Journal of
eISSN: 2379-6359


Mini Review Volume 6 Issue 1
1School of Engineering Auckland University of Technology, New Zealand
2Department of Otolaryngology Head and Neck Surgery Counties Manukau District Health Board, New Zealand
3Department of Surgery University of Auckland, New Zealand
4Doug Makinson Development Ltd, New Zealand
Correspondence: David White School of Engineering Auckland University of Technology Private Bag 92006 Auckland 1142, New Zealand, Tel + 64 9 921 9999
Received: August 28, 2016 | Published: February 20, 2017
Citation: White DE, Shakeel M, Bartley J, Makinson D, Whittington C (2017) Custom 3-D Printed Nasal Mask for Measuring Nasal Airflow: A Cost Effective Method with Design Flexibility. J Otolaryngol ENT Res 6(1): 00150. DOI: 10.15406/joentr.2017.06.00150
The nasal cycle controls the balance between heat and water fluxes and enables cells and glands to rest and recharge. Nasal drying is reported frequently during nasal applied CPAP in sleep apnoea patients. There is no current mask system that allows continuous inter-nasal airflow measurement to be recorded during both ambient and pressurised breathing. However, we have developed such a mask system utilizing standard nasal pillows and mounting head-gear produced using 3-D printing. Inter-nasal airflow was detected and continuously logged for both ambient and pressurised conditions. This system detects airflow continuously over both inhalation and exhalation phases of breathing in human beings.
Keywords: nasal cycle, airflow sensor, 3-d printing, computer-aided-design, continuous positive airway pressure, nasal mask
The exact role of the human nasal cycle, where the patent naris carries the majority of nasal airflow when compared to the congested naris, is unknown. Researchers have previously confirmed the presence of the human nasal cycle in both awake and sleep states.1 Our computational nasal air-conditioning model has shown that during inhalation, the airway surface liquid becomes dehydrated in the patent nasal airway, while the congested nasal airway remains fully hydrated.2 This finding supports the current understanding that the nasal cycle controls the balance between heat and water fluxes and enables cells and glands to rest and recharge.3
Nasal drying, which is reported frequently during nasal applied CPAP (n-CPAP) use, is commonly overcome through the use of supplementary humidification,4 but the current published literature does not explain adequately the need for additional humidification. We have hypothesized that the nasal breathing of pressurised air disturbs the nasal cycle thus interfering with nasal humidification. Unfortunately, there is no current mask system that allows continuous inter-nasal airflow measurement to be recorded during both ambient and pressurised breathing. However, we have developed such a mask system and describe it here.
The mask design incorporated separate air conduits that acted as the central mask structure for the face mounting system. For convenience, the mask attachment and head gear were based on a readily available commercial mask (Fisher & Paykel Opus). For this first mask design iteration, priority was given to conducting both air supply tubes from the strapping system attached to the head. While this was intended to minimise tangling of the hoses during sleep studies it did obstruct the user’s clear view whilst awake (Figure 1). The main body of the mask also acted as the dual air conduits to each naris via nasal mask pillows (TAP PAP, Airway Management Ltd, USA). These pillows come in a range of sizes, which enable a good air seal to be achieved for a range of facial morphology. Embodiment of the new mask was created within a computer-aided-design (CAD) environment (SolidWorks, Dassault Systèmes, France) and 3-D printed in nylon composite at the Auckland University of Technology using a selective laser sintering (SLS) process (EOS model FORMIGA P100, Germany) (Figure 2).
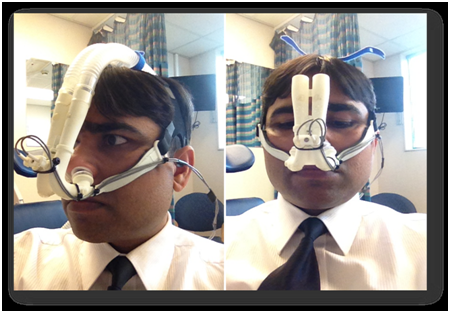
Figure 1 Compromise of allowing the mask to obstruct frontal vision to minimise the chance of the dual air supply hoses tangling during sleep studies. Image on left shows pressurised breathing, image on right shows ambient breathing.
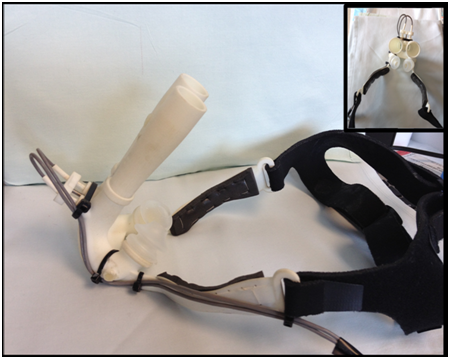
Figure 2 Custom nasal mask showing use of commercially available components of head-gear (Fisher & Paykel Opus) and nasal mask pillows (TAP PAP, Airway Management Ltd, USA).
For our investigations, relative airflow apportionment between each airway was assessed measuring air velocity within each of the two separate air conduits. This parameter was sensed using UAS1500XS series USB sensors (Degree°C, USA) which provided direct PC connection via a USB port. These sensors cover a wide measurement range varying from 0.15 to 20 m/s to 5% accuracy and were modified by the manufacturer to provide a minimum sample time of 20milliseconds. Each sensor was located between the nasal pillow and mask bias vents on the tightest straight section of the air conduit to minimise the effect of turbulence while directly reading airflow through each naris. Air velocity data from the UAS sensors was recorded every 20ms and displayed on a laptop PC (LabView, National Instruments, USA) in real time (Figure 3). Analysis of inter-nasal airflow partitioning results was undertaken using propriety software (MatLab, Mathworks, USA).
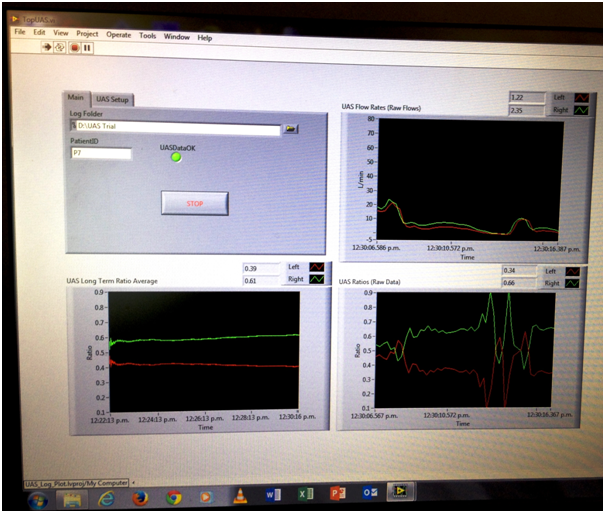
Figure 3 Screen shot of real time data collection. Data plots moving clockwise from upper right, instantaneous left and right airflow raw data, instantaneous airflow partitioning ratio and averaged airflow partitioning. Left and right airway channels are shown as red and green traces respectively.
Mask bias venting from each airway conduit was provided by a series of small holes to provide continual outflow of mask air. These holes were calibrated to pass air at a rate of 15 l/min from each side at a mask pressure of 4cm H2O to prevent excessive CO2 build-up occurring within the mask. This flow rate is the accepted minimum mask bias flow rate for a standard CPAP nasal mask having a common air space so there was no chance of CO2 build-up occurring in our new design.
A range of methods have been-used previously to measure the nasal cycle. These range from flow indication techniques based on a simple visual evaluation of condensation delivered during exhalation onto a crossed glass plane placed directly under the nares; airflow measurement using dual portable spirometers through to simultaneously measured peak exhaled nasal flow. Recently the ‘Rhino Cycle’ system has enabled continuous nasal airflow monitoring to be undertaken.1 Unfortunately all of these techniques are unable to measure inter-nasal airflow during pressurised breathing. The use of Image based analysis such as Acoustic Rhinometry, Rhinomanometry and Endoscopic evaluations are also not suited for this task. While magnetic resonanace imaging has previously been use, this is expensive so a more cost effective means was required. The closest inter-nasal measurement system we could find was a nasal mask with thermistors positioned near each naris.6 Unfortunately this system was limited to the relative indication of inter-nasal airflow during exhalation and to ambient pressure breathing. We desired a system where we could directly and continuously measure simultaneous nasal airflows for both inhalation and exhalation phases under both ambient and pressurised breathing conditions. We are happy for other researchers in this field to use our model.
None.
Authotr declares there are no conflicts of interest.
None.

©2017 White, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.