Journal of
eISSN: 2379-6359


Aim: To prospectivelycompare monopolarelectrocautery tonsillectomy and thermal welding system (TWS) tonsillectomy in adult patients.
Methods: Fifty patients over 20 years old, admitted for tonsillectomy between January 2010 and March 2012, were randomized to have one tonsil removed using monopolar electrocautery and the other tonsil removed using the TWS. Subjects used the FACES scale to rate the pain on each side 21 days postoperatively. Postoperative hemorrhaging and tonsillar fossa woundhealingwere also recorded.
Results: The mean time required to remove one tonsil was 8.3±1.5 min for the TWS and 7.5±1.6 min for monopolar electrocautery (p=0.033). There was no significant difference between monopolar elecrocautery and TWS groups in terms of postoperative FACES pain scores and bleeding rates. The tonsillar fossa wound healing scores were statistically significantly higher for monopolar electrocautery tonsillectomy versus the TWS (p<0.001).
Conclusions: Since the TWS is more expensive than monopolar electrocautery and use of the TWS did not confer any clear advantage over monopolar electrocautery for tonsillectomy in terms of postoperative pain, hemorrhage, and wound healing; monopolar electrocautery should be preferred over TWS for tonsillectomy operations.
Keywords: thermal welding system, monopolarelectrocautery, postoperativepain
Tonsillectomy is frequently performed procedure in otorhinolaryngology. The technique, which involves dissection of the tonsillar tissue from the underlying pharyngeal constructor muscles, has changed little in the last 60 years.1 Despite the use of several new methods and devices, cold dissection tonsillectomy is still considered as the gold standard.
There have been many controversies about tonsillectomy techniques and whether they provide better conditions with more advantages and rarer complications. Several methods have been used, including the classical technique, monopolar and bipolar electrocautery, radiofrequency ablation, carbon dioxide lasers, endoplasmic microdebriders, cryosurgery, harmonic scalpels, and argon plasma coagulation.2–4 Many surgeons prefer electrocautery to cold instruments in adult tonsillectomy because intraoperative bleeding is significantly reduced, although the length of postoperative pain and the recovery time may be longer with electrocautery.5,6
Tonsillectomy is considered to be a more difficult operation in adults than in pediatric patients. Specifically, the increased fibrosis along the tonsillar capsule and more prominent blood vessels in adults can lead to an increased operative time and intraoperative bleeding versus pediatric tonsillectomy. Tonsillectomy is associated with notable morbidity, including intraoperative blood loss, postoperative pain and hemorrhage, painful swallowing, and limitations in daily activities and diet.2,3 Thus, no consensus has been reached regarding the optimal technique with which to decrease morbidity associated with tonsillectomy.
The thermal welding system (TWS) (ENTceps; Starion Instruments, Saratoga, CA, USA) is an alternative technique for performing a tonsillectomy. The device has received Food and Drug Administration approval. The TWS uses a direct head and pressure to divide tissues. The head is localized at the tip of the instrument. The main operating principle of this system is tissue dissection as a result of cellular denaturation, with the generation of highly focused thermal energy. With pressure, protein molecules dissolve and fuse together, resulting in tight seal formation.7 A few recent studies have assessed the utility of this new technique and found that tissue injury is minimal with the TWS.8 These studies introduced the new technique as a safe method for tonsillectomy operations. They also reported that it provides sufficient hemostasis during dissection and decreases operating times.
Monopolar electrocautery (Electrosurgical Pencil; Bovie, Aron, USA) is one of the most frequently used instruments for tonsillectomies. Monopolar electrocautery generates an electric arc between the tissue and instrument, which ablates the tonsillar tissue. Electrocautery cuts tissues at temperatures of 400°C or higher. Electrocautery operates by applying high temperatures right to the tonsillar area, detaching the tissue fixing the tonsil from the underlying pharyngeal muscles while also coagulating blood vessels. Some degree of thermal injury to nearby structures is a major problem with its use, which is related to postoperative morbidity. Thermal damage to the pillar mucosa can slow down healing and amplify postoperative pain and late complications, including postoperative bleeding.9
In order to contribute to the debate on the optimal treatment, we intended to assess the efficacy and safety of the TWS versus monopolar electrocautery tonsillectomy in terms of intraoperative blood loss, postoperative hemorrhage rate, operation duration, tonsillar fossa healing, and, especially, postoperative pain in adult patients having repeated chronic tonsillitis.
A prospective, randomized, double-blind, controlled clinical study was conducted to evaluate the effects of standard monopolar electrocautery versus the TWS in adult patients with repeated chronic tonsillitis. In total, 50 patients over 20 years old, admitted for tonsilectomy between January 2010 and March 2012, were included. The indications for tonsillectomy were chronic recurrent tonsillitis (with no history of tonsillitis within 4 weeks prior to surgery) and snoring caused by hypertrophic tonsils. Patients having peritonsillar abscess before, current analgesic utilization for another medical condition, and bleeding syndromes were excluded. Written informed consent was obtained from all patients.
Surgical technique
All surgeries were achieved by the same otolaryngologists. The method used, the relevant side, and the operation duration was recorded by the operating surgeon. All postoperative evaluations were performed by a different clinician. Both the clinician and the patients were blinded to the surgeon’s choice of technique. The anesthetic approach was identical for all patients: induction was performed using intravenous fentanyl, propofol (2 mg/kg), and atracurium (0.5 mg/kg) following intubation. Maintenance of anesthesia was succeeded with a mixture of nitrous oxide, oxygen, and propofol. After the induction of anesthesia, each patient was positioned in the Rose position and a Davis-Boyle mouth gag, supported by Draffin bipods, was inserted into the mouth. Each tonsil was grasped and medialized using an Allis clamp. Immediately prior to surgery, routine antibiotic treatment, analgesia, and dexamethasone (0.15 mg/kg) were administered intravenously to all patients. One of the tonsils of the patients were removed using the TWS and the other one using monopolar electrocautery. The side on which TWS or monopolar electrocautery to be performed was determined by randomization. The randomization was made by the use of a random number generator (Excel, Microsoft Corp, Resmond, Washington). Through the randomization process, right tonsil of half of the patients removed using the TWS and their left tonsil removed using monopolar electrocautery. The other half had their left tonsil removed using the TWS and their right tonsil removed with monopolar electrocautery. The information about which technique was used was not given to the patients. The monopolar electrocautery probe and TWS forceps used are shown in Figure 1 & Figure 2. TWS tonsillectomy is an extracapsular technique. For the TWS, the instruments were set up according to the instructions. The superior pole was grasped with Allis forceps. No mucosal incision was carried out. First, the anterior pillar was dissected with (TWS) (ENTcepsStarionInstruents, Saratoga CA, USA). Next, the dissection was continued from the superior pole to the inferior pole. Small bleeding vessels and visible intact blood vessels were coagulated with the same forceps. If bleeding persisted, hemostasis was achieved with a 3/0 rapid vicrile suture. Monopolar electrocautery tonsillectomy is another extracapsular technique. The bulge of the tonsil was identified and incisions were made by monopolar electrocautery (Electrosurgical Pencil; Bovie, Aron, USA) at 20 W in the anterior superior part, just inside the anterior pillar, extending superiorly and posteriorly. The pericapsular dissection was carried out with care to keep the cleavage within the capsule. Bleeding was stopped by coagulation before and after dissection. If bleeding persisted, hemostasis was achieved with a 3/0 rapid vicrile suture. After absolute hemostasis was achieved, the mouth gag was removed, the temporomandibular joint was controlled, and the patient was extubated. The operating time was calculated from the beginning incision to complete hemostasis. The volume of blood lost was estimated and recorded for each patient from the suction bottle.
Postoperative evaluation
The first liquid diet was given to the patients 4 h after the operation. All patients were discharged the day after surgery with an analgesic (paracetamol) and antibiotics (amoxicillin/clavulanic acid) in weight-proportional doses.Postoperative pain was assessed using the 10-point Wong-Baker FACES scale scale in which a score of ‘0’ equals no pain and ‘10’ equals the worst pain imaginable, was used.10 Using the 10-point Wong-Baker FACES chart, the patient was asked to pick which face described the pain for each side from operation day to 21 days after the operation. The patients were monitored postoperatively for 21 days using questionnaires completed by the patients. Daily assessments included the pain score, recorded using the scale twice daily, first thing in the morning before taking any medication or drinking anything and then in the evening before going to bed. The patients were encouraged to use paracetamol every 4 h on an as-needed basis for analgesia. The patients were seen 21 days after surgery, and, at the last visit, the patient questionnaires were collected.
Healing in tonsillary fossa was evaluated according to the method of Magdy et al.,4 Edema, erythema, fossa whitening, and wound healing were rated and evaluated at 1, 3, 5, 10, 14, and 21 days postoperatively. The scoring system used for healing in tonsillary fossa is shown in Table 1. The degree of healing in tonsillary fossa was evaluated by summing the scores; the maximum score of 5 points indicated no healing in tonsillary fossa, while the minimum score of 0 points indicated complete tonsillar fossa wound healing.
|
Absence |
Presence |
Severe |
Erythema |
0 |
1 |
2 |
Oedema |
0 |
1 |
|
Fossawhitening |
0 |
1 |
|
Woundhealing |
1 |
0 |
|
Table 1 Scoringsystemfortonsillarfossawoundhealing.11
All intra- and postoperative complications were recorded.
Statistical methods
The data were analyzed using usingthe SPSS software package (Statistical Package for Social Sciences, version 12.0, SPSS Inc., Chicago, Illinois, USA). Descriptive statistics (mean, median, standard deviation, minimum, and maximum values) were calculated for numerical and categorical variables. The Mann-Whitney U-test was used to compare the TWS and monopolar electrocautery. A repeated-measurements analysis of variance was used to compare repeated measurements.
Demographics
A total of 50 patients, aged 20‒47 years, were included intothestudy. There were 38 males (meanage, 29±8.9 years) and 12 females (mean age, 28±7.6 years). Forty-four patients had their tonsils removed because of chronic tonsillitis, and six underwent tonsillectomies for enlarged tonsils causing snoring.
Operative findings
The mean time required to remove one tonsil was 8.3±1.5 min for the TWS and 7.5±1.6 min for monopolar electrocautery. The operating time for the TWS was statistically significantly longer than that for monopolar electrocautery (p=0.033), although the time difference was not considered clinically significant.
No serious intraoperative hemorrhage was encountered with either the TWS or monopolar electrocautery tonsillectomy.
Postoperative findings
Pain: There was no significant difference between the mean FACES pain scores of patients in monopolarelecrocautery and TWS groups, which were recorded daily in the morning and evening for 21 days (Table 2) (Figure 3).
Day |
Morning |
Evening |
||||
|---|---|---|---|---|---|---|
|
Monopolarelectrocautery |
TWS |
pValue |
Monopolarelectrocautery |
TWS |
pValue |
1 |
5.47±2.23 |
5.41±2.24 |
0.782 |
5.47±2.28 |
5.40±2.15 |
0.834 |
2 |
5.56±2.33 |
5.36±2.34 |
0.783 |
5.56±2.27 |
5.38±2.15 |
0.834 |
3 |
5.84±2.25 |
5.44±2.10 |
0.169 |
6.14±2.40 |
5.43±2.30 |
0.123 |
4 |
5.58±2.21 |
5.12±2.63 |
0.383 |
5.52±2.25 |
5.08±2.32 |
0.085 |
5 |
5.25±2.32 |
5.01±2.25 |
0.268 |
5.02±2.35 |
4.85±2.54 |
0.354 |
6 |
4.7±2.03 |
4.02±2.36 |
0.067 |
4.65±2.32 |
3.98±2.38 |
0.065 |
7 |
4.65±2.45 |
4.06±2.54 |
0.256 |
4.81±2.43 |
4.13±2.30 |
0.126 |
8 |
4.73±2.03 |
4.25±2.65 |
0.276 |
4.75±2.54 |
4.27±2.35 |
0.352 |
9 |
5.24±2.37 |
4.43±2.75 |
0.287 |
4.72±2.59 |
3.95±2.23 |
0.139 |
10 |
4.22±2.51 |
3.62±2.12 |
0.247 |
3.8±2.24 |
3.34±1.98 |
0.345 |
11 |
3.85±2.45 |
3.25±2.45 |
0.147 |
3.76±2.36 |
3.24±2.30 |
0.298 |
12 |
3.58±2.32 |
3.22±1.86 |
0.342 |
3.45±2.37 |
3.21±2.65 |
0.452 |
13 |
3.32±2.27 |
2.96±2.08 |
0.478 |
3.21±2.65 |
2.87±2.17 |
0.597 |
14 |
2.6±1.97 |
2.33±1.67 |
0.540 |
2.45±1.74 |
1.97±1.32 |
0.443 |
15 |
2.31±1.65 |
1.96±1.74 |
0.432 |
2.27±1.87 |
1.94±1.63 |
0.386 |
16 |
2.24±1.86 |
1.94±1.58 |
0.478 |
2.24±1.7 |
1.96±1.49 |
0.375 |
17 |
2.21±1.67 |
1.93±1.57 |
0.378 |
2.18±1.65 |
1.92±1.76 |
0.437 |
18 |
2.16±1.86 |
1.90±1.75 |
0.432 |
1.87±1.65 |
1.72±1.65 |
0.364 |
19 |
1.54±1.53 |
1.48±1.34 |
0.362 |
1.46±1.45 |
1.38±1.43 |
0.276 |
20 |
1.43±1.54 |
1.36±1.53 |
0.321 |
1.38±1.64 |
1.34±1.63 |
0.213 |
21 |
1.23±1.34 |
1.12±1.43 |
0.432 |
1.13±0.75 |
1.03±0.53 |
0.321 |
Table 2 The mean(±standarddeviation) morning and evening FACES pain scores of patients in monopolarelecrocautery and TWS groups, which were recorded daily for 21 days aftertheoperation
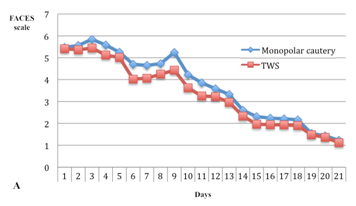
Figure 3A & B: The mean FACES pain scores of patients in monopolarelecrocautery and thermal welding system (TWS) groups, which were recorded in themorning (A) andevening (B) daily for 21 days aftertheoperation.
Hemorrhage: There were four postoperative hemorrhages requiring a revisit the operating room for control. In three patients, the bleeding occurred on the side where monopolar electrocautery had been used. This bleeding occurred on postoperative days 3, 7, and 11. There was one case of postoperative bleeding on the side where the TWS had been used, and the bleeding occurred on postoperative day 10. There were two other minor bleeding episodes on the TWS side that required the patients to seek medical attention but did not require a visit the operating room. Both of these were treated successfully with topical silver nitrate on postoperative days 9 and 11. Thus, the bleeding rates for the TWS and monopolar electrocautery were 6% and 6%, respectively. There was no significant difference in the postoperative bleeding rate between the TWS and monopolar electrocautery.
Tonsillar fossa healing
In the analysis ofthe healing in tonsillary fossa wound scores evaluated on days 1, 3, 5, 10, 14, and 21 postoperatively were statistically higher for monopolar electrocautery tonsillectomy versus the TWS (p<0.001; Figure 4).
Figure 4 Estimatedmarginalmeanscoresfortonsillarfossawoundhealingduringpostoperativefollow-ups. Tonsillar fossa wound healing scores did not show significant difference in each group (p=0.107), but the scores were statistically significantly higher for monopolar electrocautery tonsillectomy versus the TWS (p<0.001).
Complications
No intraoperative complication occurred. Five patients had postoperative low-grade fever, two reported vomiting, and constipation occurred in three patients.
In this prospective, double-blind, randomized study, we compared monopolar electrocautery and TWS techniques for tonsillectomy in adults, and showed that none of the surgical techniques had clear advantage in terms of postoperative pain, hemorrhage, time of operation and wound healing. Therefore, we suggest that since the TWS is more expensive than monopolar electrocautery, monopolar electrocautery, which have similar postoperative outcome with TWS.
Although there are several tonsillectomy methods in use, there is little consensus among otolaryngologists about the optimal technique. Postoperative pain and hemorrhaging are the most significant complications following tonsillectomy operations. These morbidities compromise patient health and safety, the quality of recovery, amount of analgesics used, time to return to a normal diet and activity, and time to return to work. Complication-related visits to the emergency department, otolaryngology department, or operating room increase medical personnel workload and hospital costs.
Because of the highly innervated tissue surrounding the tonsils, within the pharyngeal muscles, a tonsillectomy almost always results in postoperative pain. In the postoperative period, referred otalgia also occurs and may be mediated by nerve endings exposed after removal of the tonsils.
The TWS is a new tonsillectomy technique that coagulates and dissects the tissue by directly applying thermal energy and pressure.11 This new thermal instrument was developed on the basis of the hypothesis that the desired protein denaturing effects could be accomplished most effectively applying direct thermal heating of the tissue rather than an intermediate form of energy (e.g., electric, ultrasonic, laser, or radiofrequency). The thermal energy-generating element is a regular resistance heating wire, driven by a low-voltage direct current. The TWS is not a bipolar instrument because no electric current spreads through the tissues grabbed between the instrument’s jaws. The operational part of the instrument is the heating element, made of nichrome with a thermally insulated backing. This layer isolates the heating effect of the nichrome wire from the other parts of the instrument and blocks the underside of the jaw from becoming hot. When the blades of the jaw are closed, the thermal blade is pressed against a conformable silicone ‘boot’, which is mounted on the other blade of the jaw. The silicone ‘boot’ helps generate a rated thermal profile. The importance of the graded temperature profile is that the device carries out cutting and coagulation simultaneously. The device seals both ends of a vessel on either side of the cut zone, in as much as the profile has a bilaterally symmetrical shape. Due to the radiation of heat by the nichrome element, the size of the cutted zone is slightly greater than the definite pure diameter of the wire. In this region, the temperature is adequate to actually incise tissue by use of direct vaporization, with very little charring. This temperature has been measured to be in the range of 300‒400°C. At distances greater than approximately 500 µm from the middle of the wire, the temperature falls to below 100°C, which is the ideal temperature for coagulating and sealing tissues by means of protein denaturation. The other crucial function of the silicone ‘boot’ is that it enables the device to produce a strong seal on the ends of cut vessels. The goal is to exert pressure or crimp the vessel walls together in the lower temperature coagulation zone. Karatziaset al.,8 carried out tonsillectomies in 50 patients with the TWS and found that there was no measurable bleeding during surgery. Our findings also revealed no intraoperative bleeding and only one case of postoperative bleeding on the side where the TWS had been used. There was also no major difference in the bleeding rate postoperatively between the TWS and monopolar electrocautery in our study. Karatzias et al.,8 also reported that the mean operation time and time to return to a normal diet were 23 min and 8.7 days, respectively.8 The operation time with TWS was much shorter in our study than reported by Karatzias et al.,8 Despite reporting an improvement in pain with the method, there were no statistically significant data by Karatzias et al.8 They emphasized that TWS was a safe and an effective method that prevented intraoperative bleeding.8 There is no need for special training to use this technique. The most disadvantageous factor in this technique is that single-use ENTceps increase the cost of the operation.
Monopolar electrocautery is the most common method of tonsillectomy; it is preferred because it is known to reduce intraoperative bleeding and facilitates hemostasis.12‒14 In the present study, no significant difference was followed between the frequency of hemorrhage encountered with the TWS versus monopolar electrocautery. Another reason for performing electrocautery tonsillectomies is the shorter operation time matched with other tonsillectomy techniques such as radiofrequency, plasma-mediated ablation, and the use of microdissection needles.15‒17 We found that the operative time for the TWS was significantly longer than that for monopolar electrocautery (8.3±1.5 min vs. 7.5±1.6 min; p=0.033), although this difference in operation time was statistically significant, it was clinically insignificant.
In the present study, we found no clear advantage of monopolar electrocautery and TWS over each other with respect to operative time, post operative bleeding, pain, and wound healing. Taking into the consideration of limitations of our study, such as low sample size, dependent groups, short postoperative follow-up, this is the first study comparing monopolar electrocautery and TWS techniques for tonsillectomy in adults.
In this study, we showed that the postoperative pain, hemorrhage, the degree of tonsillar fossa healing, and operation time were similar between the monopolarelectrocauteryand TWS techniques for tonsillectomy in adults. Since the TWS is more expensive than monopolar electrocautery and use of the TWS did not confer any clear advantage over monopolar electrocautery for tonsillectomy.Further randomized, controlled studies with larger sample sizes are needed to further clarify and evaluate the morbidity associated with monopolarelectrocautery versus the TWS for tonsillectomy.
None.
The author declares there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.