Journal of
eISSN: 2373-4345


Case Report Volume 2 Issue 5
Misr University for Science & Technology, Egypt
Correspondence: Nagy Abdul-Samee Abdul-Hameed, Vice Dean for Graduate Studies & Researches, College of Oral and Dental Medicine, Misr University for Science & Technology, Al- Motamayez District, 77, Giza, Egypt
Received: June 20, 2015 | Published: July 25, 2015
Citation: Hameed NASA. Inserting retention plastic caps to ball implant supported overdenture: easy chair side technique. J Dent Health Oral Disord Ther. 2015;2(5):165-169. DOI: 10.15406/jdhodt.2015.02.00064
Traditionally, retention plastic caps are fitted to ball implant supported overdenture by the indirect method following the traditional prosthetic steps for implant over dentures. Drawbacks of this technique are more evident, such as improper load distribution between implant and mucoperiosteal denture foundation, pivoting effect at implant site resulting in frequent fracture of over denture at this site, loosening of the implant and time consuming and expensive as it needs extra laboratory steps and equipments. The aim of the present work was to present a simplified direct technique, which did not need any special equipments and hopping that it would avoid the disadvantages of the indirect one.
Keywords: overdenture, implants, occlusal forces, osseo integration, stabilization, residual ridges
Restoration of totally edentulous patients with removable prosthesis designs that incorporate osseo integrated implants provides the patient with alternatives to mucosa-supported complete denture.1 A highly predictable and effective approach is the implant-supported over denture, which offers improved retention, stability, function, proprioception, and comfort.2,3 Compared with complete denture, implant-supported overdenture improves the stability of the prosthesis. Increased number of implants may guarantee more retention. However, there is a problem of increased cost and anatomical limitations in severely restored residual ridges, especially in the mandible. Several studies demonstrated that the two-implants-supported overdenture therapy can be considered as a very reliable treatment for patients with an edentulous mandible.4–6 Therefore, two-implants-supported overdenture in the mandible should be the standard treatment modality for full edentulous patients suffering from discomfort with their conventional denture.4–6
Various attachments have been advocated for retaining overdentures to implants. Attachments are mechanical interlocking devices of different designs including splinting bars, ball and socket attachments and combinations of bars and attachments.7,8 All the retention approaches distribute occlusal forces through the over denture to the implants and the posterior edentulous ridges.9 The degree of load sharing that occurs depends on the specific system used.9,10 An ideal situation would exist if the load were shared so that no area would be overloaded. Because this ideal condition is probably unattainable, designs that tend to provide the most appropriate load transfer would be preferred.11 Compared with individual attachment, bar connectors provide a rigid support for over denture similar to that provided by fixed prostheses, guarantee a primary stabilization by splinting the implants,12 provide better retention,13 and reduce load transmitted to implant.14
Individual attachments are indicated mainly when the span between implants is too long and when insufficient interarch space exists to accommodate attachments on a bar.14 Despite their advantages, it has been proved that incorporating attachments in prosthesis induces more stresses to the supporting structures.14 However, the resilient ball and socket type appears to transfer the stresses in a favorable manner to the retaining structures.14 The resilient attachments are designed to provide some vertical movement and rotation of the denture base. This is intended to allow the sharing of occlusal forces between the abutment and the soft tissues.14 From a clinical point of view, it is claimed that a resilient retention mechanism for over denture fixation should be used to allow equal tissue and implant support. It protects against implant overloading (stress-breaking action) because most of the masticators stresses are transmitted to the posterior edentulous ridge .12–18 Bone loss in the edentulous regions of mandible is not significantly reduced because of the resilient nature of the ball attachment permitting free rotation in six directions.10,14 Traditionally, retention plastic caps are fitted to ball implant supported over dentures by the indirect method. Drawbacks of this technique are more evident, such as improper load distribution between implant and mucoperiosteal denture foundation, pivoting effect at implant site resulting in frequent fracture of the overdenture in this site, loosening of the implant, and time consuming as it needs extra laboratory steps. Also during curing, the caps may be distorted as the curing temperature can approach the glass transition temperature of the polymer from which the caps are fabricated. This drew my attention to introduce a direct technique, which proved to be simpler, did not need special equipments, and hopping that it will eliminate the drawbacks of the indirect technique.
Abutment preparation
Over denture construction
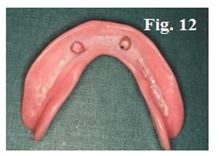
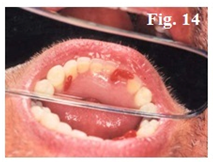
After abutment preparation (Figure 6) the conventional clinical and laboratory procedures for denture construction (Figure 7–14) are followed except that metal framework should not cover the abutment areas.
Attachment incorporation
This patient was referred to the dental center King Fahd Hospital, Al-Madinah Al-Menwara. K.S.A., to receive an overdenture, this was because the implanting dentist was working in a private clinic. He left suddenly to his country without completing the prosthetic part. The center was not equipped with facilities for such restorations at that time. The patient was asked to purchase the retention plastic caps, and by trial and error it was possible to complete the case with the current technique by the simple and available equipments. One of difficulties met was the absence of impression posts, implant body analogs, and the attachment-seating tool of the male portion. The current technique has solved these problems and an implant-supported overdenture was delivered to the patient.
The present technique has the following advantages over the indirect one
Fabrication of implant supported overdenture with retention plastic caps inserted using chair side technique is an advantageous treatment option because of saving cost and time, which benefits both the patient and the clinician.
None.
The author declares that there are no conflicts of interest.
None.

©2015 Hameed. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.