Journal of
eISSN: 2373-4345


Research Article Volume 15 Issue 3
Diploma in Economics, specialised as health-economist in dentistry, former Head of Department of “Dental Care“ in the Federal Ministry of Health, Bonn/Germany and German representative in the Council of European Chief Dental Officers (CECDO), ret, Germany
Correspondence: Rüdiger Saekel, Marienburger Str. 28, D53340 Meckenheim, Germany
Received: June 10, 2024 | Published: July 1, 2024
Citation: Saekel R. Oral health in lower middle-income African societies - surprising outcomes and strategic consequences. J Dent Health Oral Disord Ther. 2024;15(3):105-117. DOI: 10.15406/jdhodt.2024.15.00621
Objective: To assess the oral health status of the population in selected African countries and compare the outcomes with emerging and highly developed countries worldwide using quantifiable results.
Method: By means of a composite indicator - the Dental Health Index (DHI) - the dental status of a country´s entire population is measured to arrive at a ranking of oral health performance. This performance is then compared with countries belonging to other development stages. The present study is descriptive and, whenever possible, uses existing epidemiological data from national representative surveys.
Results: With the exception of Rwanda, the Sub-Saharan African countries performed better than the three North African countries of Egypt, Morocco and Tunisia, although the Arabic-speaking countries have higher Human Development Indices by comparison. Within Sub-Saharan Africa, the best rankings were achieved by Uganda, Kenya and Nigeria. However, the other Sub-Saharan countries studied also exhibited similarly low DHIs. Rwanda, Egypt, Tunisia and Morocco ranked last. One striking finding is that the Sub-Saharan countries studied show more favourable DHI outcomes than emerging or high-income countries. As large parts of the African population have been widely untouched for decades by dental services, the relatively favourable outcomes in African societies are difficult to explain and contradict conventional dental theory. The reasons behind this finding are not fully understood. It is only in the area of untreated oral diseases that the African countries perform much worse than the more developed countries.
Conclusion: If African countries were to concentrate their scarce resources on a few vital segments of oral health, they would have the opportunity, in light of favourable morbidity structures, to gradually improve the oral health status of large parts of the population. Should they choose this route, priority should be given to the young generation. Three key action fields are decisive: mobilising oral self-care, enlarging the dental workforce by training sufficient mid-level personnel and creating a true primary oral health care system which is community-centred and complemented by strictly preventive, minimally invasive and tooth-retaining treatments under the guidance of a strong public sector.
Keywords: oral health in Africa, dental morbidity structures in Sub-Saharan Africa, oral health status in North Africa, comparisons between dentition status in African and emerging/high-income countries, Africa-adjusted oral care strategies
Africa is a fascinating continent in manifold respects. With its different climate zones, cultural diversity, geographical and topographical peculiarities, its inherent natural beauty and multifaceted ethnicities living in extremely challenging conditions, the continent offers great opportunities for research. With its over two thousand different ethnic groups, Africa has ‘the world´s most diverse genetic make-up‘ and is the ‘repository of human genomic diversity‘. As such, it serves well as a reference resource for exploring the role of genomics in oral diseases.1 In fact, Africa has long been a neglected continent as far as research is concerned. However, in the last decade, as many African countries began to see economic progress that outpaced other world regions,2–4 interest in Africa has been growing. One of the most neglected fields of research in Africa is that of oral health. While there is abundant literature on oral health topics in industrialised countries, such literature is rare for developing countries and much more so for low-income and lower middle-income African states. This is particularly disadvantageous because oral health faces extraordinary difficulties and barriers in tropical conditions, as mirrored by the state of health care in general on the continent. Apart from the fact that oral disorders share common risk factors with cardiovascular diseases, diabetes mellitus, oral cancers and chronic pulmonary diseases, which are preventable and lifestyle-related,5 there are also the prevailing serious life- threatening diseases of HIV/AIDS, tuberculosis and malaria, mainly in Sub-Saharan Africa, which might interact with high prevalence rates of periodontal disorders in those countries.6–8 In this context, mention also needs to be made of Noma, a gangrenous stomatitis that destroys soft and hard tissues of the mouth and face and affects mainly children ≤ 6 years. This disease is caused by protein-energy malnutrition and vitamin deficiencies (A, B, C, iron or magnesium) and is specific to the Sub-Saharan region, the highest incidences being in Nigeria and Egypt,7 two countries studied in this paper. Our study concentrates only on the main oral diseases, caries and gum diseases, and their consequences.
Over the last 50 years, oral health has improved greatly in Western Europe and North America. This was enabled by remarkable progress in modern preventive dentistry, propelled mainly by researchers from Scandinavia, Switzerland, The Netherlands, Great Britain and the USA. The improvement of oral health status started in the 1970s among the younger generation and reached the adult age-classes at the beginning of the 1990s. Since then, oral health improvement gradually spread to older age-classes. The reasons for this overall change in oral health status can be attributed to the success of modern preventive research, the establishment of prevention and promotion programmes for children´s oral health, systematic training of oral hygiene practices, beginning at toddler age, sufficient exposure to fluoride and easy access to oral care facilities assured by appropriate dental care systems.
Much groundbreaking knowledge in the field of oral disorders and oral health is owed to the World Health Organization (WHO). With comprehensive, population-centred publications and approaches emphasising common welfare, WHO and its many open-minded and dedicated researchers play a decisive role in promoting progress in preventive and tooth-retaining dentistry, particularly in the developing world. Thus, if there is any discussion of oral health in African states, it is mainly done in the context of WHO-initiated studies that focus on the WHO regions: the African-, Eastern Mediterranean-, European-, South-East Asia-, Western Pacific- and the Region of the Americas.9 Of the six WHO regions, three are important for our study, as the Arabic countries of North Africa fall into the Eastern Mediterranean Region and the third region, Europe, is used for comparison purposes.
Findings from one global study show that the highest numbers of untreated cases of caries in permanent teeth and severe periodontitis were found in the societies of lower middle-income countries,10 to which most of the African countries belong. As for severe tooth loss (<9 teeth), Kassebaum et al. reported significant reductions between 1990 and 2010 in many of the industrialised and developing countries of the 21 Global Burden Disease (GBD) world regions, except Central Sub-Saharan Africa and a few other regions (e.g. Eastern Europe, Oceania).11 In contrast to these findings and assessments, other authors argue that, globally, dental conditions have hardly improved in the last 25 years and conclude that there is a worldwide rise in oral disorders.12 Bedi and Scully interpret the global trends of the last decades as dental decay decreasing in industrialised and rising in developing countries.7 Moreover, Benzian and Listl assert that, from a global perspective, the prevalence of oral diseases in the period 1990-2017 remained more or less unchanged.13 A further global study revealed that 69% of the world´s dentists serve 27% of the world´s population while Africa has only a 1% share of the total dentist workforce.14 The authors predict that the disparity is likely to grow even further, due to differential population growth. Our study intends to examine whether and which of these large-scale observations can be confirmed by investigations of selected lower middle-income African countries.
The current knowledge of dentistry with respect to the main diseases, caries and periodontal disorders and their interactions throughout the course of life, is summarised by WHO as follows: deciduous teeth are prone to caries after eruption and caries prevalence peaks around the age of six. In permanent teeth, caries prevalence rises strongly after eruption and culminates in early adulthood, subsequently stabilising for the rest of a person´s lifetime. Severe periodontitis starts at middle age and peaks at about age 60. Tooth loss also begins in middle- aged adults and edentulism peaks in old age (≥80 years).9 In general, ‘all oral diseases are chronic, progressive and cumulative in nature‘.9
These fundamental findings are helpful for appreciating the overarching problems of oral health in the world and for evaluation purposes. Consequently, global knowledge and insights are broken down for single countries of the developing world, in our case, selected African countries with peaceful socioeconomic and governmental structures below the threshold of emerging- country status. This being said, studies on oral health in these African countries are scarce, data collection cumbersome and the resulting data are not always nationally representative. This article aims to close this knowledge gap and intends to propose strategies adapted to the prevailing circumstances that might contribute to improving the dental health status of underserved African societies.
Furthermore, it is highly interesting to conduct a detailed analysis of oral health on the African continent, as it allows us to study how oral diseases develop when most of a country´s population remains largely untouched by dental care over decades. If treatment occurred, it consisted mostly of extraction or drug prescription.15,16 As a result, our initial research position could be compared to a study on the natural history of periodontitis-related tooth loss in a region in which periodontal diseases have not been treated for over 40 years.17 Our second objective is therefore to examine whether the findings on oral health status in Africa correspond to dental theory and if not, to determine the reasons for any discrepancies.
For the empirical data, we relied on the WHO/Malmö University global oral data base. Outdated or missing data on certain indicators, age groups or countries were supplemented by systematic internet research in English- language publishing journals. We used the WHO standard reference age classes for 5/6-, 12-, 35/44-, and 65/74- year-olds and added the data for missing teeth in seniors, as this is a key indicator in measuring the cumulative disease burden across the course of life. As caries indicators, this study utilises the proven dmft-index (decayed, missing, filled teeth) for primary teeth, the DMFT-index (Decayed, Missing, Filled Teeth) for permanent teeth and, for measuring periodontal diseases, the Community Periodontal Index (CPI) grade 4 (pocket depth ≥6 mm). An important aspect is that we measure the oral health status of the entire population and not only of a certain age group intended to be representative for the whole population, most often 12-year-olds, middle-aged adults or the elderly. As has been proven in several studies, a single age group can never reliably represent the dental status of the entire populace.18
The population´s oral health status is measured by the composite overall indicator, the Dental Health Index, the construction of which has been already described elsewhere.19,20 The formula reads as follows:
DHI=(Caries-free Index 5/6 + DMFT 12 + DMFT 35/44 + MT Index 65/74 + Edentulism Index 65/74): 5. The lower the DHI, the better the oral health status.
This study is descriptive and cross-national, and largely uses existing epidemiological data from national representative surveys. Where this is not possible, we rely on broader data pools that also enable limited generalisations. As we wish to analyse the oral health realities obtaining in African societies, the descriptive study design is best suited to identify similarities or differences in order to later demonstrate evidence of associations, relationships and influencing factors. Conclusions on cause and effect are limited, owing to the non-experimental study format.
The primary criteria for selecting these specific countries on the African continent were their development stages
- lower middle-income and low income - including signs of economic break-up but below the threshold of emerging economies. Furthermore, peaceful societal and -functioning governmental structures were additional requirements for inclusion. To get as true a picture as possible of all of Africa, both the Arabic-speaking North African and a selection of Sub-Saharan African countries needed to be included. Moreover, it was important that oral health related epidemiological material, which could be evaluated, was available for the countries. In North Africa, Egypt, Morocco and Tunisia, as well as in Sub-Saharan Africa, the discretely populated countries of Uganda, Nigeria, Namibia, Kenya, Mozambique, Malawi, Rwanda and Tanzania were chosen. Table 1 provides an overview of the current socioeconomic country characteristics, knowledge of which is necessary for our topic. We will use these facts in the evaluation process.
|
Country |
Economic development level |
Human development index (HDI) |
HDI category1 |
Urbanisation (%) |
Middle-class2 (%) |
|
Egypt (EG) |
Lower middle-income |
0.73 |
High |
43 |
18.7 |
|
Morocco (MA) |
Lower middle-income |
0.68 |
Medium |
65 |
15.1 |
|
Tunisia (TN) |
Lower middle-income |
0.73 |
High |
70 |
25.8 |
|
Kenya (KE) |
Lower middle-income |
0.58 |
Medium |
29 |
12.5 |
|
Malawi (MW) |
Low income |
0.51 |
Low |
18 |
4.6 |
|
Mozambique (MZ) |
Low income |
0.45 |
Low |
38 |
4.3 |
|
Namibia (NA) |
Upper middle-income |
0.62 |
Medium |
54 |
17.2 |
|
Nigeria (NG) |
Lower middle-income |
0.54 |
Low |
54 |
12.5 |
|
Rwanda (RW) |
Low income |
0.53 |
Low |
18 |
4.5 |
|
Tanzania (TZ) |
Lower middle-income |
0.55 |
Medium |
37 |
6.1 |
|
Uganda (UG) |
Lower middle-income |
0.525 |
Low |
26 |
6.4 |
The results for the single age-brackets in the investigated countries and the composite overall DHI are documented in Table 2.
|
Cou ntry |
Survey year |
Cariesfr ee 5/6 % |
Inde x (1) |
DMFT 12 (2) |
DMFT 35/44 (3) |
M-T 65/74 abs. |
Index 18 (4) |
Edentulis m 65/74 % |
Inde x (5) |
DHI17 (6) |
Ra nk |
|
EG |
2001/13/ 17-18/19 |
≈391 |
6.1 |
0.4 |
6.1 |
5,4 |
3 |
7.814 |
0.8 |
3,28 |
8 |
|
MO |
2002- 04/12/16- 17 |
≈261 |
7.4 |
4.8 |
14.9 |
≈3.913 |
2 |
20.65 |
2.1 |
6,24 |
11 |
|
TN |
8/19/200 3 |
44 |
5.6 |
1.4 |
5.6 |
15.8 |
8 |
32 |
3.2 |
4.76 |
10 |
|
KE |
2001/201 5 |
54 |
4.6 |
0.5 |
2.8 |
1.66 |
1 |
6 |
0.6 |
1.9 |
2 |
|
MW |
2013/19 |
59 |
4.1 |
0.7 |
3.1 |
5.1 |
3 |
2.313 |
0.2 |
2.22 |
6 |
|
MZ |
1999/201 5/19 |
50 |
5 |
0.8 |
3.7 |
1.715 |
1 |
2.014 |
0.2 |
2.14 |
5 |
|
NA |
11/19/20 10 |
57 |
4.3 |
0.8 |
3 |
5.2 |
3 |
11.214 |
1.1 |
2.44 |
7 |
|
NG |
1998/12/ 17-18 |
≈7910 |
2.1 |
1.8 |
1.216 |
8.8 |
5 |
1.3 |
0.1 |
2.04 |
3 |
|
RW |
2016 |
409 |
6 |
4.2 |
5.1 |
3.17 |
2 |
08 |
0 |
3.46 |
9 |
|
TZ |
2004- 05/2020 |
56 |
4.4 |
0.4 |
3.7 |
3.52 |
2 |
0.613 |
0.06 |
2.11 |
4 |
|
UG |
2002/14/ 16/19 |
≈8211 |
1.8 |
0.9 |
4.7 |
≈1.712 |
1 |
1.814 |
0.2 |
1.72 |
1 |
Table 2 Population Dental Health Index (DHI) in selected African countries around 2010-2020
1This symbol “≈“ means no national representative figure available; 250+ y; 360-69; 445 y; 5> 50y; 660y; 735 y; 840+ y; 9Mean of 2-5/6-11 y; 10Ife - Central Government Area, a suburban region; 11Nyakagyeme sub-country; 12Adults with a mean age of 54.4 year-olds attending a diabetic clinic in rural Southwestern Uganda; 1350-70+ y; 1420+ y; 1535/44 y; 1635-64 y, rural community in Udo. This value was taken because the national representative value of 0.5 (2009) was implausibly low; 17DHI= [(1)+(2)+(3)+(4)+(5)]: 5; 18Index for M-T conversion: 0-<2=1pts, 2-<4=2pts, 4-<6=3pts, 6-<8= 4pts, 8-<10=5pts, 10-<12= 6pts, 12-<14=7pts, 14-<16=8pts, 16-<18=9pts, >18=10pts.25–32
In many African countries, the prevalence rates of caries-free 5/6-year-olds are relatively high and often reach values of over 50%. Although in two cases (NG and UG) values of around 80% were found, the national representativity is uncertain and evidence for these values might only be anecdotal. Slightly lower than in the Sub-Saharan states are the caries-freedom rates in North Africa (TN, EG, MO). As assessing empirical values means making comparisons, we use corresponding figures from high-income and emerging countries as a benchmark. Compared with oral health levels of advanced countries worldwide, it is striking that the levels of caries-freedom among African preschoolers are only marginally lower than in high-income countries.18 It is also remarkable that the caries-free levels of preschoolers in low and lower middle-income countries in Africa are more elevated than caries-freedom levels in selected emerging countries worldwide.33
As some countries have no national representative data on caries-freedom in preschoolers, dmft values for 5/6- year-olds are also examined in Table 3. This enables us to consolidate our findings on the oral health status of preschoolers. The comparison between caries-freedom rates (Table 2) and dmft values (Table 3) reveals that lower caries-freedom in preschoolers leads to higher caries burden in deciduous teeth, as is evidenced particularly in Egypt, Morocco, Nigeria and Uganda.
|
Country |
Survey year |
dmft |
|
EG |
2013 |
3.31 |
|
MO |
2016/17 |
4,0 |
|
TN |
2003 |
1.7 |
|
KE |
2015 |
1.9 |
|
MZ |
2015 |
1.4 |
|
NA |
2010/11 |
1.4 |
|
NG |
2006 |
0.2 |
|
RW |
2016 |
2.8 |
|
TZ |
2020 |
1.5 |
|
UG |
2016 |
1.9 |
In general, caries experience in 12-year-old Africans is extremely low. Seven countries (TZ, EG, KE, MW, MZ, NA, UG) fall into the WHO category of very low (<1.2) caries prevalence and two (TN, NG) into the low category (<1.2-2.6).36 Only two countries (RW and MO) exhibit higher caries affection rates of 4.2 and 4.8 respectively in 12-year-olds. It is possible to observe an association between high caries-freedom in preschoolers and caries affection among 12-year-old children. Generally, the higher the caries-free rate in preschoolers the lower the caries prevalence in adolescents. The fact that the majority of African adolescents under observation show comparably low DMFT figures among 12-year-olds, as is the case in high-income countries,18 is unexpected, because most of the African nations have no or inadequate preventive programmes for the young generation.37 Surely, the different dietary habits play a role: on the one hand a traditional diet with few sugars and, on the other, a much more cariogenic diet in high-income countries. However, in the case of adolescents living in high-income countries, the more cariogenic diet is largely offset by training in good oral habits and protective preventive measures (e.g. fluoride varnish, mouth rinsing, fissure sealants, regular dental checkups). To this extent, the initial position of adolescents in both country-types with respect to their future dental health career is more or less equal (except for adolescents living in Morocco and Rwanda). However, it is disadvantageous for African adolescents as professional dental care is hardly available and often not sought as a lack of oral health education has led to insufficient oral literacy. Another noticeable fact is that, in Nigeria´s younger generation below the age of 21 years, around 80% of carious permanent teeth are only affected by pit and fissure lesions,32 although another study concluded that almost half of the caries-affected 12-year-olds had deep caries.39 Both forms of caries regularly remain untreated in all of the African countries studied.15,16,34 In summary, it can be said that the oral disease burden of the young generation, caries prevalence, severity and progression is very low among preschoolers and adolescents in the majority of African countries, except for Morocco and Rwanda. Apart from a small amount of oral hygiene promotion in some countries (EG, MZ, NA, NG, TZ), fluoride varnish for children at risk (EG)40 and a programme for schoolchildren (TN),41 this result was achieved more or less without the support of dental services and with only rudimentary oral hygiene. The result is amazing.
Ranging from 50% (MW)42 to 94% (EG),43 caries prevalence in middle-aged Africans can be considered widespread, but its severity, measured by DMFT, is extremely low with the exception of Morocco (DMFT:14.9), where the hitherto documented higher single values among the young generation further increased the pace of caries increment into the middle-aged generation. Overall, caries progression, except in Morocco, is rather slow and the caries level in middle-aged Africans is significantly lower than in high-income countries with advanced dental care systems.18 Even the highest value for Morocco is in line with the highest DMFT value for Denmark: (2008:13.5), which belongs to the above-mentioned high-income country-group.25 Considering that poor oral health awareness, a lack of access to dental care facilities for large sections of the population and high treatment costs, mean that, in Africa, even in young adults, decayed and periodontally damaged teeth usually remain untreated, this result is not readily explained. We will return to this problem at a later stage. However, at this point in our analysis we must acknowledge that, although the DMFT indices in both country-groups are at a similar level, the reality behind the DMFT values, is fundamentally different. In the African countries the main component of the DMFT index is the D-component and the F-component is near zero, whereas in the well- developed industrialised countries, the D-component is almost zero and the F-component is highest. The M- component is lowest in Kenya and lies between 0.7 and 2.2 in most of the other countries (Figure 1), a level that is also known from high-income countries. Only Morocco exhibits extremely elevated levels of tooth loss, and this already in the middle-aged generation.
As in the low and lower middle-income African countries most decayed cavities remain untreated and around the age of 20 a new and frequent oral disorder, periodontal disease, appears and develops exponentially until it peaks at about 55 years before slowing down,9 it is important to know the additional burden caused by this disease. From that age on, both diseases accumulate and intensify. This raises the risk of tooth loss considerably. Figure 2 shows the prevalence of severe periodontitis in the African countries studied, because only severe periodontitis is a public health concern.9 As only a few countries offer current and nationally representative periodontal data for 35/44-year-olds, we can document only a few countries. Middle-aged people in Egypt and Namibia are only marginally affected by severe periodontitis (3%), whereas among the citizens of Mozambique (7%) and Tanzania (9.2%) slightly higher affection rates were found. These findings correspond to those of high-income countries like Denmark, Japan and Germany with values of 6%, 5%, and 10.4%, respectively.25,44 Although periodontally damaged teeth, too, are regularly not treated in African states, the severe periodontitis burden among Africa´s middle-aged is not higher than in high-income societies. On the contrary, the level of affection is even slightly lower. Comparable to caries prevalence in African countries, which is generally high but not severe, a similar picture emerges concerning the morbidity structure of periodontal diseases. Exemplified in the Tanzanian data, gingivitis and shallow pockets account for 90% of the periodontal burden but serious destruction, requiring treatment, occurs in only 9% of cases.16 The corresponding figures for the CPI grades 1-3 in the other countries, shown in Figure 2, are in the same prevalence range of 73% to 93%,25 but the rates of severe periodontitis (CPI 4) are more moderate. We suggest that these few results can be taken representatively for the rest of the African countries studied. This finding, again, is remarkable as one would have expected higher affection rates of severe periodontitis in Africa in the light of frequent early-onset periodontal diseases, mainly due to a lack of oral hygiene habits and untreated periodontal disorders.
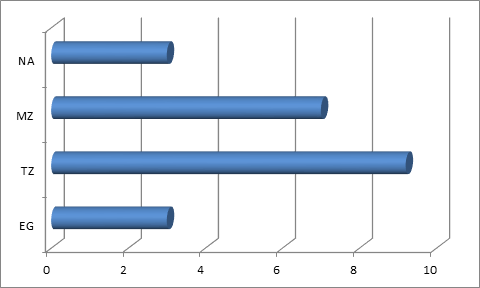
Figure 2 Severe periodontitis (CPI 4, in %)1 1 in 35/44-year-olds in selected African societies 2010-2020.
1Community Periodontal Index (CPI), grade 4: periodontal pockets ≥ 6 mm.25
Regarding the further development of oral health into older age, Table 2 reveals that the demographically young African societies41 exhibit very low numbers of missing teeth in 65/74-year-olds. Only in Tunisia and Nigeria are the MT indices more elevated, with 15.8 and 8.8 missing teeth, respectively. However, it should be noted, that data sources for the global oral data base on tooth loss in seniors are particularly scarce. Therefore, non-national representative material also had to be used. Thus, for example, the M-T value for Moroccan seniors (3.9) is implausibly low, as the corresponding figure for middle-aged already reached a value of M-T 7. Consequently, any interpretation of the results must be conducted with great caution. Nevertheless, some countries offered data for older adults/seniors in their national oral health surveys (e.g. MW, TZ, NA, RW), giving us at least an approximate picture of tooth loss in African seniors which ranges from 1.6 to 5.4 missing teeth. That level is very low compared with high-income countries,18 and more so compared with emerging countries.33
Particularly fragmentary are the epidemiological data on edentulism in seniors. Some national surveys do not even contain a chapter on edentulous elderly. In one survey, it was stated that no edentulous seniors were found.15 In some cases, random sample aspects such as insufficient numbers of probands in these young African societies meant that seniors could not be included in the surveys.15 The Arabic-speaking countries, Tunisia and Morocco, exhibit the highest rates of edentulism with 32% and 20.6%, respectively (Table 2). In the case of Morocco, this result can already be observed in the generation of 50 years and above. Namibia also reveals a higher level of edentulism (11.2%) compared with the majority of the countries, which ranged from only 0% (RW) to 7.8% (EG). The finding of 57.5% edentulous 35/44-year-olds in Mozambique (2015), as documented by the Global Oral Data Bank (GODB)25 and similarly reported by Domingos et al.,45 is not considered here given the other figures reported for Mozambique (especially the low MT of 1.7 in that age group). Furthermore, an edentulism rate of 16% already in 18-year-olds, as stated by the GODB, seems hardly likely. These two values seem implausible and are documented without any explanation as to possible outliers. Moreover, as another, more recent WHO-resource for edentulism in adults in Mozambique aged 20+, the ‘Oral Health Country Profiles 2022‘, put the value at 2.0%46 (Table 2), we decided to use this figure here. Nevertheless, Domingos et al. might be correct in stating that, due to very scarce epidemiological data on edentulism in seniors, it is hardly possible to present the complete panorama of oral health in this country.45
The results from Cameroon (1.4%) match the generally low rates of edentulism in African seniors.47 These values from the Sub-Saharan countries are surprisingly low when compared with the two highly affected Arab African countries (TN, MO). Apart from the latter two countries, most African societies studied show lower levels of edentulism in seniors compared with emerging33 and high-income countries,18 a highly unexpected result.
After examining the single values for the different age-groups within African societies, we regard the composite indicator, the DHI, which measures the oral health status of the entire population. The DHI values show dichotomous results: very low DHIs (1.7-3.5) in Sub-Saharan Africa and Egypt, indicating a low burden of oral diseases and comparatively better oral health and, on the other hand, the two North African countries (TN, MO) exhibiting higher DHIs (4.8-6.2) and thus occupying the last ranks (10 and 11) in our comparison. What is striking is that, although they rank higher on the Human Development Index, enjoy a higher level of urbanisation and possess a larger middle-class (Table 1), both Arab North African countries rank lower than the countries of Sub-Saharan Africa. Inside Sub-Saharan Africa, the lower middle-income countries of Uganda, Kenya and Nigeria achieved the best DHIs and, consequently, rank first, second and third. Fourth place is taken by Tanzania and the fifth and sixth go to Mozambique and Malawi, two low-income countries. The only upper middle-income country, Namibia, ranks seventh. What is also remarkable is that the performance of countries that are still at a low development stage (RW, MZ, MW) is comparable to that of lower middle-income countries. Comparing the DHI results of the African countries (1.7-6.2) with those of societies in emerging (3.3-7.4)33 and high-income countries (2.6-4.8),18 the values for African societies look more favourable at first glance, which is surprising. However, it is necessary to take into account that the DHI is an instrument that measures the degree to which natural teeth have been retained up to old age, meaning that tooth replacement is not considered. Indeed, tooth replacement rates in Sub-Saharan Africa are completely different from those in advanced European countries. While in Africa denture wearers account for between 3% and 18% on average47,48 the rate of replacement in European countries is much higher49 reaching 40% of 35/44-year-olds and 82% of 65/74-year- olds in Germany,44 for example.
A rougher comparison, done by WHO,9 compared the development of caries prevalence in primary and permanent teeth, severe periodontitis and edentulism, from 1990 to 2019 in the six WHO regions, whereby only the African, Eastern Mediterranean and European regions are of interest here. This longitudinal study allows us to check whether our analysis is in line with these regional findings and get an idea of how oral health in the regions has performed in the last three decades. In 2019, the prevalence level of primary caries in the African region was relevantly lower than in the three Arab North-African states and even slightly lower than in the European region (Table 4). Over the last thirty years, primary caries dropped by -3.4% in Sub-Saharan Africa, while it increased by 0.6% in the three North African states. The European region witnessed a sharp reduction of -7.6%, possibly as a consequence of the oral health policies implemented in those countries. Furthermore, the frequency of caries in permanent teeth is lower in the African region than in the Eastern-Mediterranean and European regions, both of which have similarly high prevalence rates. A comparison with 1990 percentages shows small reductions in all three regions. The prevalence of severe periodontitis is highest in the African region while the Eastern-Mediterranean and European regions exhibit prevalence rates that are almost identical to each other. In all three regions, the percentage change compared with 1990 is positive, but it is lowest in Sub- Saharan Africa (2.5%). This is in contrast to a rate that is four times higher in North Africa and more than six times higher in the European region (Table 4). The edentulism rates diverge the most in terms of the level and the percentage change. The level of edentulism in both parts of Africa is less than half that of the European region. Furthermore, in terms of percentage change, the trends are totally reversed: edentulism decreases sharply in the African and slightly in the Eastern-Mediterranean region, whereas it rises strongly in the European region (Table 4). However, these unfavourable figures for the European region are biased by the results from the countries of Eastern Europe, as these still do not offer satisfactory oral health conditions. If edentulism is considered in persons over 60 years, the prevalence rates for edentulism are globally higher (22.7%), whereas the African region shows an average rate of 12.1%, and North Africa values ranging from 26.2% to 34.1%.9 All of these developments occurred in a period when population growth in the African and Eastern-Mediterranean regions was 115% and 94%, respectively. In contrast, population growth in the European region was only 10% at that time. Therefore, an important reason for the significant rise in the rates of severe periodontitis and edentulism in the European region, might be the rapid ageing of European societies.
|
WHO Region |
Caries, primary teeth (%) |
%-∆ (1990-2019) |
Caries, permanent teeth |
%-∆ (1990-2019) |
Severe periodontitis1 (%) |
%-∆ (1990-2019) |
Edentulism2 (%) |
%-∆ (1990-2019) |
Population %-∆ (1990-2019) |
|
African |
38.6 |
-3.4 |
28.5 |
-1.66 |
22.8 |
2.47 |
3.3 |
-11.75 |
115 |
|
Eastern-Mediterranean |
45.1 |
0.6 |
32.3 |
-0.27 |
17.3 |
10.42 |
5.9 |
-2.75 |
94 |
|
European |
39.6 |
-7.2 |
33.6 |
-3.91 |
17.9 |
16.13 |
12.4 |
8.95 |
10 |
|
Global |
42.7 |
-3.3 |
28.7 |
-2.59 |
18.2 |
23.96 |
6.8 |
8.02 |
45 |
Table 4 Estimated prevalence of caries in primary and permanent teeth, severe periodontitis and edentulism in 2019 versus 1990 by selected WHO region
1Ages > 15 years; 2. Ages > 20 years.9
The global WHO study confirms by and large our surprising findings on lower caries affection in young and middle-aged African adults and much less edentulism in seniors, although large sections of African societies are characterised by a lack of awareness of oral health, neglected oral hygiene and the widespread absence of professional care. The longitudinal results underline our time-point related essential findings and insights in the presence of oral health differences between African, emerging and high-income countries that are difficult to explain. Unfortunately, the WHO study does not offer explanatory statements or possible reasons for the great disparities and often unexpected results that are brought to light by comparing country types at different development stages and by comparing epidemiological findings with theoretical knowledge in dentistry. While other global studies, focusing on the prevalence of untreated oral conditions, come to the conclusion that the highest normative need for dental procedures is found in low and lower middle-income countries10, this result is consistent and does not contradict our findings.
To identify possible reasons why empirical results on oral health in African societies conflict with theoretical dental knowledge, Table 5 offers facts that might explain why the oral health situation in Africa differs so much from other regions of the world. One of the points to be highlighted is the extreme paucity of dentists in these populations, particularly when one considers that these few dentists practice predominantly in urban areas. As only four countries (TN, MO, NA, NG) have an urbanisation grade of >50% (Table 1), large parts of the population live in the countryside and in remote areas. Here, people have almost no access to dental services. Even in urban and peri-urban regions, the uptake of dental services is very low and, if at all, generally, occurs only when pain is a motivating factor. It is conspicuous that owing to what is largely a lack of oral health awareness, even among many urban citizens, this behaviour is also found in countries where dental treatment is partially covered (TN, MO, NA, MZ) by health insurance (Table 6). When treatment is offered, it mostly consists of tooth extraction. Tooth brushing habits are poor, whereby it should be noted that the representativeness of these data is limited and they reflect no more than tendencies. The frequent use of chewing sticks, which are supposed to be as effective as manual toothbrushes, among older adults in many African rural communities (e.g. UG and NA) is also noteworthy.49 Some Muslims prefer chewing sticks as Mohammed recommended them for cleaning the teeth.51 Two single-blind, randomized studies comparing the effectiveness of fluoridated chewing sticks and toothbrushing with fluoridated toothpaste revealed comparable plaque removal and F-concentration in saliva, so that WHO recommends both methods as customary oral hygiene tools in developing countries.52,53
|
Country |
Dentists/10,000 people |
Dental visits/year (%) |
Tooth brushing + toothpaste≥ twice/day (%) |
Sugar consume/ capita (g/day) |
Smokers (%) |
Naturally fluoridated water (%) |
Existing oral health policy and goals |
|
EG |
2 |
52 |
104 |
70.9 |
24.4 |
10014 |
in preparation |
|
MO |
1.4 |
134,6 |
725 |
91.8 |
14.9 |
Yes16 |
yes |
|
TN |
3.0 |
no data |
no data |
90.6 |
25.0 |
Yes17 |
yes |
|
KE |
0.2 |
307 |
808 |
47.3 |
11.5 |
X18 |
yes |
|
MW |
0.1 |
no data |
753 |
15.4 |
11.3 |
10019 |
yes |
|
MZ |
0.1 |
689 |
6310 |
34.0 |
14.8 |
3520 |
yes |
|
NA |
0.7 |
no data |
no data |
62.4 |
15.5 |
7921 |
yes |
|
NG |
0.2 |
no data |
5013 |
27.0 |
3.9 |
8315 |
yes |
|
RW |
0.2 |
16 |
64 |
25.8 |
14.1 |
X22 |
yes |
|
TZ |
0.1 |
111 |
472 |
32.0 |
9.2 |
Yes23 |
in preparation |
|
UG |
0.1 |
1011 |
9912 |
31.0 |
8.9 |
Yes24 |
yes |
Table 5 Dental infrastructure and oral care habits among adults in selected low and lower middle-income African countries around 2020
1Check-ups: 1.8%; 284% once/day; 343% with F-toothpaste; 4once/day: 15%; 5Academic population, mean age 20 years; 613% periodically, the rest only in case of pain; 7Check-up: 3%; 8Thereof 70% using F-toothpaste; 912-year- olds; thereof 37% follow up/check-up; 1012-year-olds; 11Diabetic patients , mean age 54, routine dental check-up; 7%; 12Once/day, toothbrush use: 10%, mostly wooden tooth pick, toothpaste use: 16%; 13Rural adults, mean age 36, toothbrush use: 50%; 14Mostly in the range of 0.113- 0.452 mg/L. Maximum value: 0.8 mg/L.; 1521% of the country was in the optimal range for hot and dry regions of 0.3-0.6 ppm and in 62 % below that range; 16Mean fluoride concentration: 0.94 mg/L. Much higher values were found in phosphate regions (e.g. Khouribga), meaning fluoride concentration exceeds the Morocco limit (0.7 mg/L.9) in parts of the country; 17Average F concentration is 0.1 mg/L, only Southern Tunisia exceeds the national limit (0.914 mg/L.) with > 2mg/L; 18Country with excess intake of fluoride (> 1.5 mg/L.) in large parts, causing dental and skeletal fluorosis; 1983% below 1,5 mg/L, 17% in the range 1.5-> 6 mg/L.; 20Average F concentration nationwide: 0.14 mg/L; 21F concentration < 1.5 mg/L. 8% of the population is at risk due to F concentration above the WHO limit of 1.5 mg/l; 22Excess intake of fluoride only in a small part of RW (Gihaya Island), causing fluorosis in 91% of children. National level of fluorosis: 6%; 23Northern Tanzania: > 1.5-13.6 mg/L.; Southern Tanzania: 0.741-1.450 mg/L., West Tanzania: o-0.12 mg/L; 246.5% of water sources exceed the limit of 1.5 mg/L F (average: 3.3mg/L F).16,25,28,39,46,54–71
|
Procedures for detecting, managing and treating oral diseases in primary care facilities: |
EG |
MO |
TN |
KE |
MW |
MZ |
NA |
NG |
RW |
TZ |
UG |
|
- Screening for early detection of diseases |
yes1 |
yes |
yes |
no |
yes |
yes |
yes |
no |
yes |
yes |
no |
|
- Emergency care and pain relief |
- |
yes |
yes |
no |
yes |
yes |
yes |
no |
yes |
yes |
no |
|
- Basic procedures to treat manifest caries |
- |
yes |
yes |
no |
yes |
no |
no |
no |
yes |
yes |
no |
|
Oral health interventions as part of benefit packages: |
|
|
|
|
|
|
|
|
|
|
|
|
- Coverage of the largest government financing scheme (% of population) |
In preparation |
60 |
72 |
17 |
- |
60 |
90 |
4 |
85 |
- |
- |
|
- Routine and preventive care |
yes2 |
yes |
yes |
- |
yes |
yes |
no |
yes |
yes |
no |
- |
|
- Essential curative care |
- |
no |
yes |
- |
yes |
yes |
yes |
no |
yes |
no |
- |
|
- Advanced curative care |
- |
no |
yes |
- |
no |
no |
no |
no |
yes |
no |
- |
|
- Rehabilitation care |
- |
no |
yes |
- |
no |
no |
yes |
no |
no |
no |
- |
Table 6 Dental care system characteristics in selected African countries 2021
1Promotion of oral hygiene measures and first dental visit by 12 months of age; fluoride varnish for children at risk.
2Detecting and treating oral and gum diseases free of charge for all age groups in six governorates as a first stage.40,46,79
Regarding sugar consumption, by far the highest values are found in Morocco, Tunisia and Egypt (Table 5). In the case of Egypt and Tunisia, this is also true for smoking rates in the African countries studied. The elevated sugar intake and smoking rates contribute to the high DHI values exhibited by these two North African countries (EG, TN, Table 5). The protective effect of naturally fluoridated water in both countries cannot compensate for these two harmful habits. In general, water fluoridation in African countries is a double-edged sword as the line between fluoride tolerance and fluoride toxicity is slim.54 In low concentration (0.5-1.0 mg/L) fluoride is healthy for bones and teeth but in concentrations >1.5 mg/L it can cause dental and skeletal fluorosis, which is frequently observed in East African countries like Tanzania, Uganda, Kenya, Nigeria and Malawi, as a result of volcanic activity in the Rift Valley.55 Most often, poor people living in remote areas are affected by the consumption of water containing F ≥ 2.5 mg/L (Table 5), which causes serious levels of fluorosis.
That is why fluoride exposure in most African countries is suboptimal and unable to unfold its protective effects against caries. Alternative measures could be defluoridation techniques at community level or at the point-of- use.57 As long as it is not possible to safely control the F-content of drinking water, it is unjustifiable to recommend water fluoridation. An alternative would be bottled drinking water, with the optimal fluoride content for tropical countries of 0.3-0.6 ppm, which also considers other sources of fluoride intake.56,57 To be on the safe side, the authors propose studies to determine the appropriate F-concentration in each of the different countries. Our examination of oral health awareness and habits, as well as the access to and use of dental care by African citizens, has led us to conclude that, together, these factors fail to explain the surprising findings uncovered by our investigation into African oral health, which can be summarised as follows:
Although in most African countries caries and periodontal disorders are generally not treated and, if they are, only by extraction and prescription, the severity of oral diseases, measured by DMFT and CPI 4, is lower than in high-income countries. Moreover, the long-term consequences of both diseases, tooth loss and edentulism in middle-aged persons and seniors, are much lower than in affluent societies.
These results were achieved, despite a decades-long paucity of dental professional services across large sections of African societies, combined with widely ignored oral self-care. According to dental theory, the consequences of such behaviour would result in a much greater magnitude of tooth loss in younger adults and higher levels of edentulism in old age. However, this is not what has been observed in Sub-Saharan Africa and the Arab state of Egypt. Only in the other two North African states of Morocco and Tunisia, are the findings by and large in accordance with theoretical knowledge of dentistry. As predominant causes for these divergent findings between African reality and dental theory, only dietary and genetic factors remain. Despite very low average cosumption of vegetables and fruits in Sub-Saharan countries, measured against the WHO recommendation of at least 400 g/day/person,72,73 the negligibly cariogenic traditional African diet, which is low in fermentable carbohydrates74 and low in sugar, might help to keep the oral disease burden low. On the other hand, the more cariogenic processed and animal-based ‘high-sugar food‘70 consumed in affluent societies is largely neutralised by satisfactory oral hygiene habits, sufficient fluoride exposure and frequent utilisation of dental services. As these protective measures are lacking in Africa, dietary habits probably even go a longer way to explaining a significant proportion of the differential in dental status between Africans and citizens of affluent societies or the difference between African reality and dental theory. The last remaining possibility is that of genetic influences that might lead to greater resilience among African citizens in the face of bacterial attacks on teeth and periodontium. However, some of the Sub-Saharan African populations suffer from protein-energy malnutrition, vitamin deficiencies and several endemic communicable diseases (e.g. malaria, tuberculosis, HIV/AIDS),8 which weaken the immune-system. These facts seem to contradict our genetic hypothesis. As, to date, little research has been done to understand the genetic basis of oral diseases in Africans,1 this hypothesis remains simply that. The argumentation of Tantawi et al., that affluent societies are exposed to higher risk factors which are not matched by adequate institutional preventive measures and practices,75 might touch on an important point, in so far as in high-income countries teeth are often prematurely extracted although they might have been saved by adequate tooth-retaining procedures. This interpretation further contributes to explaining the great differential in dental status between Africans and the inhabitants of high-income countries. Nevertheless, dietary factors and the latter arguments cannot fully explain the low oral degradation and the comparatively low negative consequences that untreated oral diseases have on oral health status in African countries.
In the last decade, many African countries discovered oral health as the blind spot of their health policy and, consequently, designed dental care systems and strategies (Table 6) which are still in their infancy. These initiatives show how dedicated and ambitious the individual government efforts have been in the meantime. Astoundingly, an analysis of their plans and priorities reveals that many of them seem to follow dental care models from high-income countries and intend to offer everything at the same time. Such an approach will certainly overburden economies plagued by limited human, financial and physical resources. For example, if the overall objective of a dental care system is comprehensively defined as follows: ‘to render integrated, affordable, accessible, and quality preventive, curative and rehabilitative oral health care service that is responsive to the needs of the population,‘76 which is, in similar words, also the case in Tanzania, Malawi, and Rwanda,56,77,78 it is clear that all of these goals cannot be achieved simultaneously in the foreseeable future. It will be necessary to set priorities, tackle serious problems in the most underserved parts of the population first and concentrate the limited resources on these fields of action.
The mere adoption of the Western model of oral care is likely to fail in Africa, because it is not appropriate to African circumstances. These models are characterised by a predominance of dentists, working in private practice and pursuing a treatment-oriented, reparative approach.80,81 Simply educating many additional dentists is also not a solution for Africa.14 Training dentists is a lengthy process (at least six years), the output from African dental schools is very small and the training itself is very expensive. Therefore, finding an alternative model for oral care provision in African societies is vital.
This alternative must be able to reduce the prevalence of dental decay and gum diseases and gradually diminish the accumulated bulk of treatment-need, caused by non-treatment in the past, in these rapidly growing young African societies. This must happen on a large scale and in a sustainable and financially viable manner. For this purpose, three core tasks must be tackled:
These three overarching tasks influence each other. The chances of implementing such structures are promising, as all essential segments can be created almost in the open countryside. The African countries, studied here, can adopt the newest evidence-based methods from advanced dental care systems, and tailor them to meet African specificities, without having to overcome a great deal of resistance from vested professional interests. The favourable morbidity-structure (disorders often in the early stages, mostly not severe and progressing very slowly) and the extremely young population (almost 50% is under 20 years old),40 which is generally more innovative and open-minded than fast- ageing societies, should facilitate the achievement of these proposals. Should they be successful, these African countries could even raise the bar for the long-term re-orienting of oral care provision into a truly preventive and tooth-retaining future. Such a future will bring better oral outcomes and will be, in the long run, considerably less resource-intensive than the oral care systems in countries of the old world, where 5% to 6%, in Germany even nearly 8% of GDP, are spent on dental 18,84 Furthermore, the paradigm-shift to a consistently prevention-oriented form of dental provision in those countries, where the modern preventive approach was invented, is proceeding very sluggishly. Africa has the opportunity to implement that approach on a community-centred basis faster than the old world. This might sound odd, considering Africa´s general difficulties in many aspects, but it is not.
The priority group for health education and training should be the young generation up to 20 years of age, which accounts for about half of the entire populace. If this education is successful, the habits thereby engrained should last for a life-time and build a protective barrier against the continuous change to more cariogenic dietary habits resulting from material prosperity. According to modern dental knowledge, most of the main oral disorders (caries, gum diseases) are preventable14,85 by relatively simple procedures and appropriate behavioural attitudes on the part of citizens. From the population´s perspective, the necessary key habit would be toothbrushing at least twice a day after meals, if possible with fluoridated toothpaste. As oral health awareness, a requirement for oral hygiene activities, is often not present in rural African societies, this consciousness will first have to be ignited by countrywide activities and educational measures. These activities should start with mothers during pregnancy and after childbirth and should be integrated into the toddler´s regular general early detection examinations. Such an approach would require additional dental training for the nurses/paediatricians conducting the check-ups, if a dental nurse is not present. This will allow family physician services to also provide counselling on oral hygiene, diet and fluoride supplementation.85 Similarly, adults should also be educated in oral hygiene and the corresponding habits they need to adopt. Therefore, dental nurses or other dental workers should regularly instruct the population on a community and village level. When children reach school age, school-based interventions and instructions, carried out by trained teachers, dental nurses or trained school dental care aides (mostly housewives and mothers, like in Switzerland)86 have been shown to be very effective as proven by myriad examples from lower middle-income countries.87,88
In the context of oral care habits, it would be important the ensure sufficient fluoride exposure to protect dentition against caries attacks by cariogenic foods and drinks, particularly because this method is very effective and inexpensive and can help to attenuate income-related and geographic inequalities. Furthermore, its benefits are most pronounced in deciduous teeth.89 However, as it must also be guaranteed that the naturally fluoridated drinking water is safely controlled and delivered with an optimal F-concentration, it would be worthwhile to lay the foundations for using this population-wide measure.
On the supply side of dental care, the enormous scarcity of dental personnel, primarily in rural areas where the majority of Africans live, cannot be ignored. In addition to poor oral health awareness, the general lack of dental services in the countryside and the costs of treatment are the main causes for the serious under-utilisation of oral care. Surely, the resulting treatment-need gap in African states cannot be met by training additional dentists.14,81 This would overlook the prevailing African customes and circumstances which differ fundamentally from European or American attitudes and available material and financial resources for oral care. Incidentally, educating dentists, who prefer working in private practice located in urban settings, is very costly and time- consuming and, considering the low output rates of the few existing African dental schools, not a constructive endeavour capable of solving the problem in the foreseeable future. Furthermore, dentists are not essential for most of the primary oral health services needed. The specific morbidity structure of oral disorders in Africa, a high prevalence of caries and gingivitis/periodontitis, but mostly in early stages with relatively few consequences in terms of tooth loss and edentulism, requires few dentists but a large number of MLPs who can be trained in a comparatively short period of time. Ninety percent of the necessary oral treatments provided for rural and poor citizens in developing countries consist of pain relief, which is predominantly achieved by tooth extraction.90 Dentists in clinics complain that patients do not request filling treatment. Consequently, the low demand for saving decayed teeth often does not justify the presence of a dentist.90 Furthermore, in rural sub-district centres and village health posts dentists are not necessary as the required treatments can be performed by well-trained MLPs.90
These persons, who already conduct oral health promotion, should be further trained to also provide atraumatic restorative treatment (ART). Several studies from all over the world, demonstrated that, particularly in developing countries, such well-trained mid-level cadres (e.g. dental therapists/hygienists) produce very satisfying treatment results in the area of primary oral health care.91–93 In underserved communities in the old world, too, this group of personnel produced positive and cost-effective outcomes.94 Consequently, in its Oral Health Action Plan (2023-2030), WHO recommends the implementation of new skill-mixes in oral health provision and advocates for MLPs to have greater autonomy in their work.95 MLP concepts have been designed for Vietnam90 and for Cameroon.96 In Cameroon, such a concept is practiced by the largest provider of oral health services in the country, a private, non-profit organisation which has been running 10 clinics in six of the 10 Cameroon regions for a long time. There, over 90% of almost the full scope of dental treatments (extractions, fillings, root canals, cleanings and most dentures) are provided by MLPs at the same quality level as dentists.96 A few dentists focus on complex procedures (e.g. facial injuries) and on teaching intermediate providers. The ratio of dentists to MLPs in this well-functioning provider model is 4 to 42.96 However, this example also demonstrates how difficult it is, even in Africa, to institutionalise such a model. Although the Cameroon government had recognised the affiliated training school for MLPs, as early as 2012, the institution was unable to obtain a license to educate MLPs from the Cameroon National Dental Council. There are also other African countries (EG, MW, MZ, NG, TZ) where noteworthy ratios of dentists to MLPs (1:1.3) can be observed.97 However, compared with the Cameroon model, task shifting in those countries is still insufficient. In a technical paper, WHO recently proposed a rough threshold of 1:8 dentists/MLPs as an optimal skill mix for dental professionals with a view to attaining Universal Health Coverage in Africa.98 In addition to this, the fact that countries like Tanzania56 and Malawi77 have published oral health guidelines that explicitly state that mixed dental teams, particularly those including MLP´s, should be formed to serve the population, indicates an urgent need to establish or enlarge schools for training MLP´s instead of educating more dentists.96
As MLPs often work in rural and remote areas, they might sometimes need advice from centrally located dentists. This could be enabled by establishing teledentistry (TD) via the internet, computers and mobile phones.
Although, digital connectivity in Sub-Saharan Africa is low and access to mobile phones and electricity is higher than access to the internet and computers,99 MLPs should, to the extent possible, have access to this modern tool that makes it possible to overcome the limiting factors of time, distance and manpower. TD allows access to underserved people in remote areas, enables diagnosis and the recommendation of treatments in difficult cases, enhances care quality and facilitates the dental education of ancillary personnel.100 TD has demonstrated its applicability in high-income as well as emerging countries and across different patient groups.101 The feasibility of MLPs treating oral lesions via images transmitted by email was evidenced by studies from Brazil and the USA.102,103 Especially the American approach, where several dental therapists/hygienists perform their primary oral care duties while digitally linked to a sometimes distant dental clinic or a dentist´s practice, could be a perfect model for the large rural areas of Sub-Saharan Africa. Tantawi et al. give a detailed overview of the teledentistry models in place in African countries.104 A fact sheet on evidence-based TD from the World Dental Federation (FDI) explicitly features the societal benefits of TD in underserved regions105 and the newest summary of knowledge on TD, published by Goffin et al., sees the main advantage of TD ‘in expanding the reach of care,‘106 which is so decisive for Africa. African researchers also advocate for implementing TD to improve oral health assistance in rural and remote areas.107
In keeping with African oral morbidity-structures, the currently prevailing attitudes of African citizens towards oral health and the obtaining socioeconomic and cultural conditions, combined with very limited financial resources, a primary oral health concept (POHC), practised on a community-centred basis and bolstered by a strong public health sector, is the only promising approach to serve the African people with dental services in a sustainable manner. This conclusion was expressed already two decades ago by researchers and WHO.90,108,109 Our detailed and country-specific study supports that perception and suggests complementing that approach by an active, future-oriented preventive component, specifically targeting the young generation, which will soon determine the destinies of African countries. Expanding the POHC system to include a preventive and strictly tooth-retaining component is urgent, as a gradually rising standard of living leads to life-style changes and shifts in dietary habits to more cariogenic, ultra-processed and animal-based110 ‘civilized‘ foods and drinks.70 This could result in higher caries rates and more severe degradation of dentition. Furthermore, a high, unchanged prevalence of oral disorders combined with a rapidly growing population will put added pressure on the health systems of African countries.13 In short, a relevant deterioration of oral health status might occur in the future if no measures to counter this are implemented. Such measures could comprise the activation of oral self-care and preventive support from dental services, meaning that modern preventive dentistry with minimal intervention practices10 must be integrated in a feasible manner into the primary oral care approach. Minimal intervention dentistry (MID) aims to intercept oral diseases at an early stage111 and comprises ART techniques112 as well as silver diamine fluoride.113 As the preventive MID-approach does not require expensive equipment, treatment costs shrink considerably.10 Thus, according to our definition, both components would be promising building blocks for a modern, Africa-adjusted oral health system. Although most of the main oral disorders (caries, gum diseases) are preventable with the aid of relatively simple procedures and appropriate behavioural attitudes, such a system - which integrates modern dental knowledge - would gradually compensate for past omissions and simultaneously lay the foundations of a better oral health future for African societies, beginning with the young generation. African researchers, too, recommend including prevention into the basic POHC system.74,114
As the primary oral health care system has been described elsewhere,115–116 only the new preventive elements of the proposed Africa-adjusted system are outlined here. First and foremost, it would need to be legally constituted and codified in guidelines so that public and private providers of oral health are obliged to adopt a preventive and tooth-retaining approach. This objective should also apply to the curricula of dental schools. Without changing the curricula in that direction, it will not be possible to achieve a paradigm shift in dental training, away from restoration-oriented teaching, which prepares dentists for individual work in private practices (the current situation), to preventive and tooth-retaining training for practice in community-centred settings, integrated into dental public health services.114,115,117
The paradigm shift to preventive and community-based primary oral health care, if possible integrated into general primary health care, requires strong political leadership and, in the light of the extreme scarcity of resources, will be constrained to strict priority-setting in the three above-mentioned cornerstones of oral health. To obtain financial, personnel and technical expertise in these key fields of reform, North-South partnerships, South-South cooperation schemes (e.g. in the training of dental personnel)118 and private/public partnerships (PPPs) between African public health structures and socially engaged multinationals from the dental and information technology sector that can facilitate teledentistry, should be envisaged. Successful partnerships in these fields exist and can serve as good practice examples.119–123 For Aggarval, PPP´s in developing countries might even be ‘the new panacea in oral health.‘124
If African countries concentrate their limited resources on a few vital segments of oral health, the chances of gradually improving the oral health status of large sections of the population are promising. Priority should be given to the young generation. The three key action fields could be summarised as: mobilising oral self-care, enlarging the dental workforce by training sufficient MLPs and creating a true primary oral health care system which is community-centred, guided by a strong public sector and expanded to include strictly preventive, minimally invasive and tooth-retaining treatments.
Once again, I am greatly indebted to my former colleague Erica Long-Michalke for polishing the English text.
The author declares that there are no conflicts of interest.

©2024 Saekel. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.