Journal of
eISSN: 2373-4345


Review Article Volume 13 Issue 1
1Professor and Head of Dental Biomaterials, Faculty of Dentistry, Modern University for Technology & Information, Egypt
2Professor of Oral Medicine and Periodontolgy, and Dean of Faculty of Dentistry, Modern University for Technology & Information, Egypt
Correspondence: Nagy Abdulsamee, Professor and Head of Dental Biomaterials, Faculty of Dentistry, Modern University for Technology & Information, Egypt
Received: August 31, 2021 | Published: February 28, 2022
Citation: Abdulsamee N, Elrefaey M. Laser: silent revolution in prosthetic dentistry bridging the gap to future. historical review. J Dent Health Oral Disord Ther. 2022;13(1):9-19. DOI: 10.15406/jdhodt.2022.13.00563
Several technologies have been used to overcome current challenges in dentistry throughout the last few decades. Laser technology is the most recent addition to this group of technologies. Because of its great precision, biocompatibility, and few side effects, it has had a significant impact and has so supplanted several traditional procedures. For the past two decades, lasers have been well-integrated in clinical dentistry, enabling practical choices in the management of both soft and hard tissues, with a growing usage in the field of prosthetic dentistry. One of their key advantages is that they can deliver extremely low to extremely high concentrated power at a precise location on any substrate using any method available. New approaches are provided for the development of prosthodontic treatments that demand high energy levels and careful processing, such as metals, ceramics, and resins, as well as time-consuming laboratory processes like cutting restorative materials, welding, and sintering.
Lasers have a wide range of applications, and their use in the field of prosthodontics has seen them replace stainless steel scalpels with optical scalpels to a respectable extent throughout the surgical field and other traditional ways. A new technology on the horizon will address these flaws, but it will also come with its own set of hazards and restrictions. The purpose of this article is to discuss the application and uses of lasers in prosthodontics, as well as how lasers have revolutionized patient care. A future project could be the development of new intraoral laser devices.
2. Keywords: Laser physiscs, prosthetic Computer-Aided Design, laser sintering, implantology, maxillofacial prosthodontics
In 1917, scientist Albert Einstein established the theory of stimulated emission, which serves as the scientific foundation for the production of laser light.1 His theory lay dormant until 1956, when Thomas Maiman created the first laser, the Ruby laser. Mailman exposed an extracted tooth to a prototype Ruby (694 nm) Laser, which resulted in energy transfer. Rubby laser was first employed in 1967 for carry removal and cavity preparation, although it resulted in pulpal damage.2 The CO2 laser was invented by Patel at Bell Laboratories in 1964,1 but it was not used in oral surgery until the 1980s for the excision of soft tissue diseases.3
The Nd:YAG laser was the first laser designed exclusively for dental usage in caries eradication and Kinetic cavity preparation, and it was created in 1987 and approved by the US Food and Drug Administration in 1990.3 One year after the Nd:YAG laser, the argon laser was produced. Lasers became widely used in dentistry after the advent of the diode laser. The American Dental Laser, which paved the way for laser dentistry, did not become commercially available until 1989.
Drs Terry and Bill Meyers invented the first dental laser in 1989, a 3W Nd:YAG for soft tissue application, and since then, a range of laser wavelengths have been introduced and sold.4 In the mid-1990s, laser dentistry made a breakthrough. In the mid-1990s, dentists were able to choose from a variety of laser types (diode laser, Nd:YAG, Er,Cr:YSGG, Er:YAG, CO2) with appropriate wavelengths (810 - 890 nm, 1064 nm, 2780 nm, 2940 nm, 10600 nm respectively).
Light is an integral part of our life. LASERS, one of the greatest inventions in science and technology, was developed in the early twentieth century. Light amplification by stimulated emission of radiation (LASER) was invented by Gordon Gould, a Columbia University doctoral student, in a 1959 study that went on to become a gift to the health sciences.5 In the medical field, the use of lasers for treatment has become widespread.6 Lasers are a very appealing technology in numerous sectors of dentistry because of their low intrusive nature and speedy tissue reaction and healing. They serve as a tool to achieve a better result than ever before. The rapid development of lasers and their wavelengths for a variety of soft and hard tissue applications may continue to have a significant impact on prosthetic dentistry's scope and practice. The goal of this paper is to familiarize every clinician, particularly prosthodontists, with laser fundamentals and different laser systems so that they can incorporate them into their clinical practices.7
The three separate phenomena that occur during the production of an atomic spectral line outlined by Albert Einstein in 1916 (Figure 1 and 2)8 are spontaneous emission, stimulated emission, and absorption. Amplification of stimulated emission generates laser light.9,10 Amplification is a step in the laser's internal process. Understanding how light is produced can be aided by identifying the components of a laser instrument.9-11 A typical laser is made up of six fundamental components (Figure 2):
The common characteristics properties of all laser beam types (Figure 3As-C) in comparison to those of normal light (Figure 3A-C) are:-
A) Directionality is a situation in which all waves are parallel to one another and have little divergence or convergence. It allows laser light to travel long distance without loss of intensity (Figure 3A). Those of normal light are scattered (Figure 3A).
B) Monochromaticity refers to the fact that it is made up of only one wave length. This monochromatic feature of laser light has therapeutic significance since it allows it to target certain chromophores like water, hemoglobin, and melanin, allowing for specialized clinical uses (Figure 3B). Those of normal light are polychromatic (Figure 3B).
C) Coherence All photon waves have the same amplitude and frequency, which is known as coherence. As a result, a special type of focused electromagnetic radiation is produced (Figure 3A).12 Those of normal light are non-coherent (Figure 3C).
D) Because of laser collimation, monochromaticity, and coherence its Brightness are more intense and brighter compared to the sun. A 1 mW He–Ne laser, which is a highly directional low divergence laser source, is brighter than the sun, which is emitting radiation isotropically. Brightness is defined as power emitted per unit area per unit solid angle.13
In medical practice, wavelengths ranging from 193 nm to 1060 nm are commonly employed, with wavelengths ranging from ultraviolet to far infrared (Figure 4). Invisible ionizing lasers, on the other hand, are not used in dentistry.
It is usual to classify laser devices according to their active material into:-
N.B. Fiber lasers: They operate in a similar way to solid-state lasers in terms of principle. The doped area is found in the fiber's core. This type of laser has a higher thermal dispersion and the unique ability to operate in transversal single mode16 due to the fiber shape. This provides for many kilowatts of emission while retaining a greater beam quality.17 Micromachines, vol. 9, no. 209, p. 23. Yb-doped and Yb/Eb-doped fiber lasers are commonly utilized in industrial applications where high precision machining is required. Tm-doped fiber lasers allow for improved contact with soft tissues in medical applications without causing a temperature rise at the operation site. It has the potential to be used for intraoral welding of metallic appliances.18
Certain lasers' output is dangerous to the human body, and its exposure can harm the eye and skin. Limited access to the room and equipments, the use of personal protective equipment, system monitoring, testing and operations of the laser and its delivery systems, correct applications, and vigilance on the part of each laser team member are all necessary for hazard control.19 The International Electrotechnical Commission (IEC), a global agency, has developed a new categorization system to identify the amount of laser beam hazard given in Table 1.20
|
|
Table 1 Standard IEC Classifications20
Any practice that uses lasers must have proper safety protocols in place. The practice should select a laser safety officer whose role it is to implement and maintain safety standards. Each device's maker is required to train providers on the critical precautions that are required for each device. The following are some of the most common safety precautions:-
Laser classification according to emission mode21
Any laser emission mode works on the idea that light energy contacts tissue for a specific amount of time, causing a thermal reaction. The dental laser device is capable of emitting light energy in three different modes:-
Clinical significance of pulse type
We need a pulsed mode to cut very thin or fragile soft tissue because the amount and rate of tissue removal will be slower, but we need a continuous wave to cut thick dense fibrous tissue because more energy for removal and emission will provide a faster yet safe pace of excision.
Laser tissue interaction
One of four ways light energy interacts with a target medium (e.g. oral tissues) (Figure 7)22:-
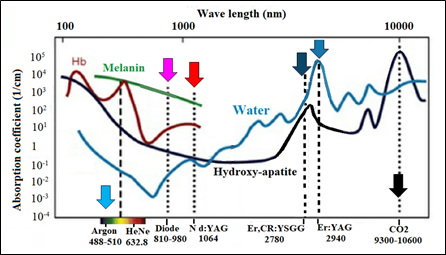
Figure 8 Different laser wavelengths in the electromagnetic spectrum and the relative absorption in dental chromophores. All the wavelengths of the dental lasers are in the visible and the non-ionizing infrared part of the spectrum.22
Absorption needs chromophores, which are light absorbers with a specific affinity for specific wavelengths of light. The following are dental chromophores (Figure 8)22:
I- Soft Tissue chromophores: Melanin, Hemoglobin & Water,
II- Dental hard tissue chromophores: Water & Hydroxyapatite),
III- Photosensitive materials in VLC materials (Camphorquinone).
Laser energy and tissue temperature
The initial phase hyperthermia occurs when tissue is exposed to temperatures above normal, but the tissue is not damaged. A temperature of 60°C causes denaturation and coagulation of the protein. Using the laser parameters within the temperature range, the clinical practitioner can eliminate the granulomatous lesion without vaporizing the surrounding tissue. At 70°C to 80°C, the tissue layers adhere to each other. The water within the tissue vaporizes as the temperature reaches 100°C. At this temperature, the ablation begins, but the dental tooth structures are not ablated. Dehydration is complete at around 200°C, and the tissue carbonizes (Figure 10). Continuous laser treatment causes tissue carbonization, which hinders normal tissue ablation, resulting in tissue necrosis.23,10
Uses of laser in prosthodontics
Smile design involves the use of lasers such as argon, CO2, diode, erbium, and pulsed Nd:YAG. Soft tissues are pencil-marked to determine correct gingival shape, symmetry, axial inclination, and zenith before employing the laser. To measure the marginal gingiva, a periodontal probe is positioned apically to the alveolar crest. The biological width is determined and tagged with a laser as a reference place, allowing the physician to concentrate on aesthetics and functioning as a visual completion point.38
The vitality and order of the neighboring tissues in relation are always important factors in the success of the prosthesis placement. A good pre-prosthetic surgery can increase the success rate and improve the patients' satisfaction. Lasers are used to treat irregularly resorbed ridges, deformities, and hyperplastic tissue, resulting in changes to both hard and soft tissues for improved function.
3D Printing: 3D printing for both bony and soft tissue reconstruction, has become the essential clinical tool which derives a model from a computer-aided design (CAD) built in a layer by layer fashion. Various 3D printing techniques have been explored in the clinical setting such as stereo-lithography, multi jet modelling, SLS, binder jetting and fused deposition modelling.49,50
In clinical dentistry, cutting the metal framework after casting is common due to a poor fit in implant or dental abutments. The most common reason is wax pattern distortion, as well as deformation or strains during casting 53. Welding the split pieces of the metal framework has been employed to overcome laboratory distortion problems that result in metal framework mismatch in the marginal area. Welding the metal pieces decreases framework deformation and enhances fit to the abutments as well as stress distribution uniformity.53
Connecting the metal framework's sections has been done in a variety of ways. Laser-assisted welding is the favored method among them because it allows the alloy to melt and integrate into the original framework by forming a new joint.53,54 When a light beam strikes the metal's surface, the metal absorbs it and converts it to heat, which then penetrates the metal due to conductivity. Because of the high heat concentration, the metal melts and forms a hollow cavity that will be filled with molten metal.55
This technological achievement has been made even more efficient by the industrial enhancement of compact powerful units of pulsed Nd:YAG lasers. Due to the concentration of energy in a relatively tiny portion of the framework, laser-assisted welding is precise and well defined. In addition, the operator has complete control over each stage of the welding process at all times. Any distortion that occurs during the welding process can be identified and repaired instantly by placing fresh spot welds on the opposite side of the original distortion point.56 Laser welding appears to give precision, reduced distortion, and a small heat affected zone in the dental lab.57
In a case study involving intraoral welding with a Nd-YAG laser, a metallic (Co-Cr-Mo) bar for a maxillary overdenture was welded intraorally in 47 seconds with no pain or discomfort reported by the patient.58 The Nd-YAG laser is a good choice for welding orthodontic wires in orthodontics.59
Intraoral Laser Welding (ILW) in implant prosthetic dentistry58
A 67-year-old man visited our office for a physical examination. The patient seemed edentulous on the upper arch, where he had a total removable prosthesis, during the clinical examination. His issue was that the denture was not stable, and he found it difficult to speak and eat. The choice was made to put four implants in Figure 15 a. Four abutments were screwed to the implants after the surgical operation (Figure 15 a) (Figure 15 b).
Then, a bar previously constructed by the dental technician previewing the position of the implants by the maxillary arch impression was fitted in the four abutments (Figure 15 c). The bar was welded intraorally (Figure 15 d) using a dental Nd:YAG laser to secure the position. The entire intraoral welding treatment lasted 47 seconds, and the patient reported no pain or discomfort during it (Figure 15 e).
The bar was withdrawn from the mouth with the abutments (Figure 15 f), the welding technique was completed extraorally with the same device (Figure 15 g), the abutments were cut and polished, and it was then reintroduced into the mouth (Figure 15 h and i). Four silicon OT Cap (Rhein 83, Italy) were then used to secure the prosthesis to the bar (Figure 15 j). After two days, seven days, and fifteen days, the patient was evaluated again, then monthly for six months, and no concerns were found.
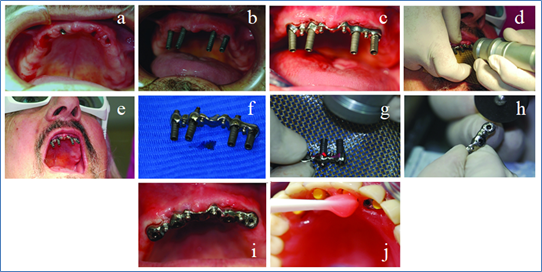
Figure 15 a) Patient just after four implants insertion, b) Abutment screwed to the implants, c) Bar inserted in the abutments, d) Intra oral laser welding, e) The bar welded to abutments, f) Bar and abutments removed from the mouth, g) The welding procedure completed extra orally by the same device, h) The abutment cut by disc, i) The bar reapplied into the mouth, and j) The OT Caps fixed with acrylic resin to the prosthesis58
Metal frames for metal-ceramic restorations are made using laser sintering. Its goal is to eliminate the negative effects of casting while also lowering the financial cost and labour time. The porosity of the material, the fit in the marginal area, and the mechanical qualities of the material in general are critical to the reconstruction's effectiveness. Selective laser sintering is a layered manufacturing technique that allows complicated three-dimensional items to be created by hardening consecutive layers of material powder on top of one another. It is accomplished by employing the heat energy generated by a concentrated laser beam to treat the targeted locations. Each layer is scanned depending on the individual cross section, as determined by the CAD model, using a beam deflection system (galvanic mirrors). A powder deposition technique is used to deposit consecutive layers of material (ranging in thickness from 20 to 150 m).61,62
For the fabrication of CoCr crowns and bridges, laser sintering has now become the industry standard.63 It is now possible to create fully stress-free and properly fitted non-precious metal frames even for bigger bridge spans by optimizing post-processing after the actual building process. Because of the high number of units that can be placed on a single platform, the manufacturing time per unit has been lowered to just a few minutes (Figure 16). When it comes to fixed restorations composed of non-precious alloys, the process is incredibly cost-effective and well-established.
One-piece prostheses can now be planned digitally and manufactured subtractively using CNC milling units or additively using 3D printing thanks to the introduction of digital techniques for denture production, such as computer-aided design/computer-aided manufacturing (CAD/CAM) and additive manufacturing techniques.64
The difference between indirect and direct fabrication processes may be seen here. The frameworks are printed in wax or polymers and then cast using the lost-wax technique in the indirect approach. The CAD data set is immediately turned into a Co-Cr alloy object by laser sintering in the direct approach (Figure 17).65 This approach is still in its early stages of development. In recent articles, laser sintering has been reported to provide advantages in digital manufacturing in terms of standardization, shorter production times, and easy digital data transfer.66 Its economic viability, however, is currently being evaluated.67 Before this procedure can be confidently suggested, more research is required. The retaining elements (clasps) require special attention since they are constantly exposed to significant mechanical loads while performing their retaining and supporting functions.
The advantages of laser sintering include the rapid building of complicated metal frameworks and the use of an automated system, as well as the reduction in working time due to the elimination of numerous phases such as wax model making, coating, dewaxing, and casting. Because the required amount of the alloy is accurately selected and regulated, it saves on the use of the alloy by decreasing metal waste. The success of a dental restoration depends on how well the restoration fits in the marginal area. An in vitro study compared marginal fit and axial wall adaptability of cobalt-chromium copings fabricated using either a conventional lost-wax or a metal laser sintering technique, finding that the laser sintering technique had significantly higher marginal fit and axial wall adaptability than the lost-wax technique, though marginal fit values for both techniques were within clinically acceptable limits.62 Laser sintering is a technology that requires expensive equipment, which is one of its drawbacks.
Due to expensive installation costs and inadequate control over the thermal effect of lasers on soft/hard tissues, laser use was primarily limited to professionals and researchers. Dentists are more motivated to use lasers in their clinical practice as a result of recent advancements in laser technology and lower costs. Dentists may perform laser applications on their patients with much more safety than before, owing to smaller laser pulses and lower energy. Lasers are a very appealing tool for the dental industry because of their minimally invasive nature and increased tissue response with better recovery. The difficulty of setting the parameters in relation to the material utilized, its thickness, the gap dimension, and the filler alloy are the most challenging and problematic aspects of using laser technology for dental welding. Laser-assisted welding has almost completely replaced traditional soldering processes among dental workers. In the near future, laser sintering-based metal framework construction may be able to replace waxing and casting. Furthermore, Nd:YAG laser welding equipment have traditionally been big and expensive to install and maintain. As a result, the development of simple, inexpensive machines that are simple to operate and require little training would be a fantastic opportunity for dentists to weld metals directly in their offices.68
The wavelength, power, intensity, fluence, and pulse duration of the many laser systems available for intraoral and laboratory application vary. Although a variety of devices are available for dental applications, some industrial lasers appear to be more effective in the processing of very hard materials, such as zirconia. The ability of ultrafast lasers to ablate and cut the yttria stabilised zirconia (YTZP) surface with excellent precision, creating a wide variety of spots or lines, justifies additional exploration. Such laser equipment are expensive, which is a major drawback that limits their use in dental laboratories. Furthermore, the cost-effective manufacture of intraoral ultrafast laser hand pieces (of minimal size) appears to be a future goal.69
Not applicable.
None.

©2022 Abdulsamee, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.