Journal of
eISSN: 2379-6359


Case Report Volume 17 Issue 1
Department of Otolaryngology, Ridgeview Medical Center, USA
Correspondence: Michael T Hopfenspirger, Ridgeview Medical Center, 560 South Maple Street, Suite 40, Waconia, MN, USA, Tel 952 4422191
Received: February 07, 2025 | Published: March 14, 2025
Citation: Hopfenspirger MT. Conservative management of an adult with multiple mandible fractures. J Otolaryngol ENT Res. 2025;17(1):22-23. DOI: 10.15406/joentr.2025.17.00559
Various approaches have been supported in the treatment of mandible fractures. Variables including number and location of fractures, patient age, status of dentition, overall health and socioeconomic factors may be used to aid in selecting the most appropriate treatment. In adults, multi-fracture cases are typically treated surgically with any combination of maxillomandibular dental fixation and rigid internal fixation. A case is presented here wherein a select patient with multiple mandible fractures was treated with observation alone. Her fractures and treatment course are described along with a brief discussion of the available treatment alternatives and how this option compares.
Keywords: mandible, fracture, treatment, fixation, conservative management
MMF; maxilla mandibular fixation, ORIF; open reduction internal fixation, ROM; range of motion
Traumatic fractures of the mandible are a relatively common injury treated by otolaryngologists. Given the number of variables that can be involved in these cases, the treatment approaches vary. Moreover, even among cases with reasonably similar details, literature can be cited to support significantly different approaches. This treatment landscape can be both beneficial, as resources may vary depending upon location and availability, and confounding, in that both surgeons and patients seek the ‘best’ solution. The standard of care for treatment of a case with multiple mandible fractures involves either maxillomandibular fixation (MMF) and/or open reduction with rigid internal fixation (ORIF). A variety of different approaches involving these techniques can be employed and result in equally and reliably good outcomes. However, there are disadvantages to all of these approaches necessitating an honest, complete informed consent process with patients. Among the disadvantages are risks associated with surgical complications, significant costs of treatment, and time away from work or other important activities. Presented here is a case of a young adult woman who suffered multiple mandible fractures and yet elected for observation only. Her course is outlined here and followed by a brief discussion of the implications of her experience.
A healthy, non-smoking, 22-year-old woman presented to the emergency department after suffering a fall from her bicycle. She was helmeted and denied any loss of consciousness or neck symptoms. Lower lip and chin lacerations were evident and she reported that her bite did not align. A noncontrast maxillofacial CT was obtained and showed a minimally displaced fracture of the right mandibular body and a minimally displaced fracture of the left mandibular condyle (Figures 1 & 2). Her soft tissues injuries were repaired and she was referred to the otolaryngology clinic for management of her fractures. Two days following the injury, the patient was evaluated in the clinic. She reported pain throughout the mandible in addition to trismus and mild malocclusion. The fractures were discussed and surgical treatment with ORIF and MMF was advised. An informed consent discussion occurred in which the risks and benefits of both the recommended treatment and no treatment were made clear. The patient expressed reasonable reservations about the surgery and opted for non-surgical management only. She was warned of the risks of non-union, malunion, and a potentially prolonged recovery period. Given her choice, she was strongly advised to visit the clinic on a weekly basis, adhere to a slowly progressing diet, and otherwise rest her jaw. The patient presented as mature and reliable and agreed to the plan.

Figure 1 Non-contrast CT. Left to right, top to bottom; coronal, sagittal, and transverse views of the right mandibular body fracture.
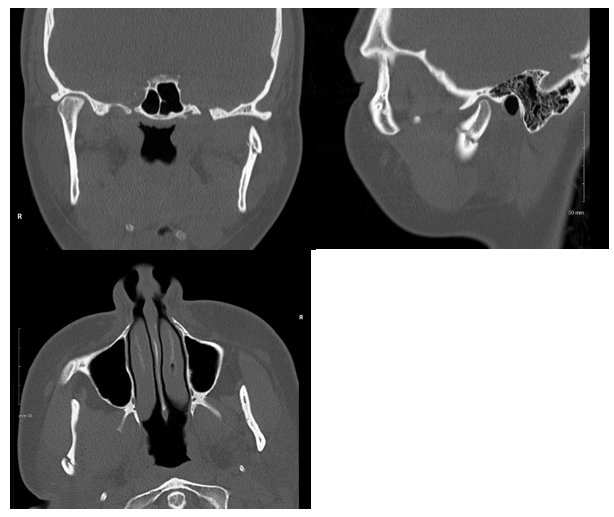
Figure 2 Non-contrast CT. Left to right, top to bottom; coronal, sagittal, and transverse views of the left mandibular condylar fracture.
One week later, the patient returned for follow-up. She reported improving pain (now only 3 out of 10), a reduced area of pain, and now normal dental alignment. She had been adhering to a pureed diet. No changes to her management were advised and she was to follow-up in one more week.
Two weeks after the injury, the patient was seen again. She reported pain (1-2 out of 10) only when supine and had stopped using any pain medications. Her occlusion remained normal. At this point, she was advised to begin daily range of motion (ROM) exercises and to progress to a soft diet. Three weeks after the injury, the patient was again evaluated. She reported minimal pain and normal occlusion. She had been performing and tolerating ROM exercises. She was encouraged to slowly increase the complexity of her diet and, given the quality of her response, asked to return in two weeks. At five weeks since the injury, the patient was last seen in the office. She reported no new symptoms and normal occlusion. She was tolerating a normal diet and had normal ROM. She was asked to follow-up on an as-needed basis at this point and was not seen again.
Fractures of the mandible vary widely in location, fracture number, complexity (comminution, favorability status), and overall severity. Other factors, such as bone quality, status of dentition and overall health, age, resource availability and surgeon preference may also be relevant and combinations of these variables result in a variety of management approaches. The preferred treatment approach to a case with multiple mandible fractures is surgical (to include interdental fixation), resulting in predictable and favorable outcomes.1 In many published reports, the term ‘conservative management’ often includes the use of interdental fixation. For the purposes of an appropriately contextualized discussion of this case report with relevant literature, this characterization becomes problematic. Application of interdental wires and appliances, which often includes some element of bone manipulation and reduction, is routinely done under anesthesia. A good argument can thus be made that treatment approaches short of this are more appropriately labeled as, “conservative.” Secondly, published reports on the subject of conservative management of mandible fractures may involve patients with single and simple, rather than multiple fractures. Observation-only therapy for those with simple, non-displaced fractures of the mandibular condyle, for example, is a well-established approach. This case report is importantly different in these ways.
Nondisplaced bone fractures, in otherwise healthy individuals, will heal if forces antagonistic to the stable approximation are minimized (for example, interdental elastics) or removed (rigid fixation). Indeed, this is the principle of most surgical approaches: the reduction of fractures (if necessary) followed by a mechanism to greatly reduce, or virtually eliminate, movement of the closely approximated segments. Given the function of the mandible, this environment would be unlikely to exist without such interventions. However, it is not altogether impossible. Nondisplaced (or even minimally displaced) fractures are, by definition, sufficiently reduced. The degree to which antagonistic forces can be minimized is the variable for consideration. In most cases, there is little reason to avoid controlling this with the standard approaches mentioned above. In this case, a mature and self-motivated adult chose to attempt a completely non-surgical route after considering all options and achieved a successful outcome. Several groups of authors have published on the subject of conservative management of mandible fractures. Rashid, et al, completed a systematic review and meta-analysis of outcomes in cases of non-surgical management.2
However, their analysis specifically excluded patients with condyle fractures. The vast majority of cases analyzed involved solitary fractures, with only two (of 80) involving multiple fractures. Arya, et al, published their experience with conservative treatment of 34 patients.3 This series also excluded cases involving condylar fractures and, importantly, all patients had solitary fractures. Finally, Cooney, at al, reported on their review of a series of pediatric patients who were treated conservatively.4 The comparison of this group’s experience is also questionable beyond the age demographic given that here, ‘non-surgical’ management did include at least some period of interdental fixation for about half of the patients (many of whom did have more than one fracture). A common theme throughout these studies was the overall favorable outcome of these more conservative approaches. That said, this case report differs significantly from these data given the additional complexity of the second fracture and the lack of any intervention at all (even brief MMF).
None.
The author declare that there are no conflicts of interest.

©2025 Hopfenspirger. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.