Journal of
eISSN: 2379-6359


A new challenge to the medical community is presented with Levamisole, an antihelmintic immunomodulatory agent, recently used in combination with cocaine to enhance its psychoactive effects. The prevalence of cocaine induced vasculopathy is increasing and physicians need to be aware of this emerging condition due to its serious possible complications. We report a case of intermittent purpuric skin lesions located in the auricles in a patient with regular cocaine consumption and a review of this distinctive clinical syndrome described linked to levamisole-adultered cocaine.
A high index of suspicion should be kept in mind if this is considered a potential cause for purpuric intermittent lesions in cocaine abusers. To aid the diagnosis a punch biopsy associated with an extensive workup including immunologic testing is recommended. There are several clinical and laboratory findings that support a diagnosis of Levamisole induced vasculitis, including ANCA positivity, specific anti-HNE antibodies and auricle involvement, that help distinguish this condition from autoimmune vasculitis. Regardless, no optimal treatment has been described, steroids have been used preventing progressive damage but complete withdrawal is indispensable.
Keywords: auricle, cocaine, levamisole, purpuric lesions, vasculopathy
ANCA, antineutrophil cytoplasmic antibodies; Anti-HNE Antibodies, anti-hydroxynonenal antibodies; HIV, human immunodeficiency virus; ANA, antinuclear antibodies; c-PAN, cutaneous polyarteritis nodosa; LIVEN, levamisole-induced vasculopathy; HNE-ANCA, human neutrophil elastase-ANCA
Levamisole is an immunomodulatory and anti-helmintic drug, used to treat parasitic infections and inflammatory autoimmune conditions.1‒3 Recently, it has been used illegally as a cutting agent in cocaine to enhance its euphoric properties.2 The cutaneous lesions following adultered-cocaine consumption include a distinctive vasculopathic purpura, microvascular thrombosis and leukocytoclasia. The effects of this drug may be very severe and they need a high clinical suspicion for it to be detected and avoided on time.
A 52year old man with HIV and Hepatitis C, presented to our consult with a 2year history of intermittent purpuric skin lesions in both ear auricles and a small one in his lower left limb. They occurred every time he snorted cocaine, and disappeared a couple of days later. It has worsened along the years regarding extension and recently a small permanent ulceration in his left helix has appeared reason why he consulted (Figure 1).

Figure 1 Right (A) and Left (B) auricle showing purpuric disseminated lesions. Notice the small necrotic area in the upper part of the left helix.
Physical examination revealed a non-toxic-appearing man with painless purpuric lesions with bilateral helical involvement, one with a small necrotic area. Besides also having a perforated nasal septum there were no other clinical findings. Since he had consumed the day before and the lesions appeared the next day, some tests were performed immediately including urine toxicology, showing positive cocaine metabolites. Laboratories also revealed a normal hemogram and an elevated erythrocyte sedimentation rate.
Histopathology of a punch biopsy, performed a couple of days later, revealed diffuse presence of thrombi in the superficial and deep dermal blood vessels with a neutrophilic perivascular infiltrate with leukocytoclasia and extravasation of red blood cells. No epidermal necrosis was observed (Figure 2). Immunology showed positive anti-cardiolipin, P-ANCA and ANAs. His viral load and CD4+ T-cell counts were stable compared with previous. Internists that evaluated him excluded systemic involvement. Treatment involved a complete withdrawal, which at this time during follow-up has not been accomplished by our patient.
Levamisole-adulterated cocaine induced vasculitis is a condition with increasing prevalence in the last decade due to its illegal use as a cutting agent.1,4‒6 Cocaine is the illicit drug most frequently reported in the emergency department of the United States of America. It is believed that the percentage of levamisole adulterated cocaine has risen to approximately 82% in the USA and Europe.3,4,7 Because of its physical properties it blends easily with cocaine.
Studies have suggested that the enhancing of stimulating, addictive and euphoric properties of cocaine is due to its effect on dopamine release.3‒5 Negative testing does not rule out the presence of levamisole or its causative role in the signs of this type of vasculitis, due to its short half life as happens without patient, who has negative laboratory findings.4,8,9
Cases have been described in the 70´s when this drug was used, due to its immunomodulatory properties, to treat cancer, rheumatoid arthritis and nephrotic syndrome,4,6,9 in which purpuric lesions appeared beginning the treatment and disappeared with withdrawal. With re-exposure, progression and worsening of the lesions was observed. If consumption is not withdrawn on time, skin ulceration and extent necrosis may result being exceedingly painful and requiring hospital admission with special wound care.1‒3 The small necrotic area in the left helix was still painless. Surgical interventions are similar to the ones used in burnt lesions. In some cases wound care is not enough and serial debridement and skin grafts may be required.8,10 Bilateral helix involvement is seen in numerous cases, being the most “pathognomonic” site, but if this condition is not known, suspicion of this possible etiology may pass unnoticed.3,7 Our patient referred cocaine consumption during his interrogatory. Systemic vasculitis rarely involves the ears.10 Some characteristics of the clinical syndrome may easily confuse with true vasculitic diseases such as Churg-Strauss syndrome, cutaneous polyarteritis nodosa (c-PAN) and Wegener syndrome. Systemic involvement was ruled out in our case.
The pathogenesis of this condition is unclear. Cocaine by itself causes intense vasoconstriction which enhances platelet aggregation decreases fibrinolytic activity and activates immunologic mechanisms with consequent vasculopathic effects.7,10 Histopathological features of LIVEN (Levamisole-induced vasculopathy) are occlusive thrombotic vasculopathy with or without leukocytoclastic vasculitis and fibrinoid necrosis.2,4,6 Thrombotic vasculopathy features are characterized by eosinophilic PAS positive deposits in the luminal vessels as can be observed in our Figure 2. Lesions are characterized by being retiform and purpuric with occasional necrotic patches with perivascular lymphocytic infiltrates and ANCA positivity.5,7,9 Characteristic histologic patterns make biopsy very useful in narrowing diagnostic possibilities.9
This condition has a strong association with P-ANCA (HNE-ANCA: Human Neutrophil Elastase-ANCA specific for autoimmunity induced by cocaine) anticardiolipin and lupus anticoagulant antibodies.1,2,5‒8,10 In a literature review performed by Pearson et al. HNE-ANCA showed positive results in 100% of the cases analyzed.7 After exposure to levamisole, antibodies normalize within 2-14months after discontinuation. This entity is usually also accompanied by neutropenia and agranulocytosis (Figure 3).
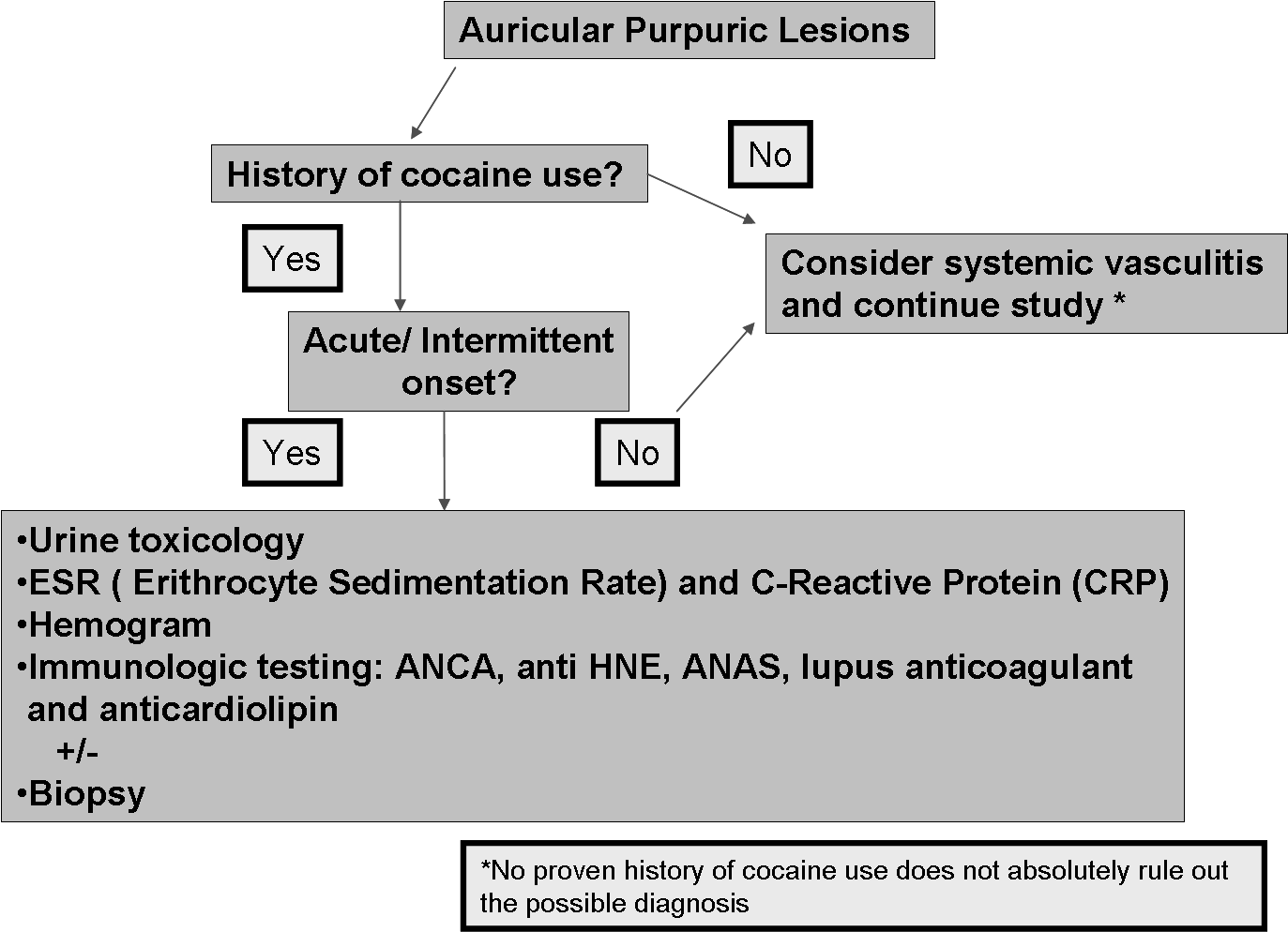
Figure 3 We present a diagnostic algorithm for Auricular Purpuric lesions including: Urine toxicology, ESR: Erythrocyte Sedimentation Rate; CRP: C - Reactive Protein; Hemogram; Immunologic Testing; ANCA; Antineutrophil Cytoplasmic Antibodies; Anti-HNE Antibodies: Anti-Hydroxynonenal Antibodies; ANA: Antinuclear Antibodies; Lupus Anticoagulant and Anticardiolipin, and Biopsy.
Steroids have shown unclear benefits. They are usually indicated in extensive lesions to prevent complications such as necrosis.4,5 But there is no firm evidence that systemic steroids are indicated.10Immunosupresors are used sometimes to maintain remission but in our patient due to his medical history this was not considered. The only effective treatment is withdrawal.2
The increasing number of cases of vasculitis induced by levamisole-contaminated cocaine represents a diagnosis that must be known by every physician. A high clinical suspicion is required to correctly diagnose this entity associated with an appropriate laboratory workup along with histopathologic confirmation of the diagnosis. Serious possible consequences, should aware clinicians to be able to recognize the characteristic features usually involving ears, face and lower limbs associated to this condition.
None.
Author declareas there are no conflicts of interest.
None.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.