 200020 and along with this also the increase in adverse effects involving FA and its branches, generating tissue necrosis, blindness, cerebrovascular accidents2,6,14,30 among others. The most severe complications described in filler (mainly Hyaluronic Acid) are necrosis and ophthalmic injuries due to intravascular injection or compression of the vessel; they are fundamentally based on the concepts of perforators, angiosomes, and anastomoses already analyzed in chapter B.
If we want to reduce the risks, a broad knowledge of the facial anatomy, its variants, and the type of product to be injected must be had. When entering the arterial circulation, the injection of dermal filler can be transported to vulnerable regions, causing severe problems for the patient. Therefore, it is essential to avoid intravascular injection, vascular injury, and compression; for this, we must take into account the anatomical variables that FA presents, risk areas, and general principles of a safe injection to maximize the safety of the procedure and minimize risks. One of the most severe adverse effects described in the literature is ophthalmic complications, such as blindness caused by the advancement of a filler through the facial artery to reach an anastomosis with the ophthalmic territory (central retinal artery), as well as necrosis and ischemia are complications that should also be considered, therefore following injection protocols such as the use of appropriate products and instruments, needles less than or equal to 27G, the use of cannulas, low G' dermal fillers in high G' areas. Risk, injection with low pressure and small increments20, aspiration, the experience, and knowledge of the operator, among others, minimize the risks of these procedures that generally have a low percentage of complications but from which no one is exempt.
As previously stated, FA presents significant anatomical variations in its tortuous path, especially when it is at the level of the oral commissure where it is exposed without being covered by facial muscles. Studies have shown the need to be sure of the anatomical pattern presented by FA to provide safety and less risk to the surgeon who will perform a particular procedure; for this, the use of in vivo and non-invasive techniques that reflect the patient's reality is required. For successful pre-surgical planning.
Computed tomography angiography is one of the current techniques for reconstructing vascular, bone, and surrounding soft tissue anatomy, considered less invasive and more efficient since the patient is exposed to less radiation than in magnetic resonance imaging.31 One study evaluated computed tomography angiography in the evaluation of anatomical variations of FA and its branches, classifying its anatomical variation into four types: Type 1, a short path that ends proximal to the superior labial artery (34%); Type 2, an intermediate course that ends distal to the superior labial artery near the nasolabial fold (40%); Type 3, a classic course that extends to the lateral nasal ala beyond the nasolabial fold with an angular branch (24%); and Type 4, angular branch duplicated as the main terminal branch of the facial artery (2%).32 Although, on the other hand, in cadaveric studies, it is observed in a higher percentage that FA ends its course in the angular artery,33 computed tomography angiography is limited for the detection of small-caliber arteries and can generate adverse effects due to the use of contrast media.32
Doppler ultrasound is a test that allows analysis of the facial vascularization pattern, even in its terminal branches. For example, one study analyzed FA by Doppler ultrasound at the base of the mandible in front of the masseter muscle, obtaining a mean diameter of 2.7mm;34 another using the same methodology had a mean diameter of 2.14mm.35 However, computed tomography found a mean diameter of 2.83mm;36 these variations may be due to the methods used. However, both tests play in favor of correct pre-surgical planning.
FA does not present a harmonic and symmetrical distribution throughout the face and, as we have established, this artery has a tortuous and irregular distribution.3 even it is not similar in the same individual; therefore, before performing a particular surgical and minimally invasive procedure, we must take these anatomical conditions into consideration and analysis.
Concerning the flaps, the preoperative study is essential, within which the use of different imaging techniques would allow greater security in the performance that the different flaps of the FA tributary territory may have. With the advent of minimally invasive procedures that patients choose to deal with the signs of aging that accompany age, we must be aware of acquiring technical skills coupled with detailed knowledge of the anatomy and path of FA and the types of anastomoses that may exist, thus avoiding complications and vascular iatrogeneses such as necrosis and blindness. Therefore, it is still of great importance to know the distribution, the perforators, the ramifications of the FA, as well as the actual or strangulation anastomoses that at some point may act as a functional element of "salvage" of an ischemic territory that is accidentally affected during a filler injection procedure.21
In recent years, the increase in minimally invasive facial procedures for aesthetic purposes has also accompanied different complications that can have devastating results. Therefore, detailed knowledge of the anatomy of FA, its anatomical relationships, distribution patterns, and types of anastomoses are fundamental in minimizing the risks of this type of iatrogenesis.
None.
None.

©2022 Constanza, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.