Journal of
eISSN: 2373-4345


Case Report Volume 10 Issue 6
1Dental Department, King Saud University Medical City, Saudi Arabia
2Department of Preventive Dentistry, Alrass Dental College, Qassim University, Saudi Arabia
Correspondence:
Received: November 22, 2019 | Published: December 2, 2019
Citation: Aldayel AM, Alfawzan AA. Management of class II div.2 malocclusion using TADs supported frog appliance. J Dent Health Oral Disord Ther. 2019;10(6):331-336. DOI: 10.15406/jdhodt.2019.10.00507
This case report describes the effect of Temporary Anchorage Devices Supported Frog Appliance on Class II div.2. The use of miniscrews supported distalizer minimized unwanted teeth movement while distalizing maxillary molars and reduce the need of patient compliance. The design of appliance and treatment steps were demonstrated in this case report. Case selection is an important factor of molar distaliztion and achieving planed result.
Keywords: miniscrews, distalizer, class II div.2, anchorage, molar distalization
Class II malocclusion is one of the most common cases present in the orthodontic clinics. The prevalence of class II malocclusion in Saudi population is 16.4%.1 Clinical features of Class II Div.2 malocclusion include: mandibular retrognathism rather than maxillary prognathism, horizontal growth pattern, skeletal deep bite, retroclination of upper incisors and prominent soft tissue chin.2‒5 The treatment of this type of malocclusion depends on the severity of sagittal discrepancy, patient cooperation, and growth period of the patient. The treatment options include growth modification, orthodontic camouflage or orthognathic surgery. Camouflage can be done by extraction of premolars or maxillary molars distalization. Many techniques have been used for molar distalization.6,7 Intraoral noncompliance appliances are preferred nowadays because they reduce the need of patient cooperation. The use of Temporary Anchorage Devices (TADs) preferred to minimized unwanted teeth movement while achieving the planed teeth movement and reduce the need of patient compliance.8,9 The present case report illustrates management of Class II Div.2 malocclusion using TADs supported Frog appliance.
Diagnosis and Etiology
A 19-year-old girl was referred to orthodontic clinic with a chief complaint “I can't show my smile as my front teeth aren't align”. She had insignificant medical and dental history with regard orthodontic treatment. Clinical examination revealed that she was in permanent dentition stage with traumatic deep bite, lower lip strap habit and dry lips. The jaw function was within normal limits with no signs of temporomandibular joint dysfunction. Pretreatment extra oral examination showed that her profile was convex profile, competent lips, acute nasolabial angle (NLA), deep labiomental fold (LMF), wide buccal corridor, retrusive lower lip and non-consonant smile arc.
The maxillary and mandibular dental midline was shift to left side by 0.5 mm in relation the soft tissue facial midline. Her malocclusion was characterized by molar 1/2 Class II right side, 3/4 Class II left side and canine Class II relationships bilaterally. Overjet (OJ) 5mm, over bite (OB) 8mm which is represent 100% of lower incisors overlapped by upper incisors, retroclined upper incisors, retruded lower incisors, curve of Spee was exaggerated in the upper arch and deep in the lower arch by 5mm. Mild maxillary and mandibular crowding about 2 mm and 3 mm respectively, multiple rotated teeth and lower molars were tipped lingually. There was no transverse discrepancy (Figure 1&2).
The initial panoramic radiograph showed condyle, rami height, sinuses, bone trabeculation and level were symmetrical within normal limit, all third molars were impacted, no missing teeth and normal roots shape and length except tooth #34 with dilaceration root (Figure 3).
Cephalometric analysis showed that patient had SNA angle of 80°, SNB angle of 76°, ANB angle of 4° and MP angle of 26°. The upper incisors had a 102° angle relative to the palatal plane and the lower incisors had a 90° angle relative to the mandibular plane (Figure 4 & Table 1).
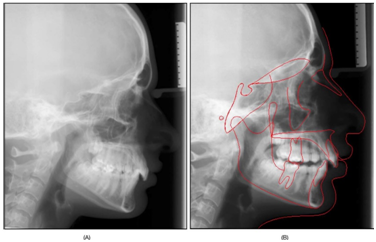
Figure 4 (A) Pretreatment Lateral Cephalometric Radiograph. (B) Pretreatment Traced Lateral Cephalometric Radiograph.
Measurement |
Mean |
Pre-treatment |
SNA |
82±2° |
80.9° |
SNB |
80±2° |
76.1° |
ANB |
2±2° |
4.8° |
NA - APg. |
0±5° |
6.1° |
Wits Appraisal |
1.2±1.9 mm |
3.5 mm |
Mand. plane to FH |
25±5° |
19.3 |
Mand. Plane to SN |
32±5.1° |
26.4 |
Max. Plane to SN |
8±3° |
10.3° |
Max. to Mand. Plane |
25±3° |
21.6° |
Y axis SGn. / SN |
59±4° |
60.2° |
Lower Face Height |
55±3% |
50.3% |
U Inc. to Max. plane |
110±6° |
102.7° |
U Inc. to SN |
104±2° |
96.6° |
U Inc. to NA |
22±5° |
14.8° |
U Inc. to NA (mm) |
4±3 mm |
2.1 mm |
U Inc. to L Inc. |
131±5° |
143.1° |
L Inc. to Mand. |
93±6° |
90.4° |
L Inc. to NB |
25±6° |
22.6° |
L Inc. to NB (mm) |
4±2 mm |
1.3 mm |
L Inc. to APog. (mm) |
1±2 mm |
-2.3 mm |
Upper lip to E-line |
-4±2 mm |
-5.1 mm |
Lower lip to E-line |
-2±2 mm |
-4.7 mm |
Nasio-labial angle |
100±10° |
88.1° |
Table 1 Pre-treatment lateral cephalometric reading
Treatment objectives
Based on the clinical examination and records analysis, the treatment objectives were:
Treatment options
Based on the clinical examination and treatment objectives, the following treatment plans mentioned:
Proposed retention strategy and rationale
Based on the treatment plan that have been chosen by the patient and her parents, the retention protocol was upper modified Hawley retainer with anterior bite plate and lower fixed retainer extend from first premolar to other first premolar in addition to Hawley retainer. Since this case has deep bite, ideal axial inclination of the incisors at the end of treatment could be a factor in deep bite stability. Proper interincisal angle should be achieved to prevent the deep bite relapse.10 Lower fixed retainer will be placed to keep the anterior teeth alignment and to avoid deep bite relapse. Using anterior bite plate with Hawley retainer will prevent relapse of deep bite. Keeping lower incisors in contact with the palatal acrylic of the upper retainer will prevent lower incisors eruption and allow eruption of posterior teeth.11 Long-term use of Hawley retainer firmly holds each tooth in its position and maintain transverse width.
Treatment progress
Treatment started with placement of separators in upper and lower first and second molars and referred the patient to oral surgeon to extract upper and lower third molars. Bonding upper arch 5-5 teeth with preadjusted fixed appliances (0.022 × 0.028-inch, MBT system), band upper first and second molars and leveling and alignment upper arch till reach to 0.019x0.025Niti. Single TAD (OrthoEasy® Pin 0.022“/1,7 x 8mm) Forestadent have been placed in palate area. Alginate impression taken for upper arch to construct modified frog appliance. A frog appliance kit consists of: screw, preformed spring and screw driver (Figure 5).
The manufacturer advice, occluso-apically the frog screw should be placed approximately 10mm to 12mm from the occlusal surface. This produce bodily movement of the molars because the appliance approximately at the center of resistance of the molars. Lingual sheaths soldered to the lingual surface of upper first molar bands and anterior part of frog appliance solder to miniscrew cap. At the time of appliance insertion, the upper first and second molar bands cemented using a multi-cure glass ionomer orthodontic band cement, inserted the ends of the distalizing spring in to the lingual sheaths of the molar bands, adapt anterior part of appliance in TAD then inserted the spring in posterior part of appliance (Figure 6).
After checking stability of appliance, cut the main arch wire (0.019x0.025 SS) between second premolar and first molar bilaterally then start the activation of appliance. According to the manufacturer instruction, one complete rotation around the axis of the activation screw opens the appliance 0.4mm. Three rotations are recommended for four to five-week interval visit and five rotations are recommended for eight-week interval visit. At each appointment, oral hygiene, the stability of the appliance and progress of distalization were evaluated till super class I molar relationship has achieved. After the maxillary first and second molars distalized, expansion done in the upper arch by open the loops in frog appliance spring wire. Later the device was left in place as a retention appliance for three months. Sectional arch wire has been replaced with continues arch wire 0.016x0.022 Niti. One month later, start leveling and alignment of lower arch from right second molar to left second molar till reach (0.019x0.025 SS) in both arches and start space closure. At the end of active treatment, finishing procedures were applied for final alignment of the teeth, detailing of the occlusion, frog appliance and TAD had been removed. After 21 months of treatment, debonding of upper and lower arches, retainers delivered for the patient.
At the end of orthodontic treatment, bilateral Class I molar and canine relationship was achieved with normal OJ. All upper and lower teeth aligned with flat curve of speed along with coinciding upper and lower teeth midline with the facial midline. Acceptable overbite was attained with alleviation of deep traumatic bite (Figure 7).
Final cephalometric analysis and superimposition of pretreatment and posttreatment tracings showed that the skeletal Class I relationship had been achieved with increase of the lower anterior facial height (Figure 8 & Table 2). Overall superimposition showed nose grew downward by 2 mm, an upper lip moved downward by 2 mm and backward 3mm, lower lip moved upward by 2mm and backward 1 mm, point A moved backward by 1 mm, point B moved forward 2 mm and downward 2mm based on Bjork method of stable structure that register on the inner contour of the anterior wall of sella turcic. Maxillary and mandibular regional superimposition showed that upper central incisor proclined by 6° and retruded by 1.5mm and intruded by 1mm and upper first molar moved distally by 4.5mm. However lower incisor proclined by 9° and intruded by 2mm and lower first molar mesialized by 2mm and extruded 2.5mm. Downward backward rotation of mandible based on Bjork method of stable structure that register on anterior wall of key ridge and the inner cortical structure at the inferior border of the symphysis and mandible canal (Figure 9). The final panoramic radiograph showed a good root parallelism except #15, 25 and #34 dilaceration (Figure 10).
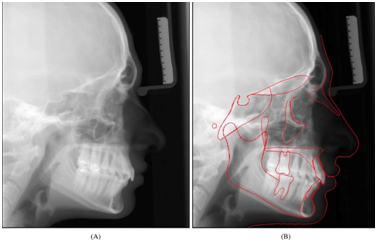
Figure 8 (A) Post-treatment lateral cephalometric radiograph; (B) Post-treatment traced lateral cephalometric radiograph.
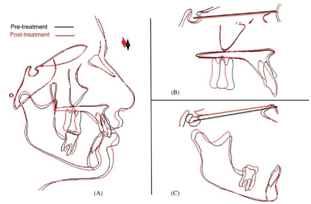
Figure 9 (A) overall superimposition; (B) regional maxillary superimposition; (C) regional mandibular superimposition.
Measurement |
Mean |
Pre-treat |
Post-treatment |
SNA |
82±2° |
80.9° |
80.5° |
SNB |
80±2° |
76.1° |
77.8° |
ANB |
2±2° |
4.8° |
2.7° |
NA - APg. |
0±5° |
6.1° |
3.8° |
Wits Appraisal |
1.2±1.9 mm |
3.5 mm |
1.3 mm |
Mand. plane to FH |
25±5° |
19.3° |
22.9° |
Mand. Plane to SN |
32±5.1° |
26.4° |
30.0° |
Max. Plane to SN |
8±3° |
10.3° |
10.9° |
Max. to Mand. Plane |
25±3° |
21.6° |
25.1° |
Y axis SGn. / SN |
59±4° |
60.2° |
62.9° |
Lower Face Height |
55±3% |
50.3% |
53.1% |
U Inc. to Max. plane |
110±6° |
102.7° |
108.2° |
U Inc. to SN. |
104±2° |
96.6° |
102.1° |
U Inc. to NA |
22±5° |
14.8° |
20.3° |
U Inc. to NA (mm) |
4±3 mm |
2.1 |
2.9mm |
U Inc. to L Inc. |
131±5° |
143.1° |
131.9° |
L Inc. to Mand. |
93±6° |
90.4° |
99.9° |
L Inc. to NB |
25±6° |
22.6° |
32.1° |
L Inc. to NB (mm) |
4±2 mm |
1.3 mm |
4.3 mm |
L Inc. to APog. (mm) |
1±2 mm |
-2.3 mm |
3.5 mm |
Upper lip to E-line |
-4±2 mm |
-5.1 mm |
-3.5 mm |
Lower lip to E-line |
-2±2 mm |
-4.7 mm |
-1.8 mm |
Nasio-labial angle |
100±10° |
88.1° |
90.6° |
Table 2 Post-treatment lateral cephalometric reading
The patient presented with skeletal Class II due to retrognathic mandible and Class II div 2 malocclusion with decrease lower anterior facial height, reduce mandibular plane angle and traumatic deep bite (short face features). Non extraction treatment favored as this approach takes an advantage of increasing vertical facial height to enhance overbite correction. Extraction in low angle cases complicate the mechanics of overbite correction because strong muscles force impedes the ability of the posterior teeth to move forward.12,13 Orthodontists for the most part concur that space closing mechanics tend to deepen the bite and making it more difficult to correct and/or maintain the proper overbite relationship in patients with deep bite.14
Molar distalization is recommended for the correction of Class II malocclusions in deep bite patients and in the presence of a convex or normal facial profile.15 So, non-extraction with maxillary molars distalization option was offered to the patient as the best option and the patient agreed with it.
The advantages of Frog appliance : Palatal appliance, Skeletal anchorage, Hygienic, 3D movement, the ability to measure the amount of distalization, easy in activation and adjustable arms (not solder to bands).
To eliminate the need for dental anchorage and its undesirable side effects on the anterior arch, we have added TAD within Frog molar distalization appliance to eliminate the need of dental support or acrylic palatal button. The anterior area of the palate is considered to be a safe region for miniscrew insertion because it is far from the teeth roots and other important anatomic structure.16
Miniscrew supported Frog appliance is a fixed appliance, reduce the need of patient compliance. Moreover, the use of this appliance results in successful, distalization of maxillary molars. The outcomes from this case report reflected that the Frog appliance is an effective and a reliable method for the distalization of maxillary molars. The use of miniscrews with this appliance eliminate the effect of distalizer on the other teeth.
None.
The authors would like to thank Dr.Abdulaziz K. AlKhunain, consultant in orthodontics, teaching faculty member at prince Abdurrahman advance dental institute Riyadh, Saudi Arabia for all of his careful, constructive and insightful comments in relation to this work.
The authors declare there are no conflicts of interest.

©2019 Aldayel, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.