Journal of
eISSN: 2379-6359


Case Report Volume 10 Issue 5
1Department of Oral Medicine and Radiology, Century International Institute of Dental Sciences and Research Centre, India
2House Surgeon, Century International Institute of Dental Sciences and Research Centre, India
3Head of Department, Department of Oral Medicine and Radiology, Vydehi Institute of Dental Sciences and Research Centre, India
Correspondence: Nilofer Halim, Senior Lecturer, Department of Oral Medicine and Radiology, Century International Institute of Dental Sciences and Research Centre, Poinachi, Kasaragod, Kerala, India, Tel 91 8089794270
Received: August 20, 2018 | Published: October 4, 2018
Citation: Halim N, Jose D, Kalkur C, et al. Oral arteriovenous malformation with phlebolith. J Otolaryngol ENT Res. 2018;10(5):281?283. DOI: 10.15406/joentr.2018.10.00362
Arteriovenous malformation of head and neck is a rare vascular anomaly but when present, it is persistent and progressive in nature. It can also represent a lethal benign disease.1 Arteriovenous malformation occurs due to the failure of complete involution of fetal capillary bed resulting in the development of abnormal connections between arteries and veins.2 Associated important clinical signs are warmth, a palpable thrill and a bruit. Most of the case reports of vascular lesions in oral cavity have been presented in relation to tongue, lips and in palate. Asymptomatic lesions tend to get neglected by patients. Here, we present a case of multiple vascular malformations on tongue and lips in a 32 year old female patient which was diagnosed based upon her oral lesions. Multiple radiopaque phleboliths were observed in panoramic radiograph.
Arteriovenous malformation is a type of vascular anomaly where there is a stunt between arterial and venous vasculature. Vascular malformations are seen in about 1% of the population. But, many of them do not present themselves for treatment.1 Progression of AVM is commonly induced by puberty, trauma and pregnancy. Those induced by trauma usually involve a single vessel whereas congenital form of AVM usually involves multiple vessels.3 Most AVMs are present at birth, but become clinically significant later1. In oral cavity, these lesions most commonly occur on anterior two-third of tongue, palate and gingival and buccal mucosa.4
These lesions can be diagnosed by plain radiography, CT scans, magnetic resonance imaging or angiography. The most conventional modern approach for its management includes various sclerosing agents and embolization combined with surgical treatment.5–7 In this paper, we present a case of AVM involving the tongue, lips of a 32 year old female.
A 32 year old female reported to the Department of Oral Medicine and Radiology Century Dental College with the chief complaint of forwardly placed tooth in the lower front tooth region since 6 months. There were no associated symptoms. There was no related history in any of her family members. Her previous medical history revealed that she had undergone surgery for the removal of similar lesion on the lower lip a year back. On general physical examination, she was moderately built and nourished. On extra oral examination, patient had a cherubic appearance. There was no significant facial asymmetry detected. TMJ showed midline deflection to right at rest. Mouth opening was within normal limit and clicking was absent.
On intra oral examination, a solitary bluish nodule measuring less than 2 cm in size was observed on the upper left side of labial mucosa (Figure 1). The lesion was soft in consistency, non tender, easily compressible, pulsatile at latero-posterior aspect and was not fixed to underlying structures. Greyish nodule less than 1 cm was also seen on left side of labial mucosa opposing 33 and 32 region. A tumor like growth with bluish discoloration measuring about 1x2cm in size was observed on the antero-lateral border of anterior two-third of tongue partly involving dorsum and ventral surfaces of tongue. Surface of the swelling was smooth and borders were well defined (Figure 2). There was no ulceration or bleeding or any discharge from tongue and surrounding areas of the tongue were normal. On palpation, all inspectory findings were confirmed, the lesion readily blanched on application of pressure. Identical lesion was seen on postero-lateral aspect of tongue on left side close to lingual tonsil. Chair side diascopy was done and the lesion did not blanch under pressure (Figure 3). Based on history and clinical findings, a provisional diagnosis of vascular malformation was made and differential diagnosis of Hemangioma was considered. Patient was advised for Orthopantamography, the findings of which revealed multiple radiopaque discrete calcifications with lamination over left hyoid bone and right ramus of mandible near mandibular foramen suggestive of plebolith (Figure 4). Since the lesion was asymptomatic, the patient was followed up and advised for Doppler study of facial region and asked to report if any changes are noted.

Figure 2 A tumor like growth with bluish discoloration measuring about 1x2cm in size on the antero-lateral border of anterior two-third of tongue. Surface was smooth and borders are well defined.
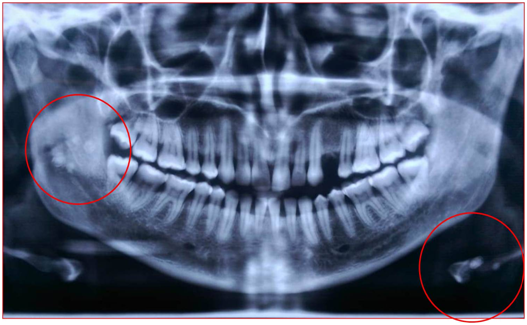
Figure 4 OPG showing multiple radiopaque discrete calcifications with lamination over left hyoid bone and right ramus of mandible near mandibular foramen suggestive of phlebolith.
The patient has an Angle’s class III molar relation with spacing in relation to lower anteriors and anterior crossbite on the basis of which, a provisional diagnosis of Angle’s class III malocclusion was made and the patient was referred to the Department of Orthodontics for the correction of the same. The patient was diagnosed with tongue thrusting habit, the correction of which will help in the management of her malocclusion. So the Department of orthodontics provided her with a habit restrainer.
Arteriovenous malformations are vascular lesions composed of dysmorphic arterial and venous vessels connected directly to one another without an intervening capillary bed.2
AVMs may arise during early fetal development, due to the failure of regression of arteriovenous channels in the primitive retiform plexus.2 The embryologic theory explains the predominance of AVMs in the head and neck region, since the early embryo is composed of mainly cephalic structures.2 The shunting between the high pressure arterial and low pressure venous channels account for the clinical picture and progression of the lesion.3 Most cases are sporadic, but there are a few inherited syndromes such as Cobb syndrome, Parkes-Weber syndrome etc seen along with AVMs whose molecular genetics have been elucidated recently.4 Mutations in RASA 1 gene, GAP gene show associated congenital malformations along with AVMs. A defect in ligands or receptors present on the endothelial cells can lead to the formation of AVMs. Estradiol-17 beta receptors are seen in proliferating conditions of AVMs whereas they are absent in stable or involuting lesions and corticosteroid treatment has been suggested theoretically to block these receptors.
The incidence of AVMs is equal in both sexes.2 About 40-60% of lesions are visible at birth. 30% of AVMs become clinically apparent during childhood.2 The size may increase rapidly secondary to infection, trauma, ligation, and attempted excision or via hormonal influences such as during pregnancy and puberty.1 AVMs may progress through 4 different stages and can be scored by severity using the 1990 ISSVA-accepted Schobinger clinical staging system.1,2,3,5
Stage I (quiescence), Stage II (expansion), Stage III (destructive), Stage IV (decompensation).
Stage I lesions: Asymptomatic having the appearance of a port-wine stain on involuting Hemangioma. They are present from birth until adulthood. The presence of a thrill, a bruit or increased warmth may suggest a high flow component in the AVM. Some AVMs may remain in this stage throughout the patient’s life.
Stage II lesion: This phase begins during adulthood. It represents expansion and invasion of deep structures. Progressive dilatation, thinning and fibrosis of arteries and veins are seen histologically. On clinical examination, local temperature is increased and on palpation, a pulse or a thrill can be felt. A murmur may be heard on auscultation.
Stage III lesion: Grossly it mimics stage II. Here involvement of deep destruction occurs with spontaneous necrosis, pain, chronic ulceration and hemorrhage. This stage is seen after years of progressive worsening.
Stage IV lesion: Characterized by cardiac decompensation and high output failure. High output cardiac failure may result from increased blood flow in large AVMs.
Calcifications on OPG are rare. Phlebolith is uaually associated with low flow vascular lesions and was first described by Kirmission in 1905. They appear as multiple round radiopaque masses with smooth periphery and concentric rings giving it a laminated or bulls eye appearance. They are usually visible ob the ramus region on OPG.8,9 They have to be differentiated from other radiopacities such as sialolith, atheromas and calcified lymphnodes.10
Arteriovenous malformations are diagnosed by clinical findings and radiologic features.3 In high flow vascular malformations, plain radiography and computed tomography scans have a limited role as diagnostic aid. The diagnosis is usually made with Doppler ultrasonography.3 Magnetic resonance imaging which has become the investigation of choice since it depicts the extent of invasion of the lesions, providing multiplanar images and differentiating between high and low flow lesions. Existence of flow voids on MRI helps to confirm a fast flow vessel. Angiography is useful in poorly defined cases and for embolization before surgery.4 It demonstrates the major feeding vessels, flow characteristics of AVM and anastomoses.4 Typical angiographic findings are striking hypertrophy and tortuosity of feeding vessels. The nidus (centre) of lesion may differ from large tortuous vessels to innumerable small vessels appearing as an intense blush. Collateral vessels typically have a ‘corkscrew’ appearance. When contrast is used, parenchymal staining is generally present.1
If an AVM is asymptomatic, no treatment is necessary. Therapy becomes necessary with complications such as pain, ulceration, and bleeding or heart failure.7 Management of AVMs usually requires multimodal treatment including preoperative embolization and complete surgical resection. Various sclerosing agents (sodium morrhuate, boiling water, nitrogen mustard, 1% sodium tetradecyl sulfate etc) have been used to treat these high flow lesions but have proven ineffective because they were displaced from their site of action by speed of the blood flow.7 High power lasers have an excellent therapeutic option for this type of lesion in the oral cavity.5 Their coagulative properties allow procedures to be done without the risk bleeding, which promotes a better healing pattern. For AVMs not amenable to surgery, superselective arterial or retrograde venous embolization is used as a first choice of treatment.1 Different materials used for embolization include Polyvinyl Alcohol particles, gel foam, coils, and methyl methylacrylate and silicon spheres.11
Arteriovenous malformations are defects in vasculature with abnormal connection between arteries and veins. A rare case of multiple arteriovenous malformations of tongue and lips in a 32 year old female has been presented. It has been emphasized that the management of these cases requires a multidisciplinary approach. Laser therapy, embolization followed by surgical excision is the favorable treatment modalities.
None.
None.

©2018 Halim, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.