Journal of
eISSN: 2379-6359


Concussion (mTBI) diagnostics and management are some of the most commonly discussed topics in the healthcare setting for children, adolescents, and adults. Currently, there is no “gold standard” for the assessment and management of concussion patients; however, research is emerging in the field. We present a case report of a 70-year-old male suffering from both cortical and labyrinthine aspects of concussion. We utilized our protocol, The American Institute of Balance – Vestibular Cognitive Integration (AIB-VCI) for assessment and management of both the cortical and labyrinthine aspects of the patient’s concussion. This was met with great success; namely, the patient was performing at his target vestibular and cognitive levels in a timely manner post-concussion. The literature is abundant with information regarding patients with similar symptoms that do not recover as rapidly, or decline in vestibular and cognitive performance (McCrory et al., 2012). This suggests that the AIB-VCI may be a useful assessment and management strategy for patients suffering from vestibular and labyrinthine concussion.
Keywords: concussion, cortical, labyrinth, vestibular, cognitive, mtbi, balance, vertigo, memory
mTBI, mild traumatic brain injury; AIB, the american institute of balance; VCI, vestibular cognitive integration; PC-BPPV, posterior canal benign paroxysmal positional vertigo; GSOP, gans sensory organizational performance test; VR, vestibular rehabilitation; BPM, beats per minute; NAB, neuropsychological assessment battery; HVLT, hopkins verbal learning task; SDMT, symbol-digit modalities task
Concussion (mTBI) is one of the most commonly discussed and emerging healthcare issues for children, adolescents, adults, and the elderly. For younger individuals, concussion is mostly related to sports induced trauma. According to The American Academy of Neurology (2013), female adolescent football (American soccer) players are the most likely sports participants to suffer a concussion. In the elderly population, mTBI is a significant result of head trauma post-fall. The National Institutes of Health reported that falls and subsequent mTBI in the United States account for over 1.8 million emergency room visits (2015).
Head trauma, direct or indirect through sports, falls or motor vehicle accidents may produce cortical concussions, labyrinthine concussions, or both.
At The American Institute of Balance, this dichotomy between the two potential aspects of concussion is of utmost importance. This is due to the fact that concussion patients can make little to no progress, or worse yet, regress in their abilities without proper attention to therapeutic regime. Also, the breadth of symptoms that patients experience need to be differentiated as a patient with a cortical concussion that complains of dizziness will require different management than a patient with a labyrinthine concussion who also reports dizziness.
Cortical involvement may influence:
Labyrinthine involvement may influence:
For the appropriate diagnostic and treatment triage of concussion patients, as well as the important aspects of return to play or activity (RTP/A) decisions, it is beneficial to ask the right diagnostic questions based on intake, then to use the best practice approach to an evidence based continuum of care. We present the following case study as an example of the AIB Concussion protocol.
A 70-year-old male was seen at our facility for concussion evaluation. He reported falling on his left side and then his back while gardening 1week ago. No direct head impact was encountered; however, he remarks of indirect jarring of his head and neck. Immediately after falling, he reported an episode of true vertigo lasting for 4hours. This vertigo was experienced regardless of position or head and body movement. Currently, he states that this constant vertigo has subsided. However, he now experiences dysequilibrium while ambulating on dynamic surfaces as well as when ambulating with active head rotation. Post vertiginous episode, the patient noticed dizziness and vertigo when laying on his left side at night as well as with vertical head pitch. This has continued to present. The patient went to the ER after falling and head imaging studies were completed. No remarkable findings were noted. The patient also notices difficulties calculating amounts to pay on his bills and remembering daily tasks. These cognitive symptoms began following the fall he experienced.
Vestibular assessment
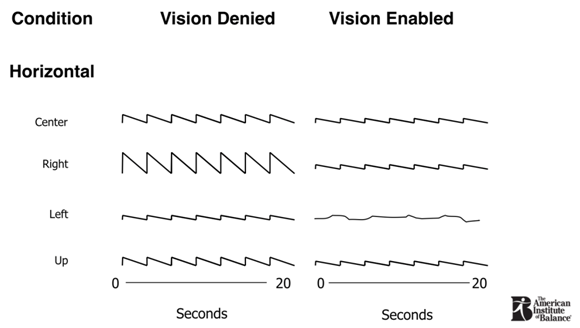
Figure 1 Gaze testing evidenced right-beating nystagmus with all eye deviations. Vision enabled conditions evidenced suppression of nystagmus. These findings are commensurate with an uncompensated left peripheral vestibulopathy.
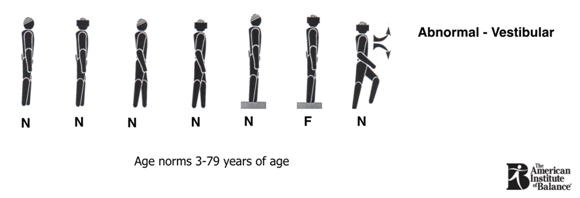
Figure 2 Gans SOP test results are normal in conditions 1-5 and 7 with a fall (denoted as “F”) in condition 6. This pattern is remarkable for an uncompensated peripheral vestibulopathy.
AIB - Vestibular Cognitive Integration Assessment and Management Tools and Scores
Management strategy
Management protocol (Figure 3)
(Figure 4) Other exercises based on the patient’s vestibular and cognitive complaints and deficits included:
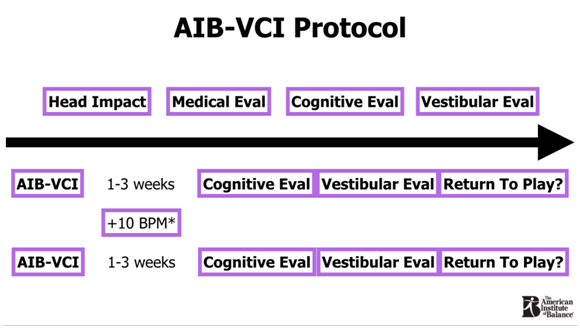
Figure 3 Our protocol consists of a combination of vestibular rehabilitation exercises and cognitive training exercises. The former consists of adaptation, habituation, gaze stabilization, and substitution based on the patient’s symptoms and test findings; the latter consists of training material that relates to the cognitive tests that show deficit (see Figure 2 for an example). Note: it was deemed unnecessary to include heart rate elevation with this patient as he was not medically stable enough to complete the tasks due to recent cardiovascular events unrelated to the current concussion.

Figure 4 One of the selected exercises for the patient based on his vestibular complaints of oscillopsia with active head rotation and body movements as well as his cognitive complaints of digit memory. During this exercise the patient would make a circle pattern of movement with his body and head while focusing on a ball with a cue card attached, or with the cue card alone, in addition to performing a forward/backward digit memory task.
Each of the aforementioned contain both vestibular and cognitive tasks. All of the exercises were completed 3-5days per week for one hour per session. After 1-3weeks, the patient’s vestibular and cognitive performances were measured.
First Follow-up
Vestibular assessment
Cognitive assessment
Updated management strategy:
Head circles and visual tracking to be done on less dynamic surfaces and/or for shorter duration (Figure 5)
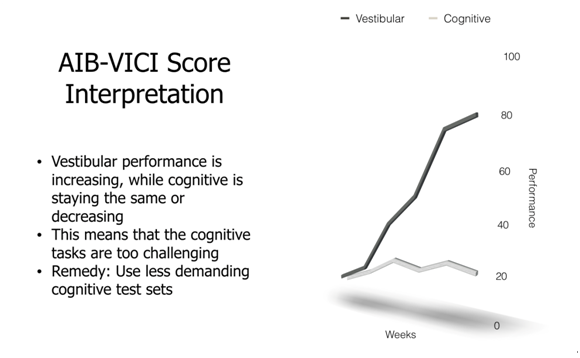
Figure 5 The graph depicts the relationship between vestibular and cognitive performance. In this case, the patient is making progress with vestibular compensation but not with cognitive performance. Unlike the increased intensity needed for vestibular therapy, cognitive therapy can be negatively influenced by too demanding of tasks. As such, the remedy is to decrease the intensity of the cognitive tasks.
Second Follow-up
Vestibular assessment
Cognitive assessment
Updated management strategy
Third Follow-up
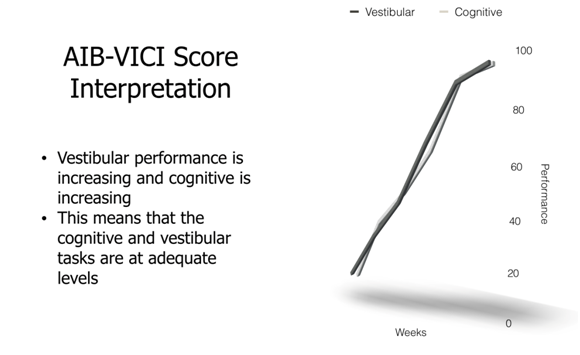
Figure 6 This graph illustrates the intended results of the AIB-VCI. The patient has centrally compensated for the unilateral peripheral vbestibulopathy and has reached his age-corrected normative cognitive scores. Thus, the patient has been successfully rehabilitated for his cortical and labyrinthine aspects of the concussion.
The AIB-VCI protocol is effective because it uses well-established tenants of concussion rehabilitation for both cortical and labyrinthine concussions. Experts agree that demanding rehabilitation sessions can lead to a lack of progress being made for cognitive function.1 However, this is not the consensus on vestibular rehabilitation, where the opposite is true: the more demanding the rehabilitation session, the better, and faster, the positive outcome.2 We now have a dichotic problem that has, for the most part, traditionally been managed with a single strategy, be it complete rest, or intense intervention, both are likely to fail. The AIB-VCI can differentially adjust for difficulty of training sessions on two levels. Namely, vestibular task difficulty and cognitive task difficulty. Thus, we can compensate for a patient who may need less demanding cognitive training but more intense vestibular training, while still making progress in both areas. The risk of not differentiating the diagnosis and management of labyrinthine from cortical concussion can go beyond a lack of progress being made. Too intense, or too time-consuming, cognitive load can create a cascade of events in the central nervous system that lead to neuronal cell death.3 Tau protein and increased ventricle size then take up the space where neurons were once present and the patient is left with a permanent neurological change. If this keeps happening with either repeated head trauma or a lack of adequate cognitive rest, a condition called Chronic Traumatic Encephalopathy (CTE) develops.4 This leads to permanent structural and functional changes, including diminished cognitive performance beyond that of the head impact itself.3,4 As such, having a management strategy that allows for constant modification of vestibular and cognitive training independently, while still completing both tasks in a timely manner, is of utmost importance. The AIB-VCI was designed for this purpose.
Future studies may seek to assess the ongoing progress of patients after having completed the AIB-VCI protocol. This will help determine the need for maintenance schedules and cognitive plasticity post treatment. In addition, specific symptoms may be targeted and measured over time. One of the most common for concussion patients is a headache. It is unclear how the AIB-VCI protocol impacts specific symptoms such as this over the long term.
None.
Author declares there are no conflicts of interest.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.