Journal of
eISSN: 2471-1381


Case Report Volume 4 Issue 2
1General Surgeon and Coloproctology, Santa Fe Foundation in Bogotá, Colombia
2General Surgeon, Santa Fe Foundation in Bogotá, Colombia
3Internist-Gastroenterology, Santa Fe Foundation in Bogotá, Colombia
4General Surgeon, El Bosque Clinic, Colombia
5General Surgeon and Coloproctology, Military University, Colombia
6General Surgery Resident, El Bosque University, Colombia
7Medicine intern, El Bosque University, Colombia
Correspondence: L Felipe Cabrera, Surgical Investigation Group of University El Bosque, General Surgeon, University El Bosque, Bogota, Colombia
Received: March 18, 2018 | Published: March 29, 2018
Citation: Eduardo L, David HJ, Margarita R, et al. Pylephlebitis both a surgical and non-surgical pathology: A 2-case report and literature review. J Liver Res Disord Ther. 2018;4(2):80 – 83. DOI: 10.15406/jlrdt.2018.04.00104
Pyleflebitis is a rare entity that presents with septic thrombophlebitis of the portal or mesenteric vein as a complication of abdominal infectious processes with or without bacteremia. It is associated with a high mortality rate from 11 to 32%, and incidence of 2.7per 100,000; the treatment is to eliminate the source of infection with antibiotic therapy, anticoagulation and/or surgery. The main cause is diverticulitis (30%), but pancreatitis causes portal thrombosis in 5%. There are positive blood cultures in 50-88% of cases, due to polymicrobial infection and the superior mesenteric vein is involved in 42%. Abdominal tomography is the gold standard for diagnosis. We present a double case report of patients with pylephlebitis of different etiologies who are offered both medical and surgical treatment with positive results.
Keywords: mesenteric thrombosis, pancreatitis, portal vein, pylephlebitis, sepsis
The first documented case of pylephlebitis was described by Waller in 1846 in a patient with appendicitis; in 1886 Reginald Fitz reported a series of 11 patients with pylephlebitis among 247 cases of appendicitis. Pylephlebitis is defined as a septic thrombotic event, accompanied by infection and inflammation of the portal system secondary to diverticulitis, appendicitis cholecystitis and pancreatitis among others. This event triggers bacterial drainage into the portal system resulting in bacterial polysaccharide capsule reticulation of fibrin and macrophage activation which in turn initiates a coagulative process. Mortality rates reach 25% with an incidence of 0.05%. The clinical presentation is non-specific and may be accompanied by fever, acute abdominal pain and jaundice.1,2 Here we present 2 cases of pylephlebitis managed medically by the general surgery department along with a literature review.
Case 1
A 49-year-old male patient presents with a clinical picture of 11days of vomiting and diarrhea accompanied by abdominal pain, fever and jaundice during the last two days. Clinical history is positive for systemic hypertension, obesity and smoking. Physical exam showed tachycardia, jaundice and tenderness in the upper abdomen. Lab works showed: no leukocytosis, neutrophilia of 92%, liver enzymes of 115mU/ml and 179 mU/ml. Alkaline phosphatase of 129U/I, total bilirubin levels of 5.2mg/dl, Direct bilirubin of 3.3mg/dl, indirect bilirubin of 1.9 mg/dl, HDL of 250U/l, Amylase of 289U/dl, Lipase of 1900U/L, C-reactive protein of 24mg/dl, Electrolytes, renal function and coagulation were all normal. Hepatobiliary ultrasound showed a collapsed gallbladder (Figure 1). Bile system MRI showed thickened gallbladder wall, no gallstones, normal bile duct, dilated superior mesenteric vein with flow defect suggesting thrombosis (Figure 2). Contrast abdominal CT showed peri-appendicular inflammatory changes including a single fluid collection of 17x16mm, peripancreatic fluid and SMV flow defect-opacification indicating thrombosis (Figure 3). Normal Endoscopic ultrasound (Figure 4). The patient had findings suggesting systemic inflammatory response syndrome however in the absence of peritoneal irritation and ongoing pancreatitis, a conservative antibiotic treatment was chosen with ampicillin tazobactam, anticoagulation therapy with LMW heparin for 10days. The patient is discharged with a 21day antibiotic and 6month anticoagulation therapy. Appendectomy was programmed thereafter and the patient had full recovery.
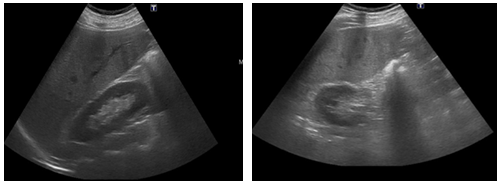
Figure 1 Diffuse hepatic parenchymal echogenicity alteration, non-dilated bile ducts and collapsed gallbladder. Normal pancreas and spleen without free peritoneal fluid.
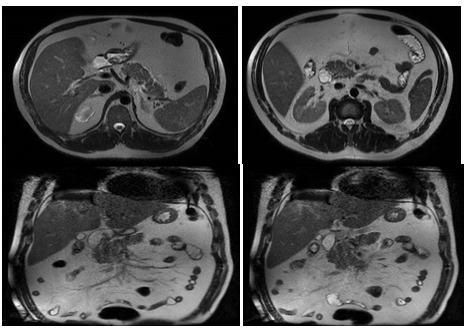
Figure 2 Fatty liver, Gallbladder with dilated wall without gallstones, no bile duct dilation nor stones. Inflammatory peripancreatic fat changes due to pancreatitis. No peripancreatic collections, increased SMV diameter with flow defect indicating thrombosis.
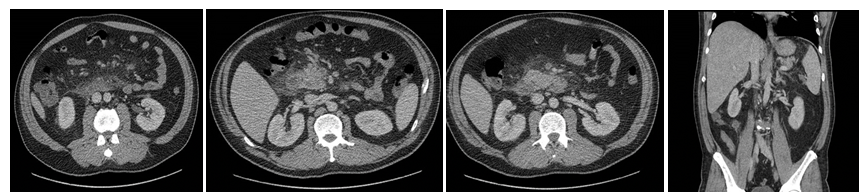
Figure 3 Periappendicular free fluid with dilated appendicular lumen, with a small 17x16mm collection. Inflammatory changes in the periduodenal mesenteric fat, peripancreatic and mesogastric zones with SMV opacification and flow defect.
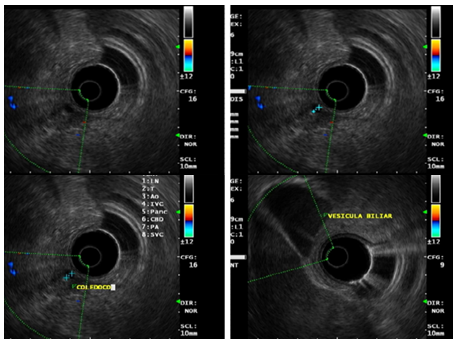
Figure 4 Endoscopic pancreatobiliary ultrasound showing a 5mm common bile duct without any other echographic abnormalities.
Case 2
A 75-year-old male patient presents with a clinical picture of 4days of fever, LIF abdominal pain and jaundice. Clinical history was positive for a laparoscopic gallbladder removal. The patient had a BP of 85/60mmHg, HR of 91bpm, RR of 22rpm, temperature of 38.2, jaundice without peritoneal irritation. Significant lab findings included thrombocytopenia of 82.000, Creatinine of 2.62, Total bilirubin of 4.3 Direct bilirubin of 3.5 indirect bilirubin of 0.8, Alkaline phosphatase of 161, normal liver enzymes, and ABGs showing metabolic acidosis. The initial proposed diagnosis was an intra-abdominal septic shock. ICU managed included Noradrenalin, IV fluids, broad-spectrum antibiotics with Meropenem and Linezolid. Initial Contrast abdominal CT showed a sigmoidal Hinchey 1A diverticulitis (Figure 5). Abdominal ultrasound showing a normal bile duct (Figure 6). Follow-up abdominal CT showing sigmoidal Hinchey 1B diverticulitis (microperforation), left intrahepatic portal vein thrombosis (Figure 7). Bile system MRI showing a common bile duct of 7.2mm (Figure 8). Despite treatment the patient had persistent bilirubin elevation of up to 11 mg/dl and a blood culture positive for a resistant E.coli. The patient was taken to a diagnostic laparoscopy finding a sigmoid diverticulitis with a plastron of pericolic fat tissue. A laparotomy incision was performed finding significant venous thrombosis of the left colic vein and sigmoid vein requiring a left colectomy with a Hartmann colostomy. Pathology report confirmed venous thrombosis. The patient had full recovery with antibiotics and was discharged.
The incidence of pylephlebitis is 2.7 per 100.000 people each year with a mortality of 11-32% with no age discrimination.3 In 1856 Rudolf Virchow described three factors leading to thrombosis formation; stasis, hypercoagulation and endothelial lesion. Pylephlebitis is therefore a consequence of an intraabdominal infectious process leading to an inflammatory, hypercoagulative, endothelial damaging along with cascade factors creating a thrombotic environment leading to a pathological bacterial thrombotic portal system. Initially this process begins in the small mesenterics veins which eventually migrates and creates an embolic septic event in the portal system.4,5 Pylephlebitis is usually a poly-microbial infectious event with Bacteroides fragilis being the most common isolated microorganism. Other Isolated bacteria include Escherichia coli, Proteus mirabilis, Clostridium, Klebsiella, Streptococcus pneumoniae and Aerobacter.6 The SMV is the most common vessel affected in 42%, followed by the intrahepatic veins 39%, splenic vein 12% and to a minor percentage the IMV 6%. The primary intra abdominal etiology is diverticulitis (30%), appendicitis (19%), IBD 6%, pancreatitis (5%), regional enteritis (4%) and malignancy (6%). Risk factor include coagulation disorders, portal hypertension, heart failure, malignancy, dehydration, post op sepsis and trauma.7 Clinical presentation varies from patient to patient however it should be suspected in patients with abdominal pain fever jaundice vomiting along with increased WBC, liver enzyme elevation and in some cases hepatomegaly.8 Blood cultures are positive in 50-80% of patients, Hepatobiliary ultrasound and portal Doppler usually detects flow defect and thrombosis. The gold standard of imaging studies for this pathology is the contrast abdominal CT. Abdominal MRIs are only indicated when other imaging studies are inconclusive.9 The mainstay treatment is broad-spectrum antibiotics with gram negative, anaerobic and aerobic coverage. However which antibiotic regimen is best is still in debate. The optimal duration of antibiotics is still unknown, however the recommended time frame is 4 weeks of which 2 weeks are IV.10 Early surgical intervention is usually required in most cases however some patients may be managed medically. Stitzenberg and col. reported a case of a patient with pylephlebitis and acute appendicitis managed with antibiotics, LMWH and interval appendicectomy. The use of LMWH is still in debate, Plemmons and colleagues described a case series of patients treated with antibiotics and LMWH with favorable results. Duffy and colleagues recommend the use of anticoagulation only is the thrombotic event extends beyond the portal system; signs of intestinal ischemia are present, lack of response to antibiotics or presence of systemic inflammatory response. Baril and colleagues recommend the use of anticoagulation only in a procoagulant state. Kasper and colleagues found no differences between the uses of anticoagulation vs no anticoagulation.10‒16 Thrombolysis with TPA is another controversial treatment option, Sherigar and colleagues published a case report of a patient treated with TPA in a patient refractory to antibiotics. Open thrombectomy has been abandoned due to high recurrence rates. Nishimori and colleagues reported a case of a patient treated with image guided endovascular Fogarty catheterization of the SMV when the patient did not respond to antibiotic therapy.17,18
Pylephlebitis has a high mortality secondary to abdominal sepsis even more than mesenteric ischemia. Because of its low incidence, an agreed consensus on its managed still does not exist. However it should be included as a differential diagnosis in patients presenting with jaundice, inflammatory response syndrome and acute abdominal pain remembering that antibiotics is the cornerstone treatment with surgery and anticoagulation therapy varying from patient to patient.
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
There is no conflict of interest.

©2018 Eduardo, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.