Journal of
eISSN: 2373-437X


Research Article Volume 8 Issue 1
1Department of Medicine, Health center university of the Punjab, Pakistan
2Department of Microbiology and Molecular Genetics, University of the Punjab, Pakistan
Correspondence: Snobia Munir, Research Scholar at Department of Microbiology and Molecular Genetics, University of the Punjab, Lahore, Pakistan, Tel 92-3158269694
Received: December 31, 2019 | Published: January 22, 2020
Citation: Malik N, Faisal A, Munir S, et al. Clinical and microbiological profile of urinary tract infection in male diabetic patients. J Microbiol Exp. 2020;8(1):30-34. DOI: 10.15406/jmen.2020.08.00282
The possibility of diabetic patients to develop various severe and fatal infections has been rising continuously. In diabetic patients urinary tract infection is very common. Due to the recurrent consumption of antibiotics and the usage of broad spectrum antibiotics, antibiotic resistant pathogens may develop in the urinary tract of diabetic patients. If untreated, UTI can lead to serious complications. Urine samples were taken from the Health Centre of Punjab University. Urine samples were plated on CLED media. Then identification of microorganisms was done by using the method of gram staining and by biochemical testing while some were identified by using API kit. After this, the sensitivity and resistance pattern of these uro-pathogens against different antibiotics were also checked by disk agar diffusion method. Physical and biochemical parameters of diabetic patients were also checked. Our results suggest that the presence of surplus glucose in the urine promotes the growth of pathogens that leads to UTI in diabetic patients. Improved glycemic control in diabetics may help in controlling the UTIs. The assessment of physical and biochemical parameters will be useful in the early diagnosis and prediction of diabetes mellitus. Sensitivity testing before antibiotic therapy may also help in the treatment and to prevent the resistance of antibiotics.
Keywords: urinary tract infection (UTI), CLED (Cysteine Lactose Electrolyte Deficient), API kit (Analytical profile index)
In the past few decades, diabetes has become prevalent in adults especially in Pakistan. The prevalence in diabetes might be due to changes in lifestyle.1 Recent studies have shown that about 422 million individuals in the world are suffering from diabetes mellitus.2 The chances of developing infections are very high in patients of diabetes. Skin infections, skin rashes, pneumonia (infection in lungs), infection in tissues and urinary tract infections are very common in patients of diabetes which can lead to serious outcome. Among all these infections, urinary tract infections seem to be very common.3 UTI affect all age groups but it seems to be more common in patients suffering from diabetes as compared to those who are non-diabetic.4 UTI can be treated by taking antibiotics. Sensitivity testing before starting antibiotic therapy is necessary to check the resistivity and sensitivity pattern of uro-pathogens.5 The research was carried out to find the uro-pathogens and to determine their sensitivity and resistance pattern against different antibiotics. It was also checked that why UTI is more common in diabetic patients as compared to non-diabetic patients. The physical and biochemical parameters of diabetic patients were also checked and these parameters were compared with the parameters of healthy control subject.
Clinical sampling
Urine samples were collected from the Health Centre of University of the Punjab, Lahore from august 2018 to February 2019 from diabetic patients that were suspected to be suffering from UTI. Urine samples were collected in dry, sterilized and leak proof plastic bottles. These bottles were sterilized by autoclaving them for about 15 minutes at 121°C (15 lbs pressure) and then the samples were collected from patients. Samples were 100 in number. Samples were instantly shifted to laboratory where they were plated on CLED media and then they were further processed. If delayed, samples were kept at 4°C and then they were examined within 2 hours of collection.
Laboratory investigation of urine samples
One drop of urine was taken on glass slide and its smear was made. Then the cover slip was set on the smear and then it was observed under microscope (40X).500 ul urine samples were plated on these petri plates. Petri plates were put on incubation incubated at 37°C for about 24 hours. After incubation, morphology of well isolated colonies was noted and total colonies’ number was counted. Then well isolated colonies of bacteria were streaked on N-agar plates.
Identification of bacteria
After that bacterial colonies were identified by various biochemical tests. While some were identified by API kit.
Biochemical tests
API kit
This API (Analytical Profile Index) -20E test strip is used to identify the enteric gram negative rods. API-20E test strip consists of wells in which dehydrated substrates is present. Bacterial suspension is used to rehydrate this. This strip consists of 20 tests.
Antibiotic sensitivity test
Resistance and sensitivity pattern of all organisms was checked against different antibiotics by Kirby Bauer method. Mueller Hinton agar was used for this. By using cotton swab colony was streaked on plate. Different antibacterial discs were placed on the plate. Plates were put on incubation at 37°C for 24. After incubation, zones of inhibition were recorded in mm.
Statistical analysis
The statistical analysis was done with SPSS statistical software package (version 22.0). Physical parameters including age, weight, height and body mass index (BMI) was calculated. The biochemical parameters which we assessed include sugar, HbA1c, cholesterol, LDL, VLDL, HDL, triglycerides, ALT, ALP, uric acid, creatinine and bilirubin. Significance of difference between mean analysis of control and diabetic groups was determined.
From the urine cultures, gram positive and gram negative organisms were identified by staining technique and it showed that more gram negative pathogens (82.3%) were present in the urine of diabetic patients as compared to gram positive pathogens (17.6%). Moreover, the number of lactose fermenter (80.6%) is also high in the urine samples (Table 1).
Organism |
Strains (N=300) |
Percentage |
Gram Positive |
53 |
17.60% |
Gram negative |
247 |
82.30% |
Lactose fermenter |
242 |
80.60% |
Non-lactose fermenter |
58 |
19.30% |
Table 1 Frequency of different pathogens in UTI
Gram positive and gram negative pathogens were further identified by biochemical tests and by using API kit and their results are shown in Table 2 and Table 3.
Organism |
Biochemical Reactions |
TSI |
|||||||
Oxidase |
Citrate |
Motility |
Indole |
Urease |
Slope |
Butt |
H2S |
Gas |
|
E.coli |
- |
- |
+ |
+ |
- |
Y |
Y |
- |
+ |
Klebsiella |
- |
+ |
- |
- |
+ |
Y |
Y |
- |
+ |
Proteus |
- |
+ |
+ |
- |
+ |
R |
Y |
+ |
+ |
Pseudomonas |
+ |
+ |
+ |
- |
D |
R |
R |
- |
- |
Table 2 Identification of gram negative organisms
Organism |
Identification Tests |
|||
Gram Staining |
Catalase Test |
DNase Test |
Novobiocin sensitivity |
|
Staphylococcus aureus |
Gram +ve cocci |
+ |
S |
+ |
Table 3 Identification of gram positive organism
Our results showed that Escherichia coli was the most common and the most recurrently occurring uro-pathogen which means that Escherichia coli is the principal agent which causes urinary tract infection in the patients of diabetes. While other pathogens that were found to cause urinary tract infection were Klebsiella, Pseudomonas Staphylococcus aureus, Candida and Proteus spp (Table 4).
Organism |
No.of pathogens (N=300) |
Percentage |
E.coli |
245 |
81.60% |
Klebsiella |
21 |
7% |
Pseudomonas |
17 |
5.66% |
Staphylococcus aureus |
7 |
2.33% |
Candida |
6 |
2% |
Proteus |
4 |
1.39% |
Table 4 Prevalence of UTI pathogens
Sensitivity pattern of pathogens were checked against different antibiotics by disk diffusion method. It shows that E.coli was resistant towards nalidixic acid followed by cephalexin, cefixime and pipemidic acid. Klebsiella was resistant towards cephalexin, cefixime, nalidixic acid, pipemidic acid and amoxicillin. Pseudomonas was resistant towards cephalexin, cefixime, nalidixic acid, and amoxicillin. Proteus was resistant towards cephalexin, cefixime, nalidixic acid, nitrofurantoin and pipemidic acid. Staphylococcus aureus was resistant towards cephalexin, cefixime, ciprofloxacin, ceftazidime, nalidixic acid, and pipemidic acid (Table 5 and Figure 1).
Antibiotic |
Sensitivity E.coli (mm) |
Sensitivity Klebsiella (mm) |
Sensitivity Pseudomonas (mm) |
Sensitivity Proteus (mm) |
Sensitivity Staphylococcus aureus (mm) |
Amoxicillin(AMC) |
75.1 |
54.9 |
38.7 |
99.9 |
99 |
Cephalexin (CL) |
27.6 |
18.7 |
13 |
0 |
0 |
Cefixime (CFM) |
39.8 |
14.3 |
38 |
0 |
0 |
Ciprofloxacin (CIP) |
73.9 |
68.9 |
90 |
100 |
0 |
Ceftazidime (CAZ) |
65.2 |
67.6 |
82 |
99.9 |
0 |
Nalidixic acid (NA) |
21.2 |
22.7 |
35 |
0 |
0 |
Nitrofurantoin (F) |
98 |
97.6 |
70 |
0 |
99 |
Pipemidic acid (PIP) |
52.4 |
22 |
66 |
0 |
0 |
Cefizox (ZOX) |
84.7 |
91 |
70 |
100 |
100 |
Imipenem (IMP) |
98.9 |
97.2 |
96 |
99 |
99 |
Table 5 Sensitivity pattern of different pathogens against different antibiotics
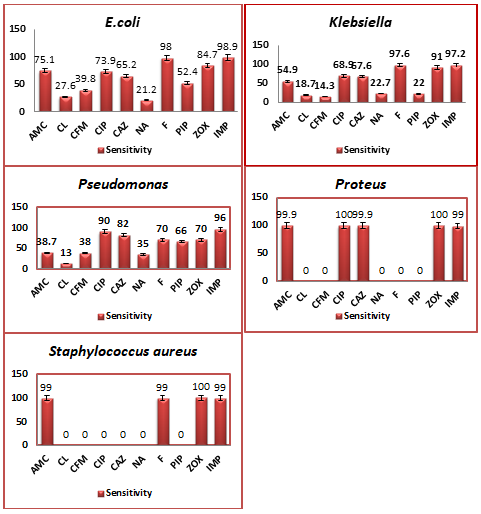
Figure 1 Graphical representation of sensitivity pattern of different pathogens against different antibiotics.
Table 6 shows the physical and biochemical parameters of normal and diabetic male patients. The difference or standard error in the mean age, weight, BMI, blood fasting sugar, bilirubin, uric acid, VLDL, HDL, triglycerides, HbA1c, ALT and ALP was statistically significant. While the difference or standard error in the mean height, creatinine, cholesterol, LDL was not statistically significant (Table 6).
Parameters |
Normal (N= 100) |
Diabetic (N=100) |
Age (Years) |
43.6±2.4 |
61.02***±1.57 |
Height (m) |
1.6002±0.065 |
1.6101*±0.009 |
Weight (kg) |
58.3±2.1 |
70.68***±0.793 |
BMI (kg/m2) |
23.9±0.8 |
27.42***±0.38 |
Blood Fasting Sugar (mg/dL) |
95.3±2.99 |
202.2***±6.67 |
Bilirubin (mg/dL) |
0.351±0.0079 |
0.762**±0.012 |
Creatinine (mg/dL) |
0.89±0.032 |
0.9**±0.017 |
Uric acid (mg/dL) |
13.5±0.09 |
13.9***±0.17 |
HbA1c (%) |
5.38±0.27 |
9.88***±0.231 |
Cholesterol (mg/dL) |
155±10.1 |
157.1***±5.786 |
LDL (mg/dL) |
94.08±2.15 |
104.4***±4.22 |
VLDL (mg/dL) |
16±1.2 |
31.4***±1.32 |
HDL(mg/dL) |
43.48±0.62 |
45.6***±0.645 |
Triglycerides (mg/dL) |
140.244±21.29 |
231.9***±9.62 |
ALT(U/L) |
30.7±5.5 |
42.9***±2.00 |
ALP(U/L) |
108.02±1.251 |
202.9***±9.00 |
Table 6 Physical and biochemical parameters of normal and diabetic male patients
+sign indicates the standard error. (P > 0.05) = non-significant. (P < 0.001)*= Highly significant. Number of “*” asterisks show the level of significant difference.
Due to destructive immune system type 2 diabetic patients have increased chances to develop UTI.6 The main reason for the prevalence of UTI in diabetics may be the nerve damage due to high glucose level in blood. Due to nerve damage, the bladder might not be able to sense the urine. As a result, urine stays in bladder for quite long time and thus increases the probability of infection.7 High level of glucose in urine also promotes bacterial growth in urine.8 In our research, urine samples of diabetic patients suffering from UTI were collected and inoculated on CLED media. As compared to gram positive pathogens, more gram negative pathogens are present in the urine of diabetic patients.9 Table 1 also showed that 82% were gram negative pathogens while 18% were gram positive pathogens in the urine samples of male patients. Table 1 showed that 80.60% were lactose fermenter while 19.30% were non-lactose fermenter.
The most common pathogen found in the urine samples of diabetics is E.coli. Along with E.coli other pathogens are also prevalent including Pseudomonas, Klebsiella, enterococci, streptococci, and Proteus mirabilis.10 According to Aguiar and Vignesh, UTI is the most frequently occurring infection in the patients of diabetes. The most dominant pathogens isolated were gram negative bacilli rather than gram positive pathogens. According to Vignesh et.al Escherichia coli were isolated from 30.2% of the subjects, Klebsiella pneumonia from 22.2%. Pseudomonas aeruginosa was isolated from 7.9%, Proteus mirabilis from 3.2%, Staphylococcus aureus from 3.2%. In our study, E.coli was the most common pathogen followed by Klebsiella pneumonia, Pseudomonas aeruginosa, Proteus mirabilis, Staphylococcus aureus (Table 4). In another study from India, it was found that E. coli was the most commonly grown organism.11,12
The main goal of treating UTI is to eliminate pathogens. So investigating the bacterial resistance and sensitivity is of utmost importance. The sensitivity and resistance pattern of different pathogens against different antibiotics has been shown in above table. In our research, 100 were control and 100 were diabetic patients. All these people were male. Their physical and biochemical parameters were compared. Physical parameters are age, weight, height and BMI while biochemical parameters are blood fasting sugar, uric acid, creatinine, bilirubin, cholesterol, triglycerides, HDL, LDL, VLDL, HbA1c, ALT, ALP. The difference or standard error in the mean age, weight, BMI, blood fasting sugar, bilirubin, uric acid, VLDL, HDL, triglycerides, HbA1c, ALT and ALP was statistically significant. While the difference or standard error in the mean height, creatinine, cholesterol, LDL was not statistically significant. The assessment of such physical and biochemical parameters will be useful in the early diagnosis and prediction of diabetes mellitus. So it is essential to evaluate these parameters by linking them with diabetes.
It is concluded from the studies that patients of diabetes mellitus suffer from UTI at some point in their life because the presence of surplus glucose in the urine promotes the growth of uro-pathogens that leads to UTI in diabetic patients. The most common pathogen that leads to UTI is E.coli. While the frequent usage of antibiotics and broad spectrum antibiotics may cause the production of antibiotic resistant pathogens in urinary tract. The mean values of physical and biochemical parameters of diabetics are high as compared to normal control subjects. The evaluation of these parameters can help to diagnose diabetes mellitus. Improved glycemic control in diabetics may help in controlling the UTIs.
University of the Punjab, Lahore provided funds. We acknowledge Dr. Nauser Malik, F.P.G.M.I., Department of Medicine, Health Center University of the Punjab, Lahore, for collection of samples.
The author(s) declare that the publication of this article has no conflict of interest.

©2020 Malik, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.