Journal of
eISSN: 2373-437X


Research Article Volume 11 Issue 4
Genetics and Genomics Consultant - Molecular biologist PhD, Uruguay
Correspondence: Juan Martín Marqués, Genetics and Genomics Consultant -Molecular biologist PhD, Uruguay
Received: September 05, 2023 | Published: September 15, 2023
Citation: Marqués JM. Loss of control of the pandemic during vaccination in Uruguay. J Microbiol Exp. 2023;11(4):98-105. DOI: 10.15406/jmen.2023.11.00396
In countries where lockdown was not strictly enforced during vaccination and the vaccination rate was near 1% of the population per day, a loss of control or a multiplying effect in virus spread was observed when the vaccination program was implemented. Particularly, in Uruguay between March and June 2021, there was a clear link between the vaccination rate and the number of positive cases of SARS-CoV-2 observed each day. The peaks in the vaccination rate by day were followed by peaks in positive cases with an 8-day lag. Typically, 10% to 20% non-detected positive cases are considered superspreaders due to their high viral load despite experiencing mild or no symptoms. These superspreaders or undetected positive cases were responsible for 80% of the virus's spread. The data we got access to allow us to define a cohort study for whole individuals being vaccinated during 5 consecutive days during March 2021 when vaccination starts. In this cohort there was a 75% reduction in tested positive cases in vaccinated individuals compared to what was expected. We have some extra data that suggest these number were maintained during the 4 months with high vaccination rate. We propose that this reduction is due to individuals they thought they were experiencing side effects from the vaccine and were not tested, but in fact they had COVID. These non-tested positives individuals, representing nearly 5% of positive cases per day, may have unknowingly become superspreaders, increasing the odds ratio to be infected during vaccination by 1.20x to 1.4x compared to a non-vaccination situation with same control measures applied. Previously, Uruguay had been considered one of the first countries in the world in pandemic management for a year without vaccination, with a particular health politic: “responsible freedom”. However, during a period of four months with high vaccination rate in 2021, the country exhibited the worst levels of disease Worldwide, applying the same politic.
Uruguay is a small country with a small population, particularly, with a significant number of professionals trained in real-time PCR, the technique that became the star in the diagnosis and prevention of COVID. Detecting symptoms and diagnosis was the main weapon for prevention, once positive SARS-CoV-2 cases were detected, a tracking procedure was established and those who had been in contact with positive patients were isolated and tested. Positive individuals were isolated since the onset of symptoms and were instructed to quarantine for 14 days upon confirmation of the diagnosis via testing. In addition, an Honorary Scientific Advisory Group (GACH) that provided advice to the government on how to best deal with the pandemic was formed, and Uruguay’s management of the pandemic received worldwide recognition in 2020, including Uruguayan virologist Gonzalo Moratorio being ranked between the Nature’s 10 in 2020.1 After the first case of coronavirus was detected in Uruguay, the government responded by not authorizing large gatherings, establishing the necessity of closing businesses and schools, and advising the population practice physical distancing, use masks, and take other known preventative measures, an approach that had a positive effect to contain the spread of the pandemic. Later in 2020, with the advice of the GACH, the government decided on the implementation of a “responsible freedom” policy, by which schools and businesses would resume their activities, but with physical distancing and the use of masks.2 During 2020, Uruguay managed to have very few positive cases despite having a river border with Argentina and a dry border with free transit with Brazil, and it made it the country with the lowest level of COVID cases worldwide for almost a year, from March 2020 to February 2021, even though its neighboring countries did not do as well, possibly due to differences in the policies enacted and the health care systems in place, as well as cultural differences.
In March 2021, two and a half months after vaccination had started in other regions, the vaccination process began in Uruguay; and once it did, it did so with great speed. By July of that year, Uruguay was one of the countries with the highest vaccination rate in the world. At the same time, during that period, Uruguay experienced the worst consequences of the pandemic, becoming the country with the highest mortality rates from COVID worldwide during 80 consecutive days.
Some important points to consider during March-June 2021 period are:
Other factors that could make Uruguay a good model country to observe a marked effect are: a good level of molecular biology testing within the population, with short turnaround times, a very good and uniform historical vaccination plan around the country, with which people have always complied in a significant way, and a small population and surface.
During the SARS-CoV-2 pandemic virus, some individuals with high loads of virus copies who were asymptomatic or presented mild symptoms were not detected among the population, and due to their behavior or attendance to social events, they became superspreaders.3 In general, some individuals infect many people, but most infect only a few, a phenomenon that has been seen for other viruses as well.4 It has been shown that superspreaders are usually nonelderly individuals, under the age of 60.5 These superspreaders are initially not detected as positive cases and they can represent from 10 to 20% of positive cases, depending on the level of surveillance in place, but in any case, their control and surveillance are the clue to maintaining low levels of the virus spread.6,7 Superspreaders are responsible for 80% of secondary infections, so they essentially are the drivers of virus spread.8
To illustrate the effect of the increase of positive cases during vaccination or the loss of control, we examined the association between the daily number of vaccinations and the daily number of positive cases. Our hypothesis was that there exists a loss of control of the pandemic associated with vaccination, and if present, it should be detectable in the distribution data of recently vaccinated people and positive for SARS-CoV-2. After analyzing a small dataset of positive cases just following vaccination during this period in aleatory days every month, we found an absence of positive cases during the first 4-5 days after vaccination along the four months of high vaccination rate as the more remarkable feature. We modeled the expected number of positive cases in recently vaccinated people. Using data from a request of public information to the Uruguayan Minister of Health and the described model for expected positive cases, we conducted a cohort study to quantify the absence of positive cases in individuals just vaccinated. When combined with the percentage of described superspreaders, the new non detected positive cases can constitute an important increase and so being behind of such an uncontrolled increased of positive cases. Our argument is that superspreaders emerged from individuals who confused COVID symptoms with symptoms of vaccination and then were not tested, which may be considered an intuitive and natural behavior and compatible with the new policy of the health system during vaccination. However, to our knowledge, this phenomenon has not been given the importance it deserves. We will show how critical this loss of control has been in the spread of the virus.
Open data from World Data was used to generate the curves representing positive cases per day and vaccines administered per day on Figures 1&2.
Figure 3 was extracted and modified from a Uruguayan report and illustrates the correlation between mobility tendencies and R.9
Vaccinated individuals and rate of vaccinated population were evaluated for Figures 4 and 5. Data from vaccinated individuals was obtained from SINAE and World Data. Data from the whole Uruguayan vaccinated population were obtained already stratified per day, age and type of vaccine. Vaccination in Uruguay started with a rate of 0.5-1% of the population and then, it continued with a rate of 1-1.8% per day (World data). On Sundays there were no vaccination except for one Sunday in April, 18th April one day before a national date.
The data corresponding to total positive cases per day, per age and per type of vaccine received, for the whole Uruguayan population were provided to us by the Ministry of Health in response to our request for information. There were provided without discrimination of the day of vaccination, that’s mean that all people vaccinated with Sinovac for example enter the group S, and if there was a positive in this group was reported as been on the group without knowing in which day he received the vaccine but we knew the day which became positive.
For the first 5 days of vaccination with Sinovac from 1st to 5th March, over 2% of the Uruguayan population was evaluated. More than 72,203 individuals were administered Sinovac vaccines and about 40,442 healthcare workers between 20 and 60 years old were administered Pfizer vaccines during 12th-15th March. These number are analyzed on Figure 5A and 5B. These two group with higher incidence than general population were not corrected by their real incidence, so the expected cases are underestimated in these two cases.
For a third and fourth analysis for the non-detected positives, on the second week of vaccination with Sinovac (starting 8th March) 80,140 individuals between 55 and 64 years old were vaccinated, and 41,548 individuals over 75 years old were administered Pfizer vaccines in a five-day period starting 22th March 2021 (second week of vaccination with Pfizer vaccine). So these two groups well delimited in time can be analyzed in similar ways that the first two groups: expected positive cases for the fraction of population being vaccinated corrected by the incidence on these two groups (these two incidences are lower than general population10)minus observed positive cases for this population (we have this group age discriminated in the data provided by the Minister of Health supplementary data), what allow us to determine the percentage of people not being detected as positives.
All SARS-CoV-2 tests reported to the Minister of Health at these times were qPCR test or Real Time PCR.
Figure 1 shows how an increase in positive cases was controlled in December 2020 through the implementation of certain policies, such as a slight restriction of mobility as can be seen in Figure 3 (orange curve), but the “responsible freedom” measures were maintained. When vaccination started in March 2021 and there was a rapid increase in positive cases, CAGH advised strengthening the measures to contain the spread of the virus, but the government decided to continue with the “responsible freedom” policy that had been succeed up to that moment.
What can be seen when observing Uruguay’s situation is that there is a positive correlation between the rate of vaccination and the positive cases detected (Figures 1&2). There is a correlation on 2 levels:

Figure 1 Vaccination rate and positive cases in Uruguay from 11/1/2020 to 06/15/2021. Uruguay started vaccination on 03/01/2021.

Figure 2 Vaccination rate and positive cases in Uruguay from 02/20/2020 to 06/15/2021 (amplification of Fig 1). Uruguay started vaccination on 03/01/2021. The x component of the arrows represents a 7-10-day long delay. The asterisk shows a particular Sunday in which 15,000 doses of vaccines were administered and it translated as an insignificant decrease in positive cases 8 days later, comparable to what had been observed other Sundays with no vaccination. Uruguay has a population of 3,470,000 inhabitants.
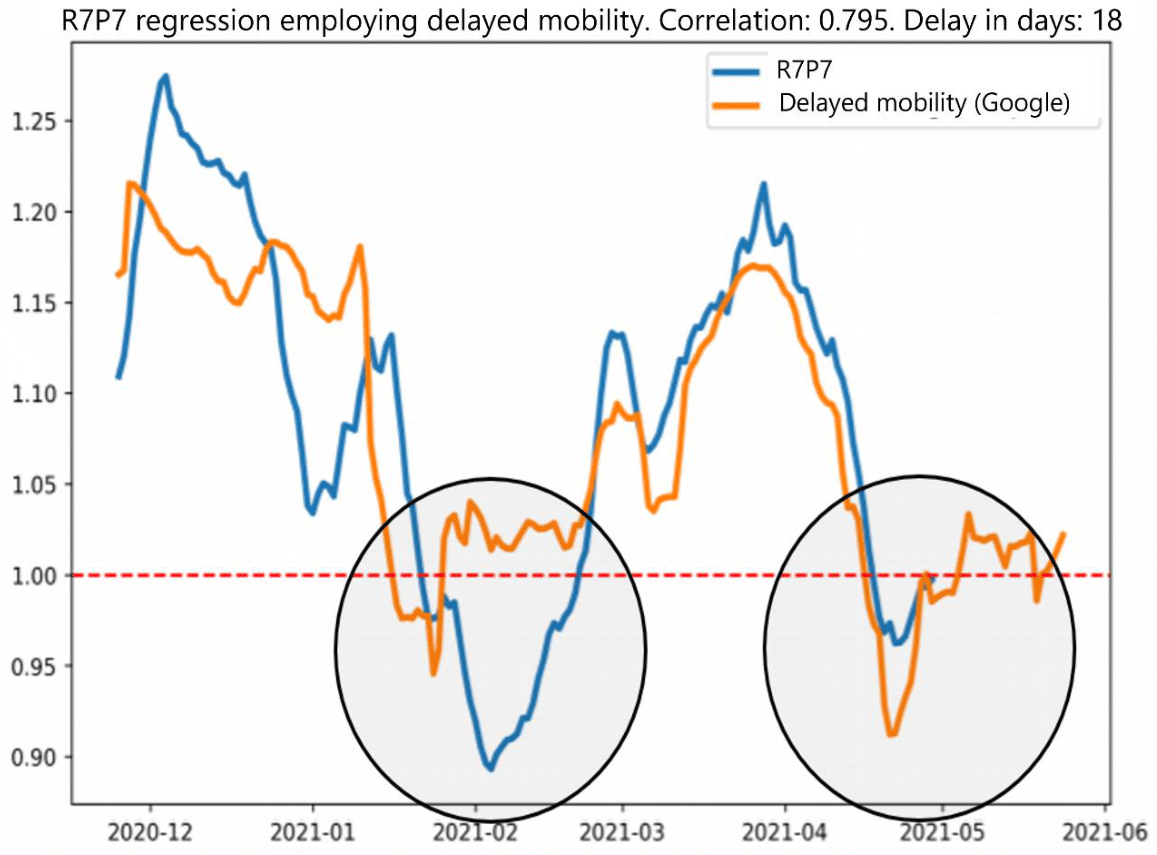
Figure 3 Correlation between mobility tendencies and R7P7 (extracted and modified from.13) Two circles were added to the original figure to highlight the difference in R7P7 between February and April (blue curve inside de circles), and such difference cannot be explained by mobility, which was very similar in both periods (orange curve is Google mobility).
A similar effect was observed in other countries, even though, not as much on a detailed level, such as in Uruguay’s situation, but with a positive correlation on the magnitude level, see Chile and Israel, and on Kerala state in India, that started massive vaccination earlier than the rest of the country and had worst results during vaccination (an interesting example of a control group within the country). When considering these situations in other different countries, the effects of lockdown must be taken into account, and when adding other factors, it is harder to visualize the effect on a macro level. However, this correlation on a magnitude level between vaccination rate and positive cases can be seen in other countries (Colombia, Malaysia, Thailand, Georgia, and others can be seen using the JHU dashboard, see Annex 1).
Mobility is a necessary factor to see the effect of vaccination on a macro level. The increase of positive cases stopped when mobility diminished in mid-April in Uruguay (Figure 3), as it had happened in December but with better results because positive cases decreased. At that moment it is possible to observe a continued positive correlation between vaccination and positive cases when observing the situation on a detailed level, maintaining high numbers of positivity during April-June (Figure 2). By mid-April, there was another factor to be considered, the number of people protected by the vaccines, albeit still not large, started to grow, but the positive cases did not diminish as expected for both factors. So, it could be surmised that another factor would be needed to maintain high levels of positive cases at this plateau in the same population where this measure had been successful three months before. I postulated that this multiplying factor or loss of control came from the vaccination events, after which the positive cases grow in such a high magnitude at the beginning and it was the force that maintained a high number of cases for 3 months in this plateau. During the April-June period, Uruguay was the worst country in the world, with over 650/1.000.000 inhab positive cases for 80 days, while being one of the top countries in terms of vaccination rate worldwide from March to June, it started vaccination on March 1 and it was the first country in the world in vaccinated inhabitants rate by late July – clearly due to the vaccination speed, which is related to the excellent vaccination plan in place in Uruguay for quite some time.
Based on data from positive cases who were recently vaccinated we detected an absence of positive cases as a primary observation the days immediately following vaccination. Thereafter, we modeled the evolution of expected positive cases in the population just vaccinated to try to quantify the number of the absent positive cases in data provided by the Uruguayan Ministry of Health in response to our request for information (Figure 4).
Several assumptions are needed to model the expected accumulated number of positive cases, as well as the number of potential superspreaders generated if there are non-detected positive cases. In general, a fraction of just vaccinated people already infected will first present symptoms of COVID on the day of vaccination or the first, second, or third day following vaccination (arrows with a small orange oval in the upper part of Figure 4). These people were infected before vaccination and during incubation period there were vaccinated. So if the incidence did not change for these people before vaccination it will not change after. Detection of these cases would be expected after the conduction of PCR assays, which can take one day. During this period, people are supposed to be isolated and waiting for the test result; however, in the case of people who are not tested, they will not comply with the isolation and will continue with their daily life as usual (going to work, practicing sports, among other activities), while they can be contagious for at least 4 days from the onset of the first symptoms (in fact, they could be contagious for between 5 and 7 days11 (solid orange circles in Figure 4). So, at a fixed day 0 (which could be any day after day 4th of vaccination but in our case coincide, below scale), we evaluate the total number of possible contagious people by adding cases that in a normal situation should have their first symptoms this day 0 (we quantified its absence the following day), and we add to these cases the non-detected cases accumulated to date which can be supposed to still be contagious due to day 0 being within the aforementioned 4-day period of contagiousness (from day-4 to day 0) (red oval in the bottom part of Figure 4).
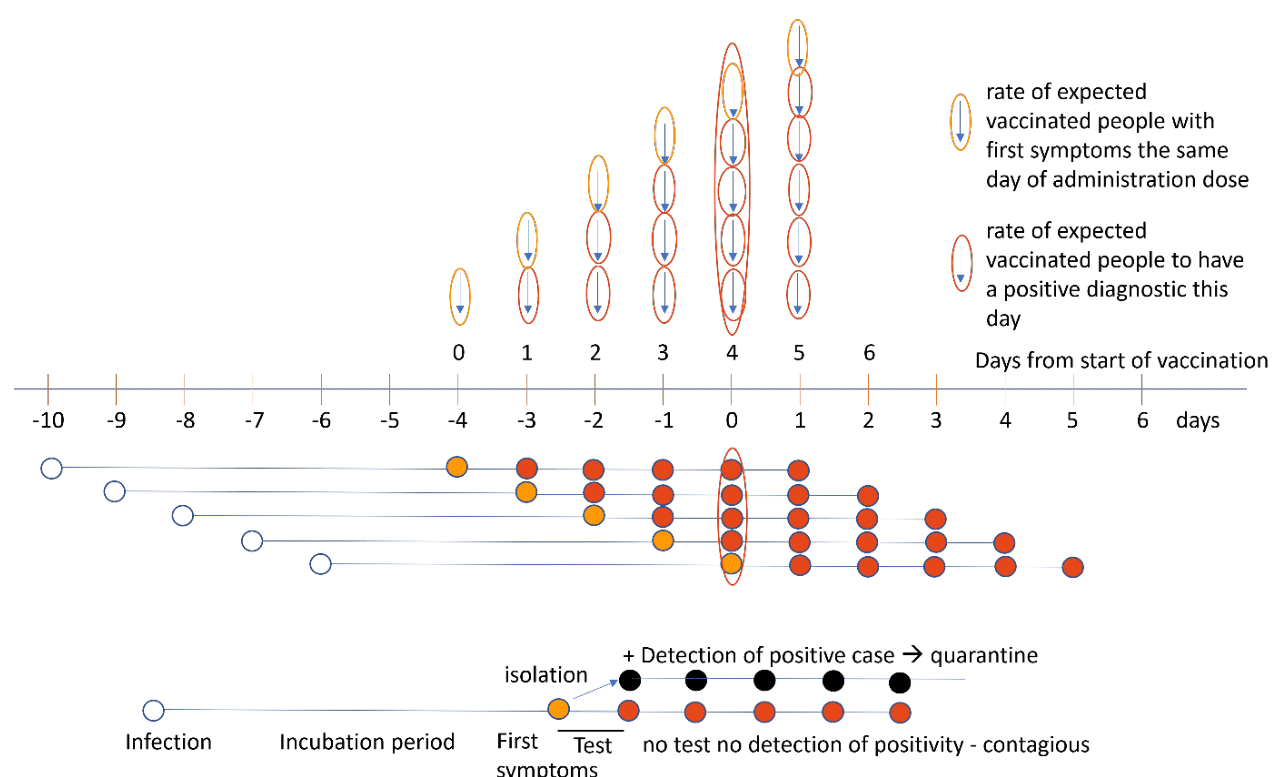
Figure 4 Model to determine the number of expected positive cases in vaccinated individuals infected before receiving the dose (upper panel) and accumulation of non-detected positive cases or potential super spreaders (bottom panel) generated during vaccination in just vaccinated people. Supposing a fixed incubation period of 6 days until the first symptoms (5 or 6 days are acceptable means for the incubation period). Supposing a fixed duration of 1 day for the turnaround time for the PCR diagnostic (the vast majority of PCR results were reported in 24 h during this period), solid orange circles (people with first symptoms) will be transformed into solid red circles if they are not confirmed as positive via means of detection one day after. Supposing people with symptoms on day prior to receiving the vaccination dose will not receive the vaccine dose (so, no expected positive cases for the day of vaccination from people having first symptoms the day before, so no red solid circle the first day of vaccination). Supposing people with symptoms should be tested, isolated until the result, and in case of positivity will be quarantined for 14 days (time frame advised at this stage of the pandemic in Uruguay, solid black circles). We suppose 4 days of contagiousness after the first symptoms, but it is well known that they could be between 5 and 7 days after the onset of symptoms.6 The non-solid red oval below regroups all the possible non-detected accumulated non-detected positives or potential super spreaders.
We have data we could use to investigate the absence of positive tested cases during the days immediately following vaccination only at the beginning of the administration of each type and dose of vaccine (first dose of Sinovac (S) and Pfizer (P), second dose of Sinovac (SS) and Pfizer (PP)). The data we had access to shows the total positive cases per day in vaccinated people discriminated by the type of vaccine, but not discriminated by when people received the vaccine or the number of days elapsed from the date of vaccination, so the data is useful to evaluate the model just for the beginning of vaccination with each vaccine (because we have the date when vaccination started for each type of vaccine and the amount of doses administered each day). If we look during the first 5 days at people with vaccinated status S, in Figure 5A, there is a lower positive rate than the one expected for those vaccinated one day before (with enough time to receive a positive result). This observation is particularly clear after vaccination with Sinovac (initially vaccinating teachers between 20 and 60 years old, and then the general population between 55 and 64 years old). For these just vaccinated people, we would expect at least the same incidence as within the general population. As it can be seen in healthcare workers who had been administered Pfizer vaccines, during the first week there is a coincidence of expected positive cases and reported positive cases showing the model is correct (Figure 5B). Instead of the rates expected for teachers who received Sinovac vaccines, we have 75% less detection (we don’t know the incidence in this special age fraction of the population, but the general population within this age range has an incidence similar to that for health care workers, and both higher than in general population but we didn’t correct for this number,10 if we would do the differences should be greater). This phenomenon can also be observed for the second dose of Sinovac, which started 28 days later. The behavior in young adults seems similar with the first and second doses, but we would expect fewer positive cases in Sinovac vaccinated people with the second dose if the vaccine effectively reduces the incidence nearly 28 days after the first dose, something that was not really clearly address for the first dose of Sinovac vaccine so we couldn’t correct for this factor.
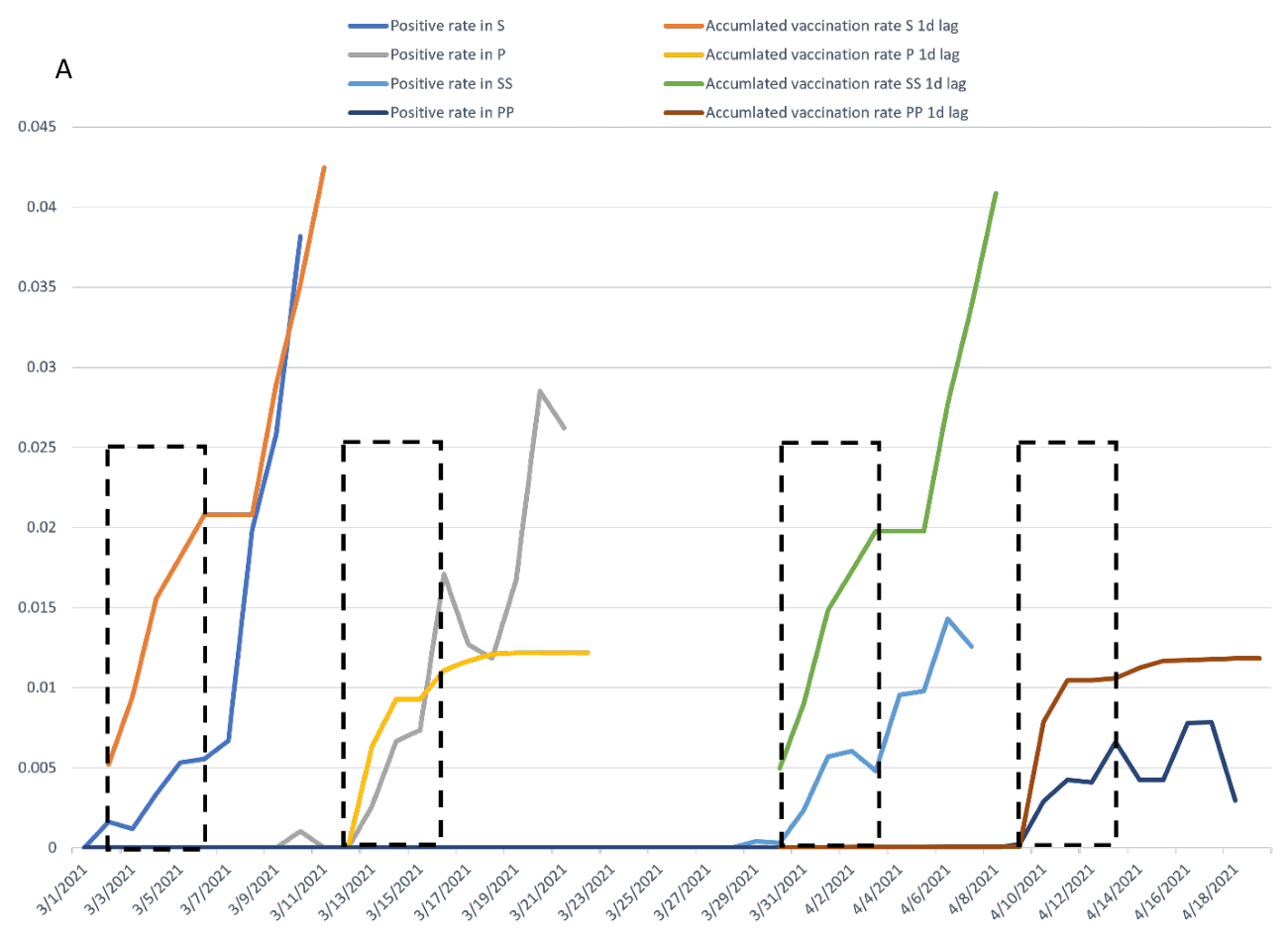
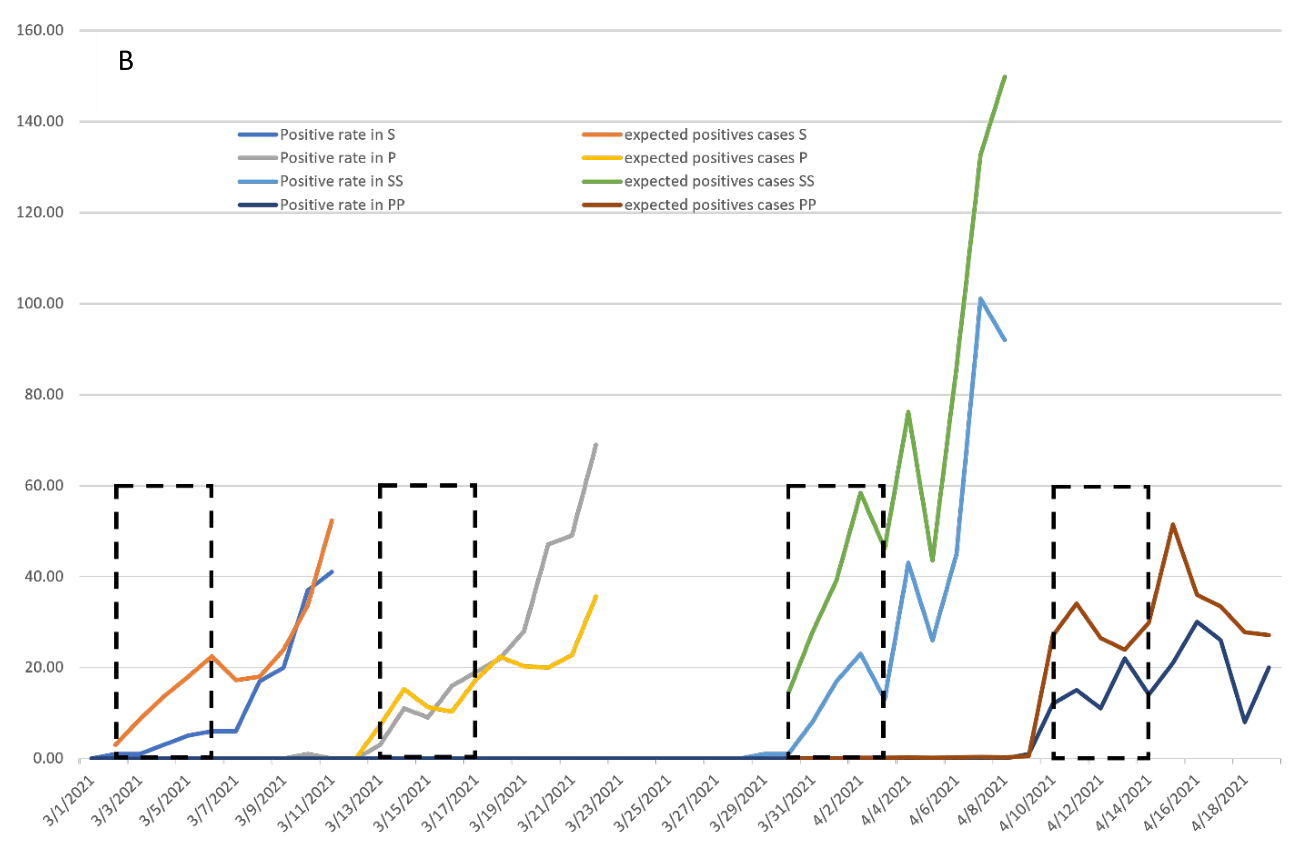
Figure 5 Positive cases as indicated by the Ministry of Health and expected positive cases (calculated applying the model illustrated in Figure 4) for all positive cases among all vaccinated individuals during the first 10 days after the start of vaccination in each group, depending on the type of vaccine and dose received. Figure 5A Positive rates among vaccinated people and accumulated vaccination rate (with a lag phase of one day assuming positive cases are detected one day after testing). Figure 5B Positive cases and expected positive cases for the proportion of accumulated vaccinated people. Group S: people who received a first dose of Sinovac vaccine (teachers were vaccinated during the first week, then general population between 55 and 64 years old); Group P: people who received Pfizer vaccine (healthcare workers first, and after high-risk individuals and people over 70 years); Group SS: people who received the second dose of Sinovac vaccine; Group PP: people who received the second dose of Pfizer vaccine.
Graph B of Figure 5 shows the number of positive cases detected per calendar day discriminated by type of vaccine (data provided by the Ministry of Health) and the expected positive cases per day calculated based on the total vaccinated people to date, the proportion of population they represent and the proportion of positive cases per day. The number of expected positives cases for day 1 after vaccination is calculated as the fraction of people vaccinated on day 0 multiplied by the positive cases informed during day 1. The difference between them and detected positive cases would be the non-detected positive cases or potential superspreaders present from day 0 to day 1. Subsequently, it is possible there are more cases with symptoms appearing on day 1, when there would be vaccinated people from day 0 and vaccinated people from day 1, but these results will be measured on day 2 with respect to real cases detected on day 2, and so on. On day 4, we would have all the possible new non-detected positive cases (calculated on day 5) that could become superspreaders if they don’t realize that they have COVID symptoms on day 4 and they get a test. We can assume that 4 days after being vaccinated, people would not confuse symptoms of COVID with the side effects of vaccination, but we can likewise count them as expected positive cases because they will result in positive cases on day 5 and they will be subtracted. To these non-detected positive cases from day 4, we will add the individuals who become contagious during the first days (represented with a red oval in the model of Figure 4 or by the area between both curves in Figure 5B). For the first event of Sinovac vaccination (S), the number of expected positive cases was 65 during these five days (from March 1 to 5, 2021), but only 16 real positive cases were detected, so 49 individuals corresponding to non-tested positive cases because a loss of control. We assume that a vaccinated individual positive for SARS-CoV-2 and not detected on day 1 will be contagious 4 days after receiving the vaccine, this is why we add the non-detected positive cases on these days, since unless the non-detected cases are detected in the middle of that time frame, which will be reflected in the real positive cases. These 49 new non-detected cases represent nearly 5% of positive cases for this day, and if they became superspreaders it could represent an increase 1.25x in general incidence or 25% increase in the number of superspreaders (taking into account that superspreaders are 20% of total positive cases, but in Uruguayan society this number should be smaller so the representation grater).
In the case of the second dose of Sinovac vaccines, the numbers changed to 62 total detected positive cases with respect to 185 expected positive cases, so the number of possible superspreaders rises to 123, representing nearly 4% of positive cases this day. For this instance of vaccination, the incidence of the second dose in people with one Sinovac vaccine 28 days after the first dose (just at the moment of receiving the second dose) will perhaps be diminished, but we don’t have good information about it, and it is difficult for the model to weigh this and correct the number.
Some more groups can be evaluated, since vaccination with Pfizer vaccines started on the population over 75 years old on March 22. Thus, we can evaluate the expected positive cases for that population and then observe the detected positive cases for individuals on that age range with P status, which results in a 48% of non-detected positive cases from the expected positive cases (we corrected for this population a diminished incidence of 60% with respect to a younger population between 18 and 49 years old). Similarly, it is possible to evaluate the general population over 55 years old receiving Sinovac vaccines, who started to be prioritized during the second week of vaccination with Sinovac (March 8), applying the same method and, in this case, 63% of the positive cases were not detected (with a diminished incidence of 76% for those over 55 years old with respect to a population between 18 and 49 years old10).
It is important to note that the relation between vaccination and the rise of positive cases in Uruguay, which is more notorious than in other countries because there is a relation not only on a magnitude level but also on a more detailed level in peaks in vaccination that reflect as peaks in positiveness. The fact that this relation on a magnitude level can be observed in different moments of the year and in different countries is indicative of a more profound cause. In mid-April 2021, mobility was diminished in Uruguay, but the effect was not as expected. Experts presented some theories as to why such us changes in behavior or a new strain P1 that started to circulate later than vaccination starts, but there were not proven enough to explain such a big change in Uruguay.12 The fact that our society responded in a correct way during one year and then experienced such a change that Uruguay became the worst in the world was a key factor to understanding something else was going on during the March-June 2021 vaccination period/wave of COVID (Figure 1). In this article, we intended to present an explanation based on a confounding behavior that is a simple way to elucidate this effect of loss of control present in Uruguay and possibly, in other parts of the world.
Uruguay’s government asked the population to act as per “responsible freedom” parameters, but what did this mean? It implied following the recommendations given in order to mitigate the effects of the pandemic: physical/social distancing, use of masks indoors and when using public transportation, and most importantly, isolation and testing when presenting symptoms; without being forcefully instructed to do so. That policy yielded very good results for almost a year in Uruguay, even when its neighboring countries had a lot of positive cases during such period. How is it possible to suddenly stop adhering to rules and immediately present the worst effects worldwide? What happened is that the rules of the game changed once vaccination started and people were told that it would be “normal to experience fatigue and headaches after vaccination”, two symptoms observed in COVID cases too and usually used to detect positive cases. Due to this fact, the “responsible freedom” policy became part of a large paradox, people, in a continued display of responsibility, followed the advice to the letter, and just vaccinated individuals were not all tested, at least those who were indeed positive cases, since those positive cases should have been included in the data but they were not (75% are not included in the registered positive cases informed by the Ministry of Health). Hopefully health care worker didn’t fallow this recommendation about secondary effects of vaccines and they have their own control with continuously test performed and this is why the positives tested cases were very similar to predicted ones for this group. Common people presenting COVID symptoms thought that they were experiencing side-effects from the vaccine and carried on with their normal daily life. The fact that in Uruguayan society, and contrary to what would be advisable, employees who go to work even though they are feeling poorly instead of taking a day off are well-regarded. Thus, one of the primary means of control for the pandemic was not complied with, since people with symptoms did not isolate and they were not taken into account as positive cases, which made it impossible to accurately monitor positive cases and the people they had been in contact with (of outmost importance when trying to limit the spread of the pandemic, since 25% of positive cases are contagious before the onset of symptoms,11 a parameter that was very well controlled due to the characteristics of small country like Uruguay), and they did not quarantine for 10 days as was originally advised to people being contact of a positive. Control on the pandemic was lost. Moreover, these cases were not visible, which made it impossible to identify the problem since invisible evidence is the most difficult to uncover. Even more so in this situation, in which a similar scenario could have been thought of, but it would not have been identified as a serious problem. While it might have been assumed that some individuals could have been administered the vaccine while being on an incubation period, it was considered of negligible importance the possibility of them becoming superspreaders and that they would be so for even longer than other superspreaders. And another summatory effect is that just vaccinated people could be in different stages of the incubation period so at day 0 of evaluation you have not only the people vaccinated the same day but also people vaccinated during the last 4 days that can manifest this day the first symptoms. These both factors are relevant to have the whole picture and they are illustrated by the model in Figure 4.
It has been sustained that preventive measures before vaccination is part of English culture and this has been the explanation why a survey study showed lower incidence before and after vaccination.13 However, it must be mentioned that only the participation in this kind of paid survey could bias the behavior so it is not a prove by itself that these preventive measure has been taken in general population.13 While there is another publication from a free survey in England through an app that no show data of the incidence before vaccination but have similar results to ours incidence just after vaccination.14 In the general population in case of symptoms, the person would not be vaccinated at that time, but they would be able to do so at a later time, not as in these kind of paid survey. What was stated by the government was that those individuals who had COVID should not be vaccinated while sick, which would not alter a priori the incidence before vaccination and, thus, would not alter it afterward. Is more natural to think that what did change was the society’s behavior after vaccination, since something that up to that point had been one of the primary means of control of COVID spread (stop circulating after first symptoms, as could be headache and fatigue) was “normalized”. In particular this kind of measure was the principal in a “responsible freedom” as was apply in Uruguay, perhaps in other countries where lockdown was apply this measure is a secondary measure compared to stopping circulation, work, sports and schools.
These cases might a priori seem few when thinking of the incidence in population multiplying by 0.5% of the population that was vaccinated (taking a fixed daily vaccination rate as an example), which would mean that only 0.0005% of population per day comply with both conditions at the moment of worst incidence in the pandemic which was 1/1000. However, upon observing the model, this would not be the case every day, but only on day 0 of vaccination, that is, the day in which vaccines started being administered in the country. On the following day, the fact that any individual from the population vaccinated that day or the day before could experience symptoms during this day and later be positive cases should be considered. That means a 1% of population for that day 2 of vaccination, and so forth. By day 5, in which 2.5% of the population has been vaccinated, we could expect 2.5% of positive cases to have been vaccinated, a figure that is more relevant. Furthermore, positive cases generated during days 0 to 4 and not detected must be added as possible superspreaders, since they are still contagious, which results in 7.5% of positive cases. Considering that according to the information provided by the Ministry of Health, 75% of positive cases were non-detected cases, the emergence of new non detected positives cases should be near 5,6% on 5 days of vaccination. These would be the cases present any given day following day 5 of vaccination. As we can see from the results on day 5, it was determined that 5% of positive cases were superspreaders when subtracting expected cases from real cases. The difference to the 5,6% we had theoretical calculated, is due to the percentage of people vaccinated per day during the 5-day period is not fixed and not exactly 0.5% as we supposed on the beginning of this paragraph. This 5% of non-detected positive cases could be a serious loss of control if we think of the contagion potential that they have on the rest of the population and very different from the first 0,5% of the population being vaccinated we started considering and perhaps authorities did as well.
We stated that from 10 to 20% of positive cases are responsible for 80% of COVID spread. The aforementioned 5% could be added to this, since those individuals satisfy the definition of superspreaders: they are not necessarily asymptomatic, they have symptoms that they confuse with side-effects from vaccination so they don’t get tested; they are under 60 years old and they work, which implies that carrying on their normal daily life could make them superspreaders. This increase in the number of non-detected positive cases could have affected the incidence, increasing it by 1.25x, also increasing natural positivity 5-6 days later (which is the incubation period for the disease). This loss of control or elevated multiplying factor, given the high rate of vaccination (with days in which nearly 2% of the population was vaccinated), favored the rise in mortality, reaching and maintaining the highest levels worldwide for 80 days (from April to June of 2021), even though mobility was diminished (which had previously proven successful, in January 2021) and even though increasingly more individuals were protected by the vaccines. But the loss of control was mainly driven by the introduction of a paradox at the level of “responsible freedom”, the main control factor in this policy was that if you feel with headache or body pain stop circulating and get tested while to vaccinated people we told them the contrary during the 3 days after vaccination.
The two most common side-effects of the vaccines are headache and fatigue, also very common symptoms of COVID. The better control a society has of these symptoms, the higher effect of the normalization of them on the just vaccinated population. Surely, we could say that Uruguayan population was very much under control during the pandemic and that did not change during vaccination, except for a number of vaccinated individuals that we lost control and had a very large impact. Thus, the systemic side-effects of the vaccines were normal (appearing in up to 15-20% of the vaccinated population11) and the individuals that failed concerning the control they should do were only a fraction of those. Nearly 1 in 50 of such cases corresponded to individuals who were not really experiencing side-effects of the vaccine, but COVID symptoms, a difference that is not easily determined without employing new methods to do so. Therefore, untested positive cases corresponding to just vaccinated individuals (due to the confusion of COVID symptoms with side-effects of the vaccines) are not traceable, just as the people they had contact with, which makes the veracity of that figure very difficult to confirm, but given that the consequences are visible, the hypothesis seems fairly simple, and the resolution is intuitive. Studying this phenomenon more deeply, with the available individualized data for the whole population of Uruguay and for the entire duration of the vaccination period, could be helpful in extending the analysis to a high percentage of the population. This study could also be easily replicated in other countries with good quality data.
A possible means to limit the viral spread to such level would be testing every individual being administered the vaccine to minimize the vaccination of infected individuals. Another possibility would be testing everyone presenting symptoms after vaccination, which would represent about 15-20% of the vaccinated population. A further possibility could be that recently vaccinated individuals are isolated for a period of 4 days. These alternatives should be evaluated while making other considerations, but given the importance of this phenomenon, measures during vaccination should be improved respect to “responsible freedom” policy.
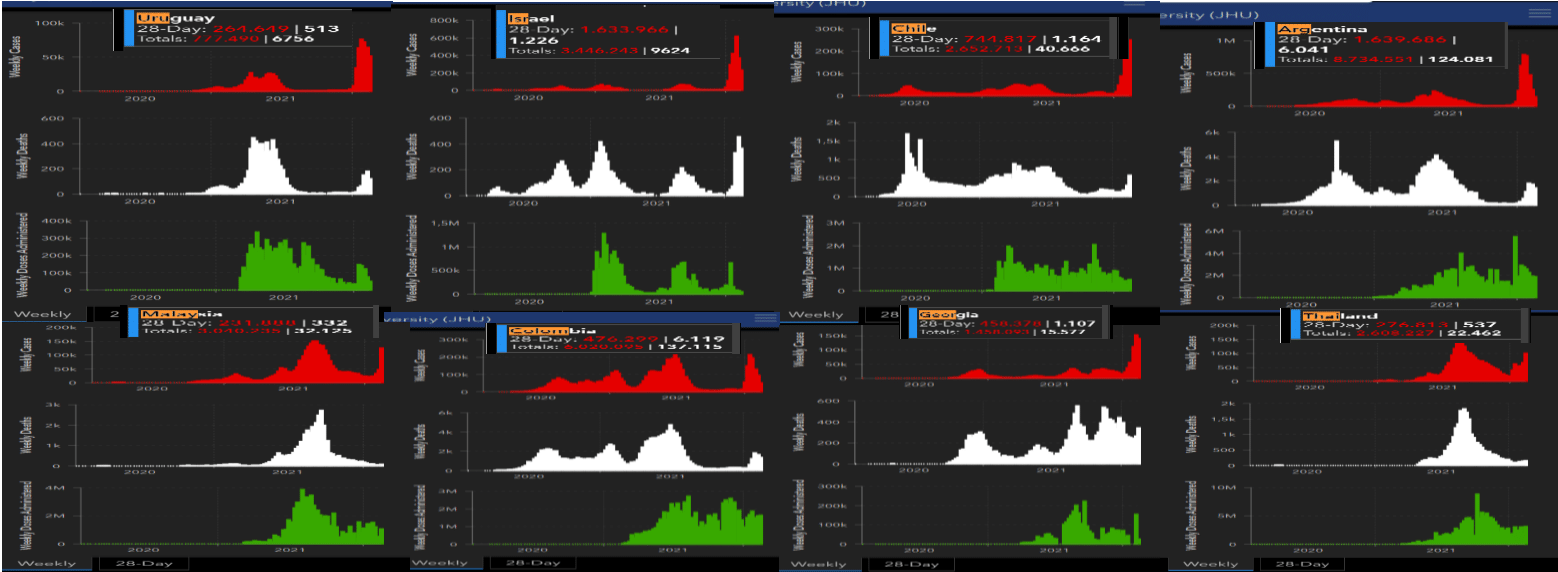
Annex 1 Countries with similarities to what was observed in Uruguay on a magnitude level -association between vaccination rate and positives cases. Most of the countries administered Sinovac vaccines (not Israel). The positive waves peaks are concomitant with vaccination in many countries (red are weekly positive cases, white are deaths per week and green are weekly vaccination cases). Data obtained from JHU.
None.
Author declares that there is no conflict of interest.

©2023 Marqués. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.