Journal of
eISSN: 2379-6359


Research Article Volume 10 Issue 3
1ENT Center (COF), Professor Edmundo Vasconcelos Hospital (CHPEV), Brazil
2Department of Otorhinolaryngology & Head and Neck Surgery, Federal University of São Paulo (UNIFESP)–São PauloSP, Brazil
Correspondence: Joao Mangussi Gomes, Department of Otorhinolaryngology & Head and Neck Surgery, 5237 Fifth Avenue, Apt C-2, Pittsburgh-PA, USA, Zip 15232, Brazil, Tel +1 412 482 2170
Received: December 27, 2017 | Published: May 1, 2018
Citation: Ximendes RC, Mangussi-Gomes J, Balieiro FO, et al. Anatomical relations between the frontal sinus drainage pathway and the agger nasi cell. J Otolaryngol ENT Res. 2018;10(3):118-121. DOI: 10.15406/joentr.2018.10.00326
Introduction: The anatomy of the frontal sinus drainage pathway is extremely variable. The definition of its relations to the agger nasi cell (ANC) greatly facilitates its understanding and, therefore, the planning of surgical approaches to this paranasal sinus. The main objective of this study was to evaluate the endoscopic anatomy of the frontal sinus drainage pathway in human cadavers, having the ANC as the main anatomical landmark.
Methods: A descriptive cross-sectional study was carried out, based on the endoscopic dissection of fresh human cadavers performed from April to November 2015. Thirteen cadavers were dissected and analyzed (total of 26 nasal cavities). The procedure began with the external trephination of each frontal sinus. After initial endoscopic dissection and identification of the ANC, 0.5% methylene blue was injected through the external trephine. Its drainage was endoscopically observed in relation to the ANC.
Results: Of the dissected cadavers, 9 (69.2%) were males and 4 (30.7%) females. The mean age (± SD) was 65 (± 12.3) years. The presence of 22 frontal sinuses was verified through the external trephination method (84.6%). The ANC was present in 23 nasal cavities (88.4%). The frontal sinus drainage pathways were evaluated in 20 sides (76.9%). In 6 of them (30.0%), the dye drained medial to the ANC; in 5 (25.0%), drainage was posterior; and in the remaining 9 (45.0%), posteromedial.
Conclusion: The frontal sinus drainage can preferably occur through 3 different ways (with respective frequencies): medial (30.0%), posterior (25.0%) and posteromedial (45.0%) to the ANC.
Keywords: frontal sinus, frontal sinusitis, endoscopy, endoscopic surgical procedures, dissection
Functional Endoscopic Sinus Surgery (FESS) is considered the treatment of choice for cases of chronic rhinosinusitis (CRS) refractory to clinical treatment.1 However, the surgical approach to the frontal sinus still represents a major challenge, even for the more experienced otorhinolaryngologist. Being unfamiliar with the anatomy of the frontal recess and all its possible variations can often result in inadequate treatment of the disease or even severe complications, such as orbital, vascular and skull base injuries.2–4
The frontal recess is the space through which the frontal sinus drains.5 It is limited laterally by the orbit (lamina papyracea) and lacrimal bone. Its posterior wall consists of the skull base bone. Anteriorly, the recess is limited by the agger nasi cell (ANC) and the frontal beak. Its medial limit is represented by the vertical lamella of the middle turbinate and the lateral lamella of the cribriform plate.2,6 Despite all these artificially fixed limits, the anatomy of the frontal recess is highly variable. The frontal drainage pathway is surrounded and influenced by the presence or absence and degree of penumatization of various cells and lamellas – ethmoid bulla, supra-bullar, fronto-bullar, supra-orbital, fronto-ethmoidal cells, and the ANC itself.7
The ANC is defined as the most anterior ethmoid cell. Defining the anatomical relations between the frontal sinus drainage pathways and the ANC greatly facilitates the understanding of its anatomy and thus, the planning of surgical approaches to the frontal sinus.8,9 We propose that this drainage can basically described as occuring in three different manners: 1) medial to the ANC; 2) posterior to the ANC; and 3) posteromedial to the ANC. The frequencies of these types of drainage, however, have not been fully explored in the literature.10 The pivotal objective of the present study was to evaluate the endoscopic anatomy of the frontal sinus drainage pathway, having the ANC as the main anatomical landmark.
Study design
A descriptive, cross-sectional study was carried out based on the endoscopic dissection of fresh human cadavers, from April to November 2015. Thirteen cadavers (26 nasal cavities) were dissected and analyzed. Cadavers with the following exclusion criteria were not considered for final analysis: age less than 18 years and/or the presence of sinonasal diseases that could interfere with the dissection and data interpretation (nasal polyps, signs of acute and/or chronic rhinosinusitis, and tumors, for example).
Before starting the endoscopic dissection, external trephination of the frontal sinus was performed bilaterally. After doing a bicoronal incision, the scalp was dissected from the anterior cranial region until the superior orbital rims, the glabella and the nasion (nasofrontal suture) were completely exposed. The trephination of each frontal sinus was performed separately, approximately 1 cm from the midline, just above the orbital rim, similar to the method described by other authors.11,12 For that purpose, high-speed electric drills (30-50,000 rpm) with 2 to 3-mm cutting burrs were used. The external opening of the frontal sinus was confirmed with the aid of a frontal ostium seeker or a delicate ball-tipped surgical probe. For those cases in which the presence of the frontal sinus was not verified after this procedure the sinus was considered absent or underdeveloped.
The material used for the sinonasal endoscopic dissection included: 4-mm, 0° and 45° Karl Storz® Hopkins II rod-lens endoscopes; XOMED® Digistar Plus camera; 14-inch SONY® HR Trinitron monitor; COMLUX® 150W halogen light source; and NEOMED® fiber optic cable. During all dissection sessions, two same doctors were always present (an otorhinolaryngologist specialized in Rhinology, and a 2nd-year ENT-resident).
The cadavers were placed in the supine position with the neck slightly extended and the head slightly turned to the surgeon's side (right side). The dissection procedure involved the following steps:
Video 1: Methylene Blue Drainage
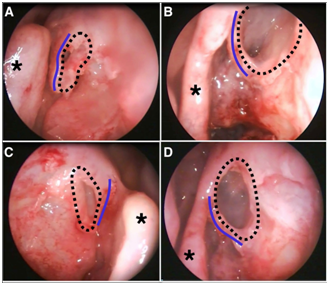
Figure 1 Endoscopic views of four different nasal cavities (A, B and D: left side; C: right side). Pictures were taken with 45º endoscopes, after adequate uncinectomy and immediately before injecting 0.5% methylene blue through external frontal sinus trephination. Key anatomical structures can be clearly visualized: dotted lines delineate agger nasi cells; middle turbinates are indicated by black asterisks; blue lines indicate vertical bars, which correspond to the superior attachment of the uncinated process to the medial wall of the agger nasi cell.
Data analysis
The data were tabulated using the Microsoft Excel software spreadsheet, v. 2010. A descriptive analysis of the data was performed, using mean and frequency measures.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee (No. 07/2015) and with the 1964 Helsinki declaration and its later amendments.
A total of 13 cadavers (26 nasal cavities) were dissected and analyzed. Of these, 9 (69.2%) were male and 4 (30.8%) female. The mean age (± SD) of the cadavers was 65 (± 12.3) years. The maximum age was 81 years and the minimum was 38 years. The demographic characteristics of the cadavers included in the study can be seen in Table 1. The distribution of cadavers regarding the different ethnicities can be appreciated in Table 2.
|
Male |
Female |
Total |
Number of cadavers (%) |
9 (69.2%) |
4 (30.7%) |
13 (100%) |
Mean age (years ± SD) |
63 ± 14.2 |
69 ± 4.5 |
65 ± 12.3 |
Table 1 Demographic characteristics of the cadavers included in the study (n=13)
Ethnicity |
Black |
Caucasian |
Mixed race |
Native Brazilian |
Asian |
Number of cadavers (%) |
1 (7.6%) |
5 (38.4%) |
5 (38.4%) |
1 (7.6%) |
1 (7.6%) |
Table 2 Ethnical distribution of the cadavers (n=13)
For all assessed cadavers, 22 frontal sinuses were identified through the external trephination method (84.6%). In 2 cadavers (15.4%), external trephination procedure was negative bilaterally. In such cases, frontal sinuses were considered absent or underdeveloped.
The ANC was identified in 23 nasal cavities (88.4%) and it was considered missing or underdeveloped in 3 (11.6%) cases. The frontal sinus drainage pathways could be evaluated through external trephination and dye injection in 20 nasal cavities (76.9%). All drainage pathways analyzed were pervious to the dye.
In 6 (23.1%) nasal cavities, it was not possible to assess the anatomical relations between the frontal sinus drainage pathway and the ANC, either due to absence/underdevelopment of the frontal sinus (3 nasal sides), absence of the ANC (2 nasal sides), or both (one nasal side).
Of the 20 (76.9%) nasal cavities that were assessed, methylene blue drainage was posterior to the ANC in 5 cavities (25.0%), medial to the ANC in 6 cavities (30.0%), and posteromedial to the ANC in 9 sides (45.0%). These frequencies are summarized in Figure 2.
The frontal sinus has the most complex and variable drainage pathway of all the paranasal sinuses. In the present study, we determined the relations of the frontal sinus drainage pathways with the ANC, which is the key to understanding the anatomy of the frontal recess.8,9
The prevalence of the ANC, defined as the most anterior ethmoidal cell on the lateral wall of the nasal cavity, shows great variability in the literature. Studies dating from the early twentieth century reported the presence of this cell in about 60% of the cases.6 In 1939, Van Alyea found this cell in 89% of the cases he studied.13 Later, Kuhn et al. demonstrated the presence of the ANC in 98% of their sample.14 Orhan et al.,15 in turn, found a prevalence of the ANC of about 40% in their population.15 In the present study, the ANC was verified in 88.4% of the assessed nasal cavities. Different results between studies corroborate the fact that important anatomical variations occur for this anatomical region and may also vary between different populations. Besides that, different studies often use different methods to assess the presence or absence of the ANC, such as imaging techniques or cadaver dissection studies. This also accounts for differences in anatomical prevalence.13,16,17 The reasons why the ANC is absent in some cases remain unexplained. In spite of that, it is observed that this happens in the less well-pneumatized nasal cavities.13,16
The frontal sinus could not be assessed through external trephination methods in 15.4% of the cases in the present study (bilaterally, in 2 cadavers out of 13). As well as the ANC, the frontal sinus and its drainage pathways present high anatomical and dimension variability. Descriptions of sinus aplasia and hypoplasia are not rare in the literature. The frequency of bilateral frontal sinus absence, for example, can vary from 3.4% to 10%.18–21 Unilateral sinus aplasia, for its turn, can be observed in 0.8% to 11% of all individuals.6,21 Gulisano et al., 22 conducted an anatomic-radiological study and detected the frontal sinus to be absent in up to 16% of the cases, which is closer to the numbers found in the present study. However, it is quite reasonable to think that the external approaches to the frontal sinus might underestimate the presence of this paranasal sinus when compared to other methods, such as imaging techniques.18,20
The location, dimensions, and degree of pneumatization of the ANC greatly determines the shape, size and diameter of the frontal recess. When the ANC is broadly pneumatized in the latero-lateral direction, it dislocates the vertical bar medially, so that this structure is next to the vertical lamella of the middle turbinate–in this anatomical condition the frontal sinus drainage pathway is posterior to the ANC. For the nasal cavities assessed in this study, the frontal recess was identified to be posterior to the ANC in 25.0% of the cases. Similarly, Thanaviratananich et al. described the frontal sinus drainage pathway as posterior to the ANC in 22.5% of their sample.10
The ANC can also be moderately pneumatized, so there is still space left between the vertical bar and the middle turbinate. In this case, the frontal sinus drainage can occur medially to the ANC. In the studied sample, this conformation was identified in 30.0% of the cases, which is similar to the frequency observed by other authors.10
A third type of frontal sinus drainage pathway was observed in this study. In 45.0% of the nasal cavities, the drainage was shown to be posteromedial to the ANC. It was observed that, in these cases, the ANC had no direct contact with the ethmoid bulla and not even with the middle turbinate, so there was space for the drainage to be posterior and medial to the ANC.
One of the factors that contributes to the success of the frontal sinus surgery is undoubtedly the complete understanding of the anatomy of the frontal recess. This is a complex area with a wide variety of anatomical configurations. The detailed study of the frontal sinus drainage pathways aids in the identification of the frontal recess and the frontal sinus, particularly in situations where the regional anatomy is distorted, as in the presence of diseases. Knowing the most common types of variations helps to correctly identify the drainage pathways, facilitating the surgical procedure. When doubts persist, the frontal sinus trephination can be performed intraoperatively.11,12
This study presents some limitations and disadvantages, being the small sample size probably the most important one. In spite of that, it also provides important contributions to the knowledge of the frontal sinus drainage pathways and the endoscopic anatomy of the frontal recess. Further studies correlating the endoscopic, radiological and intraoperative findings will be of utmost utility for the complete investigation of this anatomical region.
The results of this study allow us to conclude that:
None.
The authors declare no conflicts of interest or funding sources.

©2018 Ximendes, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.