Journal of
eISSN: 2379-6359


Literature Review Volume 14 Issue 3
1Department of Otorhinolaryngology, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Brazil
2Department of Neurology, Institute of Neuroscience Buenos Aires, Argentina
3Department of Radiology, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS) - Instituto do Cérebro (INSCER), Brazil
Correspondence: Camila Martins Brock, Otorhinolaryngology, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Avenida Ipiranga 6681 - Partenon, 90619900, Porto Alegre - RS, Brazil
Received: July 22, 2022 | Published: September 8, 2022
Citation: Brock CM, Carmona S, Hochhegger B. Analysis of body balance assessment results at posturography: an integrative review. J Otolaryngol ENT Res. 2022;14(3):62-68 DOI: 10.15406/joentr.2022.14.00508
Background: Posturography objectively assesses the central management of integrated peripheral sensory information (visual, vestibular, and proprioceptive) and the sensorimotor response required for balance. Recently published articles show the peculiarity of the currently available posturography devices and the variety of postural responses found.
Aim: The goal of this integrative review is to analyze the confluence between the outcomes of different studies involving adults and elderly patients with no instability complaints evaluated at posturography.
Methods: Of the 39 articles evaluated for eligibility, 9 articles met the criteria of this literature review. All studies included elderly patients (≥65 years). The posturography devices used were: NeuroCom®, Nintendo® Wii, and Bertec®.
Results: The objective data provided by posturography differ as regards the calculation of the oscillatory trajectory and the tests performed. Postural instability was significant under different conditions among the articles.
Conclusion: The final outcome analysis of the different studies showed that age and healthy aging result in modifications in posturography.
Keywords: posturography, healthy aging, postural balance
Postural control is the ability to maintain the desired position of the body in gravitational space, both in still position and in movement. The task of staying balanced in an upright position is a fundamental condition for carrying out daily tasks.1 However, postural control is not often studied in healthy individuals, but taken into consideration after the onset of diseases. The visual, vestibular, and somatosensory systems (especially in the lower limbs) are the main sensory systems required to maintain postural control. They are evaluated to identify early pathophysiological changes and to contribute to the rehabilitation of patients who complain of imbalance, dizziness, or vertigo.2
The upright posture with the upper limbs naturally hanging down at the sides of the body is a relevant model for the study of postural control. Posturography comes as a tool for such a purpose, as it objectively assesses the result of the central management of integrated peripheral sensory information (visual, vestibular, and proprioceptive) and the subsequent sensorimotor response needed for balance.3 Several posturography devices (portable and non-portable; with and without virtual reality) with variable accessibility have been developed. Studies on the feasibility of portable and low-cost devices aiming to favor patients' assessments have been performed - e.g., the Balance Angular Posturography (BAP), developed in 2017 by D'Albora.4,5
The many articles published in the last five years on this topic highlight the variety and peculiarity of the posturography devices available. The postural responses found may not present similar sensitivity, as the studies were mostly performed on patients with labyrinth symptoms and based on the diagnostic power of a particular test or device. This integrative review aims to analyze the confluence between the outcomes of different studies involving adults and elderly patients with no instability complaint.
Research strategy and study selection criteria
The literature search in databases, Medline (PubMed) and Lilacs, was carried out on the Regional Portal of the Virtual Health Library (VHS) using the following terms: "Posturography" AND ["healthy aging" OR "older adults" OR "elderly"]. Two independent reviewers carried out the search for articles (Figure 1).
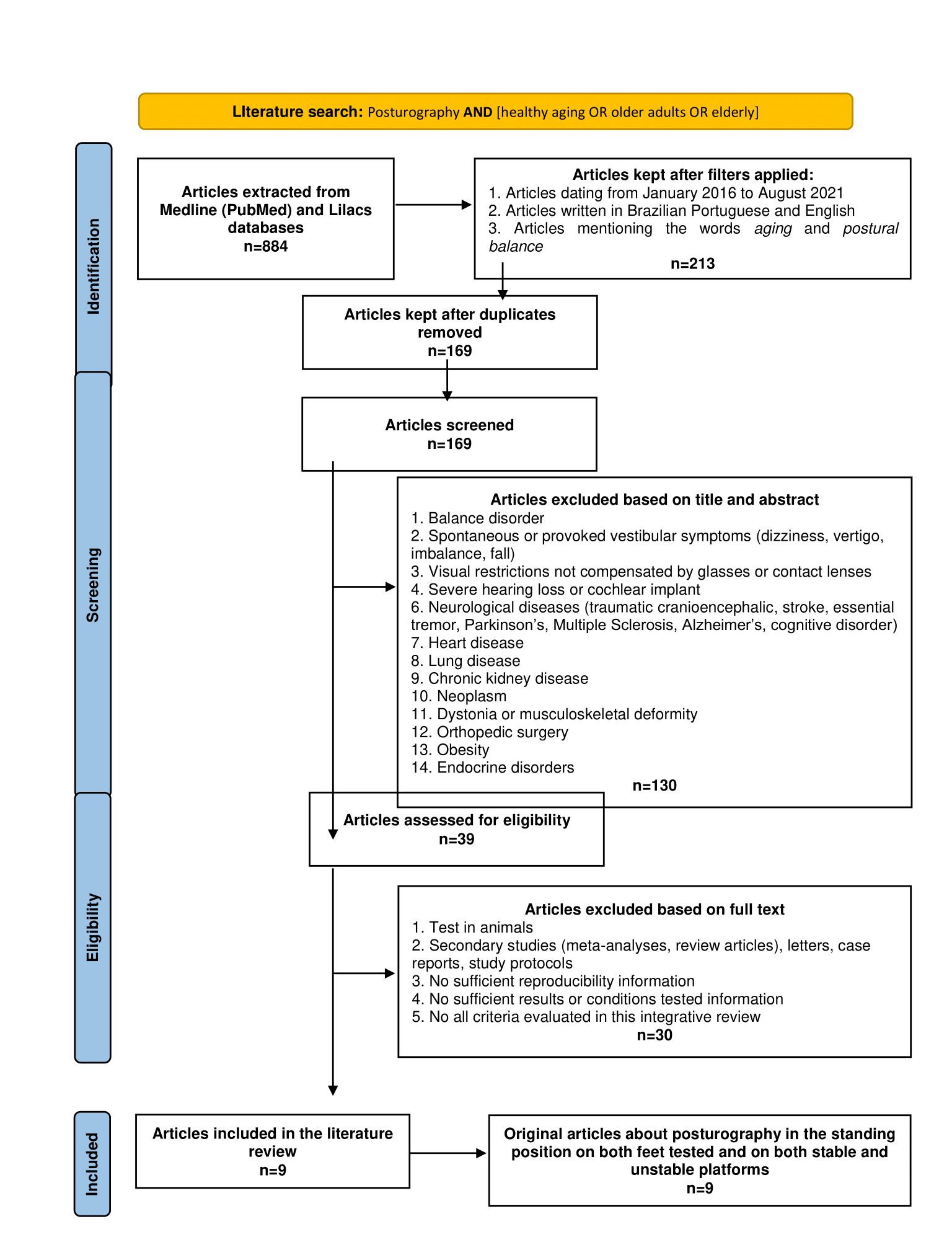
Figure 1 Summary of the literature search - PRISMA flow diagram.18
Initially, only studies in Brazilian Portuguese and English published in the last five years (from January 2016 to August 2021) and including specific subjects of aging and postural balance were selected. Articles were corrected for duplicity.
For the specific selection, the title and abstract of the articles were analyzed. Studies involving patients with balance disorders, spontaneous or provoked vestibular symptoms (dizziness, vertigo, imbalance, fall), visual restrictions not compensated by glasses or contact lenses, severe hearing loss, cochlear implant, neurological diseases “neurological diseases (traumatic head injury”, stroke, essential tremor, Parkinson's, Multiple Sclerosis, Alzheimer, cognitive disorder), heart disease, lung disease, chronic kidney disease, neoplasm, dystonia or musculoskeletal deformity, orthopedic surgery, obesity, diabetes mellitus, and other endocrine disorders were excluded from the first analysis. Thenceforth, articles were fully read to exclude those that had been performed with animals; had generated reports of secondary studies (meta-analyses, review articles), letters, case reports, study protocols; did not have sufficient reproducibility, results or conditions tested information; and did not meet all the criteria evaluated in this integrative review. The following criteria were applied in the final selection of studies: original article; posturography in the standing position on both feet and on both stable and unstable platforms.
Basic characteristics of the included studies
Of the 39 articles fully accessed, only 9 met the criteria of our literature review (Table 1): 6 cross-sectional studies, 2 case-control studies, and one cohort study. Each study was categorized by study and design, number of participants (N), sex, age (standard deviation or range), equipment, tests, and results. The total number of participants in each study ranged from 22 to 350; two studies only included female patients. All studies included elderly patients (≥65 years). The controls of both case-control studies consisted exclusively of young adult patients. Two of the cross-sectional studies compiled a wide age range, stratifying the results according to the age of participants by decade. The posturography devices used in the selected articles were: NeuroCom®, Nintendo® Wii, and Bertec®. One study evaluated postural control using two different devices, and compared the motor response registered in each test.
|
Study and design |
N |
Sex |
Age (standard deviation or range) |
Equipment |
Tests |
Results |
|
Alcock et al.6 - cross-sectional |
39 |
Female |
71,9 (7,2) |
NeuroCom |
6 conditions: 1 - Firm platform and opened eyes with fixed visual reference 2 - Firm platform and closed eyes 3 - Firm platform and open eyes with inaccurate visual reference (vertically oscillating) 4 - Unstable Platform and open eyes with fixed visual reference 5 - Unstable platform and closed eyes 6 - Unstable platform and open eyes with inaccurate visual reference (vertically oscillating) |
Significant instability: 16 (41%) under condition 5 e 27 (69,2%) under condition 6. |
|
Domènech-Vadillo et al.11 - cross-sectional |
350 |
Male 152 Female 198 |
37,38 (18-68) |
Nintendo Wii |
4 conditions: 1 - Firm platform and opened eyes 2 - Firm platform and closed eyes 3 - Unstable Platform and opened eyes 4 - Unstable platform and closed eyes |
Validation study, with a significant reduction of the global balance score the greater the height and the age. |
|
Faraldo-García et al.7 - cross-sectional |
70 |
Male 35 Female 35 |
44,9 (16-81) |
NeuroCom |
6 conditions: 1 - Firm platform and open eyes with fixed visual reference 2 - Firm platform and closed eyes 3 - Firm platform and open eyes with inaccurate visual reference (vertically oscillating) 4 - Unstable Platform and open eyes with fixed visual reference 5 - Unstable platform and closed eyes 6 - Unstable platform and open eyes with inaccuratd visual reference (vertically oscillating) |
Significant instability: age between 50-59 years and over 70 years old under condition 4. |
|
McDaniel et al.8- cross-sectional |
22 |
Male 19 Female 3 |
68,5 (58-81) |
NeuroCom |
6 conditions: 1 - Firm platform and opened eyes with fixed visual reference 2 - Firm platform and closed eyes 3 - Firm platform and open eyes with inaccurated visual reference (vertically oscillating) 4 - Unstable Platform and open eyes with fixed visual reference 5 - Unstable platform and closed eyes 6 - Unstable platform and open eyes with inaccurate visual reference (vertically oscillating) |
There was no significant instability in any of the conditions tested, in patients with moderate sensorineural hearing loss without and with bilateral hearing aids. |
|
Olchowik et al.9 - case-control |
241
Case: 141
Control: 100 |
Female |
Case: 65,5 (6,4)
Control: 20,7 (1,2) |
NeuroCom |
6 conditions: 1 - Firm platform and open eyes with fixed visual reference 2 - Firm platform and closed eyes 3 - Firm platform and open eyes with inaccurate visual reference (vertically oscillating) 4 - Unstable Platform and open eyes with fixed visual reference 5 - Unstable platform and closed eyes 6 - Unstable platform and open eyes with inaccurate visual reference (vertically oscillating) |
There was significant instability under all conditions tested, in the case group compared to the control group. |
|
Redfern et al.10 - case-control |
78
Case: 34
Control: 44 |
Case: Male 13 Female 21
Control: Male 12 Female 32 |
Case: 76 (4)
Control: 23,5 (2,9) |
NeuroCom |
6 conditions: 1 - Firm platform and open eyes with fixed visual reference 2 - Firm platform and closed eyes 3 - Firm platform and open eyes with inaccurate visual reference (vertically oscillating) 4 - Unstable Platform and opened eyes with fixed visual reference 5 - Unstable platform and closed eyes 6 - Unstable platform and open eyes with inaccurate visual reference (vertically oscillating) |
There was significant instability under conditions 1, 2, 3, 4 and 6, in the case group compared to the control group. |
|
Reinert et al.12 - cross-sectional |
90 |
Male 39 Female 51 |
76,1 (8,4) |
Bertec |
2 conditions: 1 - Maximum anteroposterior and latero-lateral oscillation on firm platform 2 - Maximum anteroposterior and latero-lateral oscillation on unstable platform |
The limit of stability, both anteroposterior and latero-lateral, is lower in individuals from 80 years old. |
|
Sparto et al.13 - cohort |
222 |
Male 100 Female 122 |
85 (3) |
Bertec |
4 conditions: 1 - Firm platform and open eyes 2 - Firm platform and closed eyes 3 - Unstable Platform and open eyes 4 - Unstable platform and closed eyes |
There was significant instability under condition 3 (compared to conditions 1 and 2) and under condition 4 (compared to all other conditions). |
|
Trueblood et al.14 - cross-sectional |
50 |
Male 17 Female 33 |
44,5 (20-69) |
Bertec versus NeuroCom |
6 conditions: 1 - Firm platform and opened eyes with fixed visual reference 2 - Firm platform and closed eyes 3 - Firm platform and opened eyes with virtual visual reference 4 - Unstable Platform and open eyes with fixed visual reference 5 - Unstable platform and closed eyes 6 - Unstable platform and open eyes with virtual visual reference |
There was significant instability with the Bertec equipment, only in age between 60-69 years old under condition 4 (compared to NeuroCom equipment). |
Table 1 Profile of selected articles
Evaluation of postural control aging
Alcock et al.6 carried out a cross-sectional study with 39 elderly women using NeuroCom® posturography. The authors studied the postural response under six different conditions, combining stable surface, unstable surface (anteroposterior oscillation platform), with open eyes with fixed visual reference, open eyes with inaccurate visual reference (vertically oscillating), and closed eyes. Significant instability occurred in 41% of the patients on unstable platform and closed eyes, and in 69.2% of the patients on unstable platform and open eyes with inaccurate visual reference (vertically oscillating).
Faraldo-García et al.7assessed the balance of 35 men and 35 women, organized by age groups (<20, 20-29, 30-39, 40-49, 50-59, 60-69, >70 years old), using the same posturography equipment and under the same conditions (also an observational study). Patients aged between 50-59 years and over 70 years showed significant instability only on unstable platform and with open eyes with fixed visual reference. McDaniel et al.8 conducted the same study strategy with 22 participants (58-81 years), predominantly male (19 men), with moderate sensorineural hearing loss. All underwent the test with and without an individual bilateral hearing aid, no statistical difference was observed.
Olchowik et al.9 studied 241 women divided into 141 adults and/or elderly (case group) and 100 young adults (control group), also using NeuroCom®, showing significant instability between the two groups under all conditions tested. Redfern et al.10 used the same design case-control to study 78 patients, 25 men and 53 women, contradicting such instability when an unstable platform and closed eyes were combined.
Domènech-Vadillo et al.11 concluded a cross-sectional validation study for the assessment of postural control via Nintendo® Wii posturography. A total of 350 (198 women), aged between 18 and 68 years (average 37.38), were tested under four conditions that combined stable surface, unstable surface, open eyes, and closed eyes. Global balance score decreased with increasing height and age.
Reinert et al.12 observed the performance of 90 elderly (51 women) with Bertec® posturography under two conditions: maximum antero-posterior and latero-lateral oscillation on stable surface and on unstable surface, without a specific visual protocol. Stability limit under both conditions was lower in the elderly aged >80 years. Sparto et al.13 followed the balance of 222 elderly (122 women) under four combined conditions: stable surface, unstable surface, open eyes, and closed eyes. Instability was found when unstable platform and open eyes were combined, and, especially, with closed eyes.
Trueblood et al.14 evaluated the response of 17 men and 33 women, aged between 20 and 69 years (average 44.5), under six different conditions, which combined stable surface, unstable surface, open eyes with fixed visual reference, open eyes with unfixed reference for virtual reality, and closed eyes. Tests were carried out with two different posturography equipment’s, with the intention of comparing the results. Significant instability was registered only for participants aged between 60 and 69 years, on unstable platform and open eyes with fixed visual reference, when evaluated using Bertec® compared to NeuroCom®.
Posturography equipment differs in relation to the calculation of the oscillatory trajectory and the conditioned tests. There is no consensus as to which parameter (area, velocity, total distance, or frequency) should be used to quantitatively assess balance, or on the standardization of sensory stimuli. NeuroCom® calculates the maximum oscillation amplitude in percentage (score ranging from 0 to 100% = stability), only in the antero-posterior direction, based on the displacement of the body’s center of gravity, measured by the center of pressure detected on the platform support.
The strategies used to maintain postural control seem to depend more on somatosensory feedback from lower limbs than on feedback from other systems - visual and vestibular. Considering the body as an inverted pendulum rotating around the ankle joint, reduced muscle strength and mobility resulting from aging recruits the participation of proximal musculature, i.e., the hip, to comply with the motor demand.3 However, when somatosensory information remains challenging, as in the balance test on an unstable surface, study participants rely more on visual cues. Consequently, vulnerability to instability increases if both afferences - proprioceptive and visual - are in conflict.15 Such outcome was found in the study by Alcock et al.,6 although proprioceptive disturbances in daily tasks are multidirectional, not bidirectional as to the oscillation provoked by the equipment.
Conversely, Faraldo-García et al.7 argued that postural instability was significant under the unstable surface and open eyes with fixed visual reference condition. Their study assessed a larger population, which was divided into age groups, and found support in senile visual deterioration (presbyopia) not compensated by glasses, between 50 and 59 years and > 70 years.
The role the cerebellum has as the main control system is to manage somatosensory or proprioceptive, visual, and vestibular afferents to produce a perfectly adjusted motor efferent response. Greater accuracy in the peripheral sensory information and better cognitive conditioning for proper central interconnection generate a better postural control. In this regard, McDaniel et al.8 assessed the response of bilateral hearing aids in patients with moderate sensorineural hearing loss, given that auditory biofeedback provides satisfactory postural corrections, and improves balance. However, the study did not replicate the strategy; authors replaced it by multi-talker babble amplification, limiting the comparison of the results found. Furthermore, the belief that hearing aids reduce cognitive decline needs to be considered when other variables are included (such as the time elapsed between the diagnosis of hearing loss and the adoption of the hearing aid, adaptation to the device, the years of use), and which affect the success of the hearing loss treatment and remodel its consequences.16
In addition to sensory polyneuropathy of the distal extremities and stiffening of the ankle joint, the vestibular system also suffers from age-related degeneration, both peripheral (due to loss of otoconia, vestibular hair cells, and vestibular neurons) and central (due to reduced arterial perfusion vertebra basilar). When added to the reduction in visual acuity, the sensory deficiencies collectively configured a pattern of senile balance, the outcome of which may be postural instability at the expense of lesser oscillatory flexibility. However, imbalance in the older population may be considered an “age-concomitant” rather than an “age-dependent” condition, as the clinical impact of a presbyvestibulopathy is modulated both by the functional state os these physiologic systems and by the ability to reweight sensory inputs and the level of central nervous system plasticity.17 Olchowik et al.9 corroborated these data, supported by the understanding that young adults have their cognitive functions preserved for multitasking. On the other hand, even when a smaller population is studied, Redfern et al.10 opposed the instability in the condition that combined unstable platform with closed eyes, defending the idea that, when proprioception is unreliable, and vision is blocked, vestibular information becomes categorical for building a new visuospatial perception. Such skill rectifies the influence of cognition and the impact of aging on postural control.
Unlike devices which use a dynamometric platform, as the NeuroCom®, the Nintendo® Wii software estimates the elliptical area in gross value, not in cm2, to calculate the global balance score. Another difference lies on the unstable surface used: while NeuroCom® uses a mobile platform, Nintendo® Wii uses high-density foam. In this case, the foam properties influence postural sway, being their specifications relevant for the reproducibility of results and for the comparison between studies. Domènech-Vadillo et al.11 used a 50 × 40 × 14 cm (width × length × thickness) 40 kg/m3 (density) foam. Global balance score was found to be influenced by height, age, and center of pressure, and it increases as height and age decrease, which means that postural control is worse in taller and elder individuals. However, by stratifying the score into the two variables, the influence of the center of pressure disappears due to the change in it according to height and age.
Bertec® and NeuroCom® are very similar posturography devices: Bertec® also calculates the oscillation through the variation of the center of pressure detected in the support platform. However, foam needs to be included to provide instability. Reinert et al.12 used a 50 × 41 × 6 cm (width × length × thickness) piece of foam and proved that the stability limits - i.e., the maximum antero-posterior and lateral-lateral oscillation intervals - progressively reduce as age advances, even on a stable surface. Given that aging process compromises physiological capacities, such as tactile sensation, flexibility, and strength, the result reinforces the need to age group the target elderly population (60 to 69, 70 to 79, and >80 years), as the average stability limits between groups may disguise normal and pathological changes that are potentially important in postural control. Sparta et al.13 argued that the expressive instability on the foam (7.5 cm thick), regardless of the visual parameter, confirmed the supremacy of proprioceptive information in postural control as an adaptive process of aging.
The latest version of Bertec® includes a stationary spherical dome as a visual environment, capable of creating a constant self-movement illusion through virtual reality. Unlike the complete NeuroCom® system, which adds a fixed visual projection that allows the use of an anatomical reference point forward, the visual projection of an endless tunnel brought about by Bertec® nullifies such feature. The normative values of the different posturography equipment may, therefore, end up being not equivalent, since the sensory systems involved in balance are sensitized in different ways. Thus, it is plausible that the condition being tested may indicate discrepant results. Trueblood et al.14 showed that visual sensitization in the Bertec® test on an unstable surface and with open eyes and fixed visual reference resulted in significant instability as compared to NeuroCom®.
Apart from technical differences between methods found during the review, it is important to highlight that age and aging are the main causes of modifications in posturography results, ruling out other causes considered to be including and excluding criteria. This factor is cardinal not only to interpret posturography results but also because balance disorders and falls have been shown to predict a reduced ability to carry out activities of daily living and a substantial reduction in quality of life.
The supremacy of proprioception and the construction of visuospatial perception (vestibular ability) as adaptive processes of aging reinforce the sensitivity of posturography for the assessment of balance in the elderly. The central management of peripheral sensory afferences (proprioceptive, vestibular, and visual) depends on the accuracy and the confluence of at least two systems, but also on the cognitive reserve available for the compensation of the compromised system. Strategies for greater peripheral sensory sensitization have been studied even in the static evaluation of postural control: including auditory biofeedback, virtual reality, and head lateralization, aimed at registering the influence of each system on the motor response. Its research, initially involving patients with no instability complaints, promotes future studies on the postural repercussion in imbalance, dizziness, or vertigo conditions as long as they are protocoled.
None.
The authors have equally contributed to this work and share first authorship.
None.

©2022 Brock, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.