Journal of
eISSN: 2379-6359


Research Article Volume 16 Issue 3
Faculty of Medical Sciences of Santa Casa de São Paulo, São Paulo University, Brazil
Correspondence: Oscimar B Sofia, Faculty of Medical Sciences of Santa Casa de São Paulo, Department of Otorhinolaryngology, São Paulo University, Brazil
Received: August 01, 2024 | Published: September 17, 2024
Citation: Sofia OB, Dolci JEL, Dolci ELL. Costal cartilage graft for treatment of empty nose – a new technic. J Otolaryngol ENT Res. 2024;16(3):69‒72. DOI: 10.15406/joentr.2024.16.00553
The purpose of this study is to describe a technique for treatment of empty nose syndrome using costal cartilage and insert the graft through an oral approach. This review aims to discuss the proposed pathophysiology of Empty Nose Syndrome (ENS), evaluate the role of validated diagnostic tools in its diagnosis, and review medical and surgical treatment strategies for affected patients. Recent findings suggest that aside from a reduction in nasal turbinate size, impaired trigeminal nerve function may also contribute to the pathophysiology of ENS.
Keywords: Empty nose syndrome, inferior turbinate reconstruction, cartilage costal graft technic.
Across-sectional study examining the relationship between Empty Nose Syndrome (ENS) and mental health, as well as functional impairments. Fifty-three individuals with ENS participated, recruited from online forums. Participants completed various validated questionnaires assessing depression, anxiety, daytime somnolence, work productivity, impairment in daily activities, and general health state. Results indicate that individuals with ENS reported moderate to severe levels of anxiety and depression. The severity of ENS is correlated with severe depression, anxiety and impaiment in daily activities.1 This review aims to discuss the proposed pathophysiology of Empty Nose Syndrome (ENS), evaluate the role of validated diagnostic tools in its diagnosis, and review medical and surgical treatment strategies for affected patients. Recent findings suggest that aside from a reduction in nasal turbinate size, impaired trigeminal nerve function may also contribute to the pathophysiology of ENS. While injectable implants for turbinate volume augmentation show promise, more data are needed to fully support their use advocate for the cautious integration of these screening tools into clinical decision-making processes.2
This review aims to discuss the pathophysiology of Empty Nose Syndrome (ENS), evaluate validated diagnostic tools for its diagnosis, and review medical and surgical treatment strategies. Preventing iatrogenic ENS through careful avoidance of excessive turbinate reduction is crucial to preventing paradoxical nasal obstruction. Initial treatment approaches include nasal humidification, patient education, and addressing concomitant medical conditions such as depression.3
This article addresses the management of patients with persistent nasal obstruction despite attempted treatment strategies, focusing on a sensitive approach considering the patient's mental health. While diagnostic testing is often unnecessary, endoscopy and imaging may be warranted in some cases. Validated patient-reported outcome measures offer objective assessment of symptoms. Medications can either exacerbate or alleviate symptoms, and various surgical interventions, while effective in some cases, can lead to functional impairment. Conditions such nasal valve stenosis, septal perforations, and empty nose syndrome are discussed.4 This abstract highlights Empty Nose Syndrome (ENS), a contentious condition characterized by disrupted nasal airflow due to excessive loss of turbinate tissue, typically occurring after total or near-total inferior turbinate resection. Diagnostic tools include a validated patient questionnaire and the office cotton test. Treatment encompasses topical moisturization, behavioral/psychiatric assessment, and surgical reconstruction. Prevention of postprocedural ENS is paramount, emphasizing the minimization of inferior and middle turbinate tissue loss.5 This prospective observational study aimed to investigate the association between dyspnea in patients with Empty Nose Syndrome (ENS) following turbinate surgery and Hyperventilation Syndrome (HVS). The study hypothesized that lower airway symptoms in ENS might be explained by HVS. Patients with HVS completed the Sinonasal Outcome Test (SNOT)-16 questionnaire before and after an eight-session respiratory rehabilitation program. This study suggests that HVS is frequent in patients with ENS, and that symptoms can be improved by respiratory rehabilitation. Pathophysiological links between ENS and HVS deserve to be further explored.6
Fifteen patients diagnosed with ENS and 18 controls with non-ENS sinonasal conditions underwent office cotton placement. Both groups completed ENS6Q testing in three conditions: precotton, cotton in situ, and postcotton, to measure reproducibility of ENS6Q scoring. Participants also rated subjective changes in nasal breathing with and without cotton placement using a transition scale. In conclusion, cotton testing is validated for assessing ENS patients in the office setting.7
Three groups were compared:
The study concludes that ENS patient’s exhibit significantly impaired intranasal trigeminal function compared to ITR patients and controls. Further prospective studies are warranted to explore the role of preoperative trigeminal function in these patients and the impact of surgery on this impairment.8 Questionnaire (ENS6Q) as an adjunct to the standard Sino-Nasal Outcome Test 22 (SNOT-22) questionnaire to better identify patients suspected of having Empty Nose Syndrome (ENS), an acquired condition challenging to diagnose objectively. In conclusion, ENS6Q is the first validated, specific adjunct to the SNOT-22 questionnaire, offering a more reliable tool to identify patients suspected of having ENS.9 This prospective cohort study conducted in a tertiary medical center aimed to evaluate changes in depression and anxiety before and after surgical treatment for Empty Nose Syndrome (ENS), as psychological symptoms are often associated with ENS, yet psychiatric instruments are underutilized in current literature. In conclusion, depression and anxiety are prevalent among ENS patients, and surgical treatment is effective in improving these psychological disorders.10
Compare the clinical benefits and improvements in quality of life between lateral nasal wall implantation and inferior nasal wall implantation in patients with empty nose syndrome (ENS) who underwent endonasal submucosal implantation. Patients were divided into lateral and inferior nasal wall groups. The SinoNasal Outcome Test (SNOT)-22, Beck Depression Inventory (BDI)-II, and Beck Anxiety Inventory (BAI) were assessed before and 1 year after implantation. In conclusion, lateral nasal wall implantation may offer significantly better clinical outcomes than inferior nasal wall implantation, suggesting it may be the preferred site for implant placement in ENS patients.11 This review aimed to evaluate the outcomes of surgical intervention for empty nose syndrome (ENS) by analyzing data from various sources including the fillers, foreign material and autologous material. And the approach can be endonasal or transoral. We concluded that, surgical intervention for ENS shows promise in improving clinical outcomes, although not all patients derive benefit. Long-term follow-up using both subjective (SNOT-25) and objective (rhinomanometry) measures of clinical outcome is recommended.12 In this study, the efficacy of submucosal injection in patientes that underwent submucosal injection of carboxymethylcellulose/glycerin gel (Prolaryn®) resorbable filler, Hialronic acid (HÁ) into the inferior meatus for the treatment of Empty Nose Syndrome (ENS) was evaluated. Fourteen patients underwent injections, and results showed significant improvements in ENS symptoms, as evidenced by decreased ENS6Q scores at 1 week post-injection, with sustained reduction at 1 month. The study concludes that transient, focal airway bulking via submucosal filler injection at sites of inferior turbinate tissue loss can markedly benefit ENS patients, suggesting that aberrant nasal aerodynamics from inferior turbinate tissue loss may contribute to (potentially reversible) ENS symptoms.13
This study aimed to assess the efficacy of intranasal injection of submucosal implantation of hyaluronic acid (HA) gel. Following treatment, the patients experienced symptom improvement for several months, with no recorded complications. The study concludes that intranasal injection of HA gel appears to be a simple, safe, and moderately effective treatment option for less severe forms of ENS due to its temporary clinical effects.14 The objective of this study was to conduct a prospective randomized blind clinical study comparing the efficacy and safety of using acellular dermal (alloderm) grafts versus silastic sheets submucosal implants for managing empty nose syndrome (ENS). A total of 24 patients diagnosed with ENS were randomly assigned to two equal groups: the silastic implant group and the alloderm implant group, based on the type of implant used to reconstruct the nose. These implants were inserted into submucoperichondrial and/or submucoperiosteal pockets created along the septum, nasal floor, and lateral nasal wall. Both graft materials proved suitable for the procedure, with no statistically significant differences between them. Patients in both groups exhibited marked subjective and objective improvements, indicating the safety and relative simplicity of the surgical procedure.15 Patients with empty nose syndrome (ENS) often experience significant discomfort in their daily lives, posing challenges for physicians in managing their condition. This study aimed to evaluate the outcomes of ENS treatment via reconstruction of the inferior turbinate using porous polyethylene (Medpor). Over a follow-up period ranging from 3 to 18 months, all patients reported subjective improvements in symptoms, and a statistically significant improvement in SNOT-20 scores was observed (P<0.05). Acoustic rhinometry assessments demonstrated postoperative improvements in nasal resistance, nasal volume, and minimum cross-sectional area, with a significant overall average score (P<0.05). Reconstruction of the inferior turbinate with Medpor represents a promising new approach for treating patients with empty nose syndrome.16
Empty nose syndrome (ENS) is a rare complication that can occur following turbinate surgery, characterized by paradoxical nasal obstruction, nasal dryness and crusting, and a persistent sensation of dyspnea. Medical treatment options for ENS include measures to humidify the nasal mucosa, such as saline irrigations and emollients. Surgical intervention is typically reserved for cases that do not respond to conservative therapies and may involve turbinate reconstruction using implantable biomaterials. Preventing ENS is crucial, and surgeons should employ techniques that preserve as much turbinate tissue as possible during nasal surgery to minimize the risk of this debilitating condition.17 The article proposes a novel method for reconstructing a completely resected inferior turbinate using hydroxyapatite cement in patients experiencing symptoms commonly associated with an excessive resection of the turbinate, often referred to as "empty nose syndrome" (ENS). Hydroxyapatite cement, a biocompatible material commonly used in orthopedic and dental applications, is suggested as a promising option for turbinate reconstruction. The proposed method offers potential advantages such as durability, biocompatibility, and ease of application.18 This study aimed to assess the impact of surgery and various implant materials on subjective outcomes in patients diagnosed with empty nose syndrome (ENS). A meta-analysis was conducted to evaluate postsurgical outcomes in patients with ENS who received treatment involving different types of implants. A comprehensive search identified 122 relevant studies, from which 6 were selected for inclusion in the meta-analysis. This meta-analysis suggests that surgical intervention can lead to improvements in symptoms and SNOT scores among patients with ENS. Additionally, autografts/allografts appear to be more effective than foreign material grafts in managing ENS symptoms.19
In this study, we propose a novel surgical technique for managing ENS by utilizing autologous auricular cartilage to augment the turbinate and restore natural airflow patterns within the nasal cavity. This innovative approach offers several potential advantages, including the use of the patient's own tissue, which reduces the risk of rejection or implant-related complications. If proven effective, the use of autologous auricular cartilage for turbinate augmentation could represent a valuable treatment option for individuals suffering from this challenging condition.20 This study aimed to assess the efficacy of endonasal microplasty in treating empty nose syndrome (ENS) by comparing the outcomes of using costal and conchal cartilage implants to construct neoturbinates. Both groups demonstrated a significant improvement in SNOT-25 scores postoperatively (P < .05). However, the group receiving costal cartilage implants showed a more significant improvement compared to the conchal cartilage group, as evidenced by the mean difference between pre- and postoperative SNOT-25 scores (P = .023). Costal cartilage appears to be more effective than conchal cartilage as implants for treating patients with empty nose syndrome.21 There is any study that show the use of costal cartilage trough an oral approach for the treatment of the ENS. Therefore, the aim of this case is to describe a technique that can be used safely and effective for that purpose.
This case describes a technique of insertion of costal cartilage graft through an incision in the deep of sulcus gingiva and lip superior at the level of pyriform aperture, detachment of mucoperiosteal and building a pocket that where will be inserted the graft. After diagnosed the ENS, clinically and using the 6-item questionnaire (ENS6Q), a CT is necessary for planning the surgery, where we can observe a total inferior nasal turbinate removed Figure 1.
After got the costal cartilage through an incision at the lever of 7 arch costal, the graft is shaped like a projectile. Figure 2A and Figure 2B.

Figure 2A The cartilage costal graft before shaped for introduction in the pocket by an oral approach.

Figure 2B Sutured incision at the level of seventh costal cartilage on right hemi-thorax were get the costal graft.
After shaped, the graft is inserted behind the pyriform aperture. Figure 3, 4, 5.
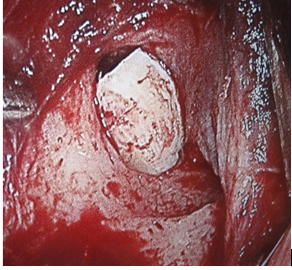
Figure 3 Close of operative view of implants placed along the lateral nasal wall just behind the piriform aperture and under the periosteum of the nasal mucosa.
Numerous procedures have been described to treat empty nose syndrome (ENS). Their objectives are to rebuild the inferior turbinate and to restore normal airflow pattern by diminishing the empty space within the nasal cavity by submucosal implantation of autograft or synthetic material. We describe a method using an oral approach and implants of costal cartilage graft. We believe that this new approach decreases the complications like infections, extrusion, reabsorption, pain or others. Implantation of costal cartilage graft can repair the damage of total inferior turbinate removed, with great success and small complications.12,19 The oral approach prevents the trauma in the atrophic nasal mucosa and consequent complications like infection and reabsorption or extrusion of the graft.14 The ideal material for nasal augmentation should have low extrusion and rejection rates, a minimal infection risk, and provide sufficient endurable structures.12
This technique shows implantation of autologous costal cartilage graft by a new approach. We agree that autologous graft is better,12,19 and by an approach, inserted the graft through an incision in the deep of sulcus gingivolabial, detachment the mucoperiosteum on the floor and lateral wall of nasal cavity at the level of pyriform aperture, and insert the costal cartilage graft.12 This will minimize symptoms and get better quality of life in patients suffering from ENS. This new technique offers an efficient material with a low complication rate in this procedure because the insertion by oral cavity permit keep the atrophic nasal mucosa intact, with less risk of extrusion.
None.
The author declares that there is no conflict of interest to disclose.

©2024 Sofia, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.