Journal of
eISSN: 2373-4345


Review Article Volume 15 Issue 4
1Dentist, Cordero Dentist University of Carabobo, Venezuela
2Odontologist, Oral and Maxillofacial Surgery, University of Carabobo, Venezuela
3UNERG Dentist, Professor, Dr. in Education Sciences UPEL, Venezuela
4Dentist, University Santa Maria, Oral Implantology University Europea de Madrid, Venezuela
5Dentist, Gran Mariscal de Ayacucho, Venezuela
Correspondence: Zulay Palima González, UNERG dentist, UNERG professor, faculty of dentistry, subject applied biochemistry, specialist in university teaching UNERG, master in oral surgery CIU, Dr. in education sciences UPEL, Venezuela
Received: September 09, 2024 | Published: October 1, 2024
Citation: Salazar AV, Cautela JP, González ZP, et al. Surgical approach to closure of orosinusal communication with pedunculated Bichat adipose tissue, case report and literature review. J Dent Health Oral Disord Ther. 2024;15(4):155-158. DOI: 10.15406/jdhodt.2024.15.00629
Introduction: Orosinusal communications are pathological conditions that are characterized by the loss of hard and soft tissues that separate the oral cavity from the maxillary sinus. It is more common between the third and fifth decade of life, with predominance in the left upper jaw area due to the Uncomfortable work position and poor visualization. There are different treatments that can be used for this closure, such is the case of closure with a pedicled Bichat bag because one of the main advantages of this technique is the excellent blood supply of the flap, the lower morbidity of the donor site and the preservation of the normal anatomy of the oral mucosa.
Objective: To perform a surgical approach to close the orosinusal communication using a pedicled Bichat bag in a patient who attended the Salazar Cordero Dental Center.
Materials and methods: Data collection through interviews, in addition to using instruments such as clinical history, informed consent, radiological studies, clinical photographs, complementary examinations and surgical treatment.
Result: A satisfactory result was obtained, with good tissue closure, without complications, the patient is evaluated every 15 days to see his healing process.
Conclusion: Knowledge and management of the techniques in closing the orosinusal communication is of vital importance when presenting this type of complications and thus providing appropriate treatment to our patients.
Keywords: communication, surgical, treatment, tissues.
Routine extraction is a common procedure performed by both the general dentist and the oral surgeon, most maxillary premolar/molar extractions heal without problems, but some may cause an involuntary opening into the maxillary sinus.1 It is there where a buccosinusal communication or oroantral communication is generated, which is nothing more than a pathological condition characterized by the loss of the hard and soft tissues that separate the oral cavity from the maxillary sinus, existing between both anatomical compartments a solution of continuity.2 The most frequent etiology of SBC is the exodontia of molars or upper premolars. This fact is related to the close relationship that the apices of these teeth often have with the maxillary sinus,3 in addition to procedures related to dental implants, cystic or tumor diseases, infections and trauma,4 this type of large communications can cause, after the accumulation of saliva and food, chronic sinusitis and oroantral fistulas. Therefore, large ACOs (>2 mm) need to be surgically closed to avoid complications.5 This oroantral communication repair can be performed using advancement flaps such as buccal fat pad as a pedicled graft, palatal rotational advancement flap closure, buccal glide flap, using bone grafts with or without barrier membrane, and other methods.6
Since Egyedi described in 1977 the technique of closing oroantral communications by means of a pedicled Bichat ball, this has become a useful procedure in oral regenerative surgery,7 this pocket is a lobulated mass located in the masticatory and buccal spaces. Anatomically it is limited medially by the buccinator muscle, anterolaterally by the zygomatic arch, the deep cervical fascia and the muscles of facial expression, and posteriorly by the parotid gland and the mandibular ramus with attached masticatory muscles.8 Several authors consider the Bichat adipose ball graft technique favorable for cases with severe damage of the palatal and/or buccal mucosa, and for preservation of the depth of the vestibule and also for the high success rate obtained with the technique.9
The use of a Bichat adipose pouch flap in the closure of oral sinus and maxillary osseous defects has been reported in several studies with positive results, as it is a simple and well tolerated technique,10 because one of the main advantages of this technique are the excellent blood supply of the flap, less donor site morbidity and preservation of the normal anatomy of the oral mucosa,11 along with good healing potential and adequate epithelialization with a low complication rate when used.12 In this sense, the combination of buccal flap and Bichat adipose pouch is appropriate for the closure of fistulas located in the second and third molar area, where the covering of the fatty flap with the mucoperiosteal flap provides two closure planes of different depths, which reduces the infection rate and improves the healing process, due to less exposure.10
Data collection by interview, using instruments such as: clinical history, clinical photographs, panoramic radiography, CT, laboratory tests, histopathological studies and informed consent. Descriptive analysis techniques were used, where the sequence of treatment, patient history and informed consent were observed.
Medical history
Age: 53years, Sex: female, Occupation: merchant
Clinical data
Reason for consultation: “I have a communication between my nose and mouth”.
Present Illness: Female patient, 53 years old, white, from Acarigua - Portuguesa State, comes to the dentistry office referring the passage of liquids from the mouth to the nasal cavity for approximately 2 months after an exodontia of the UD 25 and 26, she also manifests moderate intensity pain in that area, which stops with the intake of ibuprofen 400mg every 8 hours. The patient also manifests rhinorrhea and cacosmia since the surgery.
Family history: Parents with long-standing treated vascular disease.
Personal history: Patient reports cardiac arrhythmia since childhood, in 2012 she underwent cardiac ablation and is currently under pharmacological treatment with propranolol 10mg 1 daily 8pm.
Clinical Findings: The clinical examination showed erythema in soft tissue in the upper left portero area with presence of fistula, restorative treatments in poor condition in ud 17,16,15,27,37,36,45,47, usencia in ud 24,25,26,46, fixed prosthesis between ud 45 and 47 with pontic in ud 46, presents calculus and generalized alba matter.
Treatment Plan: Initial phase, history taking, panoramic study and analysis, cone beam tomography. Basic Sanitation Phase, Tartrectomy, prophylaxis, scaling and root planning, to this is added the taking of antihistamine every 8 hours for 5 days prior to surgery. Surgical phase, approach and closure of buccosinusal communication using pedicled Bichat bag. Prosthetic phase, evaluation and discussion of the case with the multidisciplinary team. Maintenance and control phase, photographic record, clinical review, healing evolution and update of Panoramic and tomography.
Appointment 1
Filling out the medical history, signing the informed consent form, proceeding to take intraoral and extraoral photos for the realization of this clinical case and to follow up the treatment, the patient is instructed to undergo laboratory tests for the day of surgery (Figure 1 & 2).

Figure 2 Intraoral photos Image: (A) Maximal intercupid, (B) left upper and lower posterior area (the patient manifested pain at opening).
Performing a clinical examination can help us with the detection of pathologies and injuries, it also serves as a means of information and enriches our knowledge when carrying out any research work.
Appointment 2
In this appointment we analyze and evaluate the panoramic view after the buccosinusal communication, where we observe discontinuity between the maxillary sinus and alveolus in the left upper posterior area where an exodontia of tooth 26 was performed, absence of tooth 24 and 25, presence of obturator treatment compatible with endodontics in tooth 15,16,17,27,36,44, image compatible with restorations with old restorative material (amalgam), presence of obturator treatment compatible with endodontics in tooth 15,16,17,27,36,44. 24 and 25, presence of obturator treatment compatible with endodontics in Units 15,16,17,17,27,36,44, image compatible with restorations with old restorative material (amalgam) in Units 16,17,27,37,36,47, in addition there is evidence of treatment with metallic material in Units 45,46,47.
Then we evaluated the cone beam computed tomography, observing a hypertensive image with defined edges located in the maxillary sinus compatible with a mucosal retention cyst, in the same way a discontinuity is perceived in the upper left postero area at the height of the maxillary sinus where dental unit 26 was located compatible with a buccosinusal communication, in the same way hyperdense images compatible with dental units 27 and 28 are observed. Laboratory tests are verified and after having obtained all the clinical and radiographic studies, the surgical procedure is planned where excision of the mucous retention cyst will be performed in addition to closure of the bucco-sinusal communication using a pedicled Bichat bag (Figure 3).
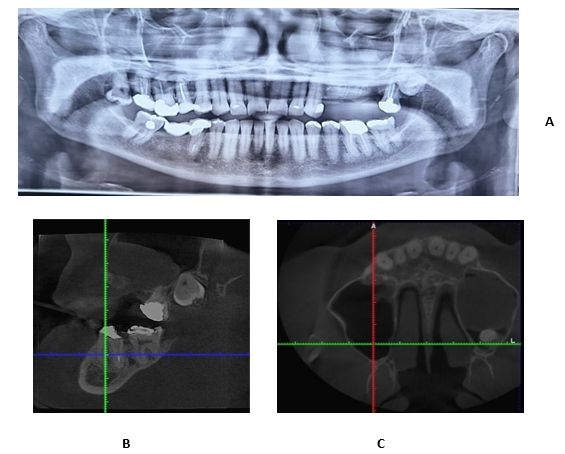
Figure 3 Panoramic and cone beam tomography: (A) Panoramic view from 04-22-2024. This panoramic view that the patient is carrying is after the extraction of UD. 26 (B) Sagittal section where a discontinuity between the alveolus and the maxillary sinus is observed, in addition to a hyperdense lesion compatible with a mucosal retention cyst, hyperdense images compatible with UD are also observed. 27,28 (C) Transverse section where a hypertensive image compatible with a space-occupying mucosal retention cyst is seen, hyperdense image compatible with UD. 28.
Appointment 3
The patient is given a clear and precise explanation of the entire surgical procedure to be performed, the risks and complications that may exist, the patient reads and signs the informed consent form and then proceeds with the surgical procedure.
The planned surgery was a closure of the buccosinusal communication with a pedicled flap of Bichat's pouch after 5 days. Pre-surgical medication of 10 mg of oral cetirizine was prescribed daily for 5 days.
The surgical procedure began with proper management and control of asepsis and antisepsis with 0.12% chlorhexidine, local anesthetic with 2% lidocaine was applied to the posterior and middle alveolar nerves and palatine nerve in the left upper posterior area. An incision was made to create a trapezoidal mucoperiorthotic flap, extraction of units 27 and 28 was performed, excision of mucosal tissue in the maxillary sinus, and lavage of the paranasal sinus with 0.9% saline solution.
A 5mm horizontal incision was then made in the inner area of the cheek and with the help of mosquito forceps the fatty sac was exposed. It was carefully repositioned until enough could be obtained to use it to close the communication. It was approached with 3.0 absorbable suture, suturing its edges with the palatal mucosa and finally the tissue synthesis of said area was carried out.
The patient is given instructions for postoperative recovery, which involve a soft diet, cryotherapy, good oral hygiene, no physical effort, and 72 hours of rest.
The pharmacological indications given to the patient in relation to antibiotic therapy, amoxicillin + clavulanic acid 875 mg every 12 hours for 7 consecutive days, analgesic ibuprofen 600 mg every 8 hours for 5 days, ketorolac 10 mg every 8 hours for 3 days and antihistamine such as cetirizine 10 mg daily for 10 days. The patient is given an appointment after 15 days.
After 15 days, good healing was observed, with the loss of 2 stitches without any dehiscence. The patient maintained good oral hygiene. After 15 days, favorable recovery was observed. The patient was instructed to undergo removable prosthesis treatments in the area after one month (Figure 4).
The 53-year-old female patient who came to his private practice at the Salazar Cordero Dental Center in Acarigua - Edo. Portuguesa, was approached in a global way, from the simplest to the most complex, both at the sinus level to eliminate any type of pathology that she presented with antihistamine days prior to surgery, and at the oral level, since the implementation of the pedicled Bichat bag as a mechanism to achieve closure of bucco-sinusal communication allowed to achieve the objectives set, with the help of a good anamnesis, clinical, radiographic approach and the group of dentists in charge of the case, who also helped to establish a good diagnosis when treating the patient.
Although it is true that buccosinusal communications are pathologies characterized by the presence of a continuity between the oral cavity and the maxillary sinus, where there is loss of hard and soft tissue, these belong to one of the most frequent accidents at the level of the upper jaw, facilitating contamination at a microbial level from the oral cavity to the maxillary sinus. It should be noted that these communications can be treated immediately depending on the size of the lesion generated and with a good approach and knowledge of the dentist.
In this clinical case, all biosafety standards were met, local anesthetics were used with good posterior, middle and palatal alveolar technique in the affected area, a trapezoidal flap was performed, mucoperiosteal detachment, cleaning with 0.9% saline solution and excision of the space-occupying lesion at the level of the maxillary sinus was performed, which histologically showed a mucosal retention cyst, a pediculated Bichat fat pad was used to correctly close the communication and tissue synthesis was performed.
The patient was assessed every 15 days for follow-up and monitoring of healing, in addition to a consultation with a prosthesis specialist to manage the construction of a removable prosthesis for the affected area.
A good approach when performing extractions at the level of the upper jaw in the posterior area will avoid complications of this type.
The pedicled Bichat fat pad will always be a good resource that we can rely on when presenting a bucco-sinusal communication.
Performing the Valsalva technique will help us identify whether we are in the presence of a bucco-sinusal communication.
Having a clear knowledge of the maneuvers at the time of the communication will help in the prognosis and favorable evolution of the patient.
General dentists must have a clear knowledge of head and neck anatomy to avoid this type of injury after tooth extractions, and if possible refer to specialists trained to resolve such communication.
Complementary examinations will always be of great help in addressing and planning in order to provide the patient with a good surgery.
Encourage patients to go to verified and legal private dental centers with oral health professionals who guarantee good care and treatment.
Promote thorough and correct examination in private dental centers to manage injuries of this type.
None.
The authors declare that there are no conflicts of interest.

©2024 Salazar, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.