Journal of
eISSN: 2471-1381


Cholangiocarcinoma is an adenocarcinoma that appears from the epithelium of the bile ducts, being the second most common hepatobiliary primary malignant tumor, after just the hepatobiliary carcinoma responding by approximately 15% of the cases of hepatic neoplasia’s, having a challenging diagnosis and poor uniformly prognosis. It presents major prevalence in the south-east Asia and it is highly lethal. It corresponds to, approximately 3% of the tumors of the gastrointestinal tract, being mainly a tumor of the elderly, with a peak of incidence in the seventh decade of life and slight male predilection. The main symptoms are the loss of weight, abdominal pain and/or palpable mass, dark urine, alcoholic stools, itching and jaundice, being the later the most common. The authors report a case of cholangiocarcinoma in a young woman.
Keywords: cholangiocarcinoma, bile duct neoplasms, tomography, ultrasonography, tumor
CT, computed tomography; USG, ultrasonography; MRI, magnetic resonance imaging
Cholangiocarcinoma is an adenocarcinoma that appears from the epithelium of the bile ducts1,2being the second most common hepatobiliary primary malignant tumor, after just the hepatobiliary carcinoma2 responding by approximately 15% of the cases of hepatic neoplasia’s, having a challenging diagnosis and poor uniformly prognosis.3 It presents major prevalence in the south-east Asia4 and it is highly lethal.5
It corresponds to, approximately 3% of the tumors of the gastrointestinal tract, being mainly a tumor of the elderly, with a peak of incidence in the seventh decade of life and slight male predilection.2 The main symptoms are the loss of weight, abdominal pain and/or palpable mass, dark urine, alcoholic stools, itching and jaundice,6 being the later the most common.2
Responsible for significant morbidity and global morbidity, especially in endemic areas of infestation of the liver by worms–Opisthorchis viverrini, clonorchis sinensis.7,8 Other risk factors include, cirrhosis, infection by virus of hepatitis B or C4,8primary sclerosis cholangitis, intestinal inflammatory diseases,3congenital anomalies of the biliary ducts such as Caroli disease, cholelithiasis,6,8 alcoholism, chemical agents such as thorotrast,8 virus of Epstein-Barr, intra-hepatical lithiasis, and diabetes mellitus.7
A tumor that appears peripherally after the bifurcation of the right or left hepatic duct it is considered peripheral cholangiocarcinoma, where as a tumor that appears from one of the hepatic ducts or in the bifurcation of the common hepatic canal it is considered hilar cholangiocarcinoma-Klatskin’s Tumor.9
A 35-year-old woman refers to abdominal pain like colic for 15 days, associated with pruritus, diarrhea, dark stools and fecal acholia. Reports sensation of abdominal swelling days before the beginning of the pain denies smoking; alcoholism and other comorbidities stopped using oral anti-contraceptive 14 years ago after using them for a year.
Presents jaundice to the physical examination. Abdomen was flaccid, flat painful to superficial and deep palpation in the epigastrium and right hypochondrium, being the liver palpable about 5 cm from the right costal edge. Laboratory tests performed, in which anemia was discovered, increase in the levels of TGO and TGP, increase in the direct and indirect bilirubin and Gama-GT. Serum tests for hepatitis reaching just for hepatitis A. USG demonstrates liver with its volume increased due to the presence of well-outlined mass hypoechogenic, heterogeneous, with areas of necrosis in its interior, with anechoic affecting the segments II, III, IV, VIII, with peripheral and central vascularization. It also demonstrated dilation of the intrahepatic biliary ducts (Figure 1).

Figure 1 USG demonstrates liver with its volume increased due to the presence of well outlined mass hypoechogenic, heterogeneous, with areas of necrosis in its interior, with anechoic affecting the segments II, III, IV, VIII.
The CT scan with endovenous contrast demonstrated liver enlargement because of four nodular formations irregularly distributed and of various sizes, presenting the largest about 12,5x10 cm in the segments II, III, IV and VIII, expansive, hypodense with well-delineated contours, with heterogeneous impregnation after the infusion of the contrast, with a tendency to the homogenization in the late phase (Figure 2). It also demonstrates dilation of the intrahepatic biliary duct in the left hepatic lobe, probably of obstructive aspect due to the hepatic injury of greater dimension, not observing dilation of the extra-hepatic biliary duct and not characterizing the gallbladder.
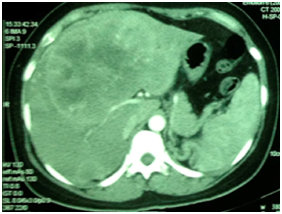
Figure 2 The CT scan with endovenous contrast (arterial phase) demonstrated liver enlargement because of four nodular formations irregularly distributed and of various sizes, affecting the segments II, III, IV, VII, expansive, hypodense with well delineated contours, with heterogeneous impregnation after the infusion of the contrast.
A laparoscopy has been performed with biopsy for anatomic pathological study. The laparoscopy demonstrates invasion of the hepatic hilus by the greater injury. The anatomopathological study demonstrates moderately differentiated cholangiocarcinoma diagnosis (Figure 3).
Several tumors or tumoral conditions must be included in the differential diagnosis of an intrahepatic mass.10Hepatocarcinoma with cirrhosis, sclerosing hepatocarcinoma and combinations-hepatocarcinoma/cholangiocarcinoma-may appear in an almost identical form of the cholangiocarcinoma.10 For diagnostic confirmation, one of the following methods must be performed: percutaneous biopsy, endoscopic USG with biopsy by thin needle or cholangiography.8 The cholangiography determines the extension of the extra-hepatic infiltration and Perihilar injuries, having a scene of the injuries and surgical planning.11 Also, it allows tissue samples to be obtained with a technique of cytological brushing, despite the low accuracy reported (9-24%) of the technique.11
The curative treatment is the complete surgical resection,3,12 with recurrence rates of 60% to 90% after the procedure.13The surgical objective for the cure and long-term survival is the complete excision with free histological edges, such as the resolution of the biliary obstruction and restoration of the bilioenteric communication.12The contraindications for the curative resection are: advanced disease with involvement of the left or right hepatic duct, atrophy of a hepatic lobe with involvement of the contralateral branch of the portal vein or of secondary biliary duct, invasion of one of the hepatic arteries (proper hepatic artery, bilateral hepatic arteries) or of the main portal vein and metastasis to lymph nodes, peritoneal cavity, or distant organs.12
The hepatic transplantation, although is not done in a routine duct, may augment the survival time in selected sick patients, in whom the resection is not viable due to the locally advanced disease.14
None.
The authors declare that there is no conflict of interests regarding the publication of this paper.
The written informed consent of the patient was obtained, for the publication of her case.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.