Journal of
eISSN: 2373-4345


Research Article Volume 14 Issue 2
1Rómulo Gallegos National Experimental University, Venezuela
2Dentist, Jose Antonio Paez University, Venezuela
Correspondence: Zulay Palima, Rómulo Gallegos National Experimental University. San Juan de los Morros, Venezuela
Received: March 06, 2023 | Published: May 24, 2023
Citation: Palima Z, Gasperin J, Garcia D, et al. Influential factors of the success and/or failure of dental implants. J Dent Health Oral Disord Ther. 2023;14(2):34-40. DOI: 10.15406/jdhodt.2023.14.00592
Introduction: Dental prostheses are the most widely used artificial means to replace missing teeth in people, in order to restore the necessary harmony in the stomatognathic complex, both functional and aesthetic. Dental implants are pure titanium fixations that are placed in the maxillary or mandibular bone in order to replace the roots of missing teeth, currently they are one of the most innovative rehabilitative therapies in dentistry.
Objective: Evaluate the factors that influence the success and/or failure of dental implants.
Methodology: This research is framed within a systematic bibliographic review.
Results: The factors that have the greatest influence and affect the immediate result are heavy smoking, implant placement under a torque of less than 15 Nm, overheating of the site, lack of primary stability at the time of implant placement, premature loading or microbiological contamination that alter the normal healing process of the soft tissues and prevent the intimate union between the bone and the implant from forming.
Conclusion: Success and failure are dynamic conditions linked to time and require periodic evaluation. The main criteria to evaluate the quality of health of the dental implant are mobility and pain, the presence of any of them compromises the implant to a great extent. Non-osseointegration and peri-implantitis were the most frequent causes of failure in the initial phase of the treatment. Regarding the anatomical regions of the oral cavity, the failure rates were low and the survival and success rates were high.
Keywords: dental implants, smoking, biological contamination, cicatrization, failure
Teeth are essential to develop a normal life. Its main function is to grind food to promote proper digestion, in addition to its importance in phonation and the harmonious expression of the face. Therefore, they play an important role in the development and social performance of a person; good teeth demonstrate signs of health and welfare.1
Oral health is not only related to the presence of teeth, but also to the state of the soft tissues in the oral cavity, which should not disturb the capacity and general health of the individual.1
One of the problems that affects oral health is edentulism (partial or total dental absence), which is not necessarily attributable to old age, since there are multiple causes of tooth loss, such as: caries, periodontal disease, malocclusions, loss of bone mass, decreased bone and increased porosity, among other causes, such as systemic diseases, accidents, bone complaints, dentoalveolar traumas and the extraction of dental pieces. The permanence or loss of these structures can affect people emotionally and socially.1
When premature dental loss occurs, the dentist is forced to think about the best alternatives and rehabilitation-type treatments, dental prostheses are the most widely used artificial means to replace missing teeth in people, in order to restore the necessary harmony in the stomatognathic complex, both functional and aesthetic.2
Accidentally, from experimental and clinical studies carried out in the 1960s by the Swedish biologist Invar Branemark; the discovery of the use of titanium and the appearance of implants as a very effective mechanism to replace missing and lost teeth, a new specialty arose in modern dentistry: implantology, through which planning, treatment and prosthetic rehabilitation are guaranteed through a multidisciplinary team, in charge of ensuring the therapeutic success and satisfaction of the implanted patient.2
Dental implants represent pure titanium fixtures that are placed in the maxillary or mandibular bone in order to replace the roots of missing teeth. This consists of the direct union of an inert material to the bone tissue and is achieved through a careful surgical installation, as well as a prolonged healing period and an adequate distribution of forces when the implant comes into operation.3
This rehabilitative alternative allows the natural tooth to be replaced by an artificial one with better functionality. Despite being a scheduled surgery, it is not exempt from failures and complications occur in any of the phases of implant treatment.3
This paper aims to identify the criteria for success and failure of osseointegrated implants through a systematic and bibliographic review.
Implants are pure titanium fixations that are placed in the maxillary or mandibular bone in order to replace the roots of missing teeth, which allows the natural tooth to be replaced by an artificial one with better functionality, but despite being a scheduled surgery it is not exempt from failures and the complications occur in any of the phases of implant treatment.3
At the present time, implant techniques offer numerous possibilities of treatment, whose good results can be predicted with great certainty based on their functionality, comfort, beauty, quality and duration; however, the failure of the procedure can occur during the surgical phase or once the prosthetic rehabilitation has been carried out, due to systemic and psychosocial factors of the patient such as iatrogenic factors, deforming habits or dental implant design, among others. However, currently some believe that implant failure after the osseointegration process is mainly due to bacterial infection and not to "rejection" when implants of proven quality are placed, although it is also attributed to specific characteristics of the patients and to the skill of surgeons. Dental implant failures constitute an outstanding health problem in many parts of the world due to their frequency and the aesthetic, facial and psychological alterations they cause in those who do not function favorably.2
The surgical success of the implants is directly related to a process of interaction with the bone (osseointegration), but, when the procedure has failed, an alteration occurs during the initial phase and a formation of fibrous scar tissue occurs between the surfaces of the implants and the surrounding bone. It is known that there are many factors that can contribute to the success or failure of implants, from the condition of the patient to the surgical and prosthetic protocols performed by the operator. Among the different classifications that exist in the literature for implant failure, the most didactic is divided into exogenous and endogenous factors.3
Among the exogenous factors are those related to the experience and skill of the operator and to the characteristics of the implants. Among the local endogenous factors, the characteristics of the bone are of great importance (since poor-quality bone will have a higher probability of rejecting an implant), as well as whether the site has received radiation treatment in the head and neck area, since it modifies the vascularity of the bone, making it unsuitable for any intervention. The amount of bone in the place where the implant will be placed should also be considered, as a lack of bone will lead to placing an implant in the wrong position, compromising the final restoration and subjecting the implant to inadequate forces, or this will lead to choosing a smaller size implant, which may affect its stability and survival.3
The placement of an implant foresees the activation of a biological response that leads to the repair of damaged tissues and the integration of the implant. Then, the same sequence of biological events that occurs in traumatic injuries to bone tissue occurs, whatever their origin, that is, bone formation involves a cascade of cellular events.4
Osseointegration of an implant in the bone is defined as the close apposition of newly formed bone in congruence with the implant, including surface irregularities; even, microscopically, interposed connective or fibrous tissue is not observed and, furthermore, the direct structural and functional connection is established, with the capacity to support normal physiological loads, without excessive deformation and without initiating rejection mechanisms. Light microscopy and transmission electron microscopy analyzes have shown an excellent fit between the implant and the bone.4
The proportion of direct bone-material contact of the implant varies according to implant material and design, host condition, surgical technique, loading conditions and time. A good description for this interface would be to describe it as a discontinuous interface, a term that reflects the trend towards understanding osseointegration as a process and not as a result.4
Proper implant prosthetic treatment planning is essential for long-term success. Obtaining information from a careful medical history is crucial as the first step in treatment planning. For Bascones, the information obtained through the interview and the clinical history, together with the evaluation of the risk factors, are key to assessing the probability that the implant has to osseointegrate.4
Generally, the ideal conditions that allow the achievement of an implant-supported rehabilitation are those that promote the function, phonetics and aesthetics of the patient.4
Various authors have proposed criteria to determine the success of osseointegrated implants: Schnittman and Schulman, Cranin et al, McKinney et al, Albrektsson et al., and Smith and Zarb. The criteria proposed by Albrektsson are widely used nowadays. According to this author, the success criteria of an implant are the following:4
By applying these criteria, a success rate of 85% at 5 years of observation and 80% at 10 years of observation is expected to classify the implant within the minimum levels of success.4 However, these criteria describe an ideal quality implant for a clinical study or report but do not address individual implants that may have a stable condition in the mouth after a brief period of bone loss.4
It should be taken into account that the criteria that are commonly cited in clinical reports refer to the survival percentage, this means if the implant is physically in the mouth or if it has been removed. Critics argue that implants that must be removed for either pain or disease may also be retained and misclassified as successful.4
There are other terms that have been suggested for implant success over time, such as early successful implant for an implant that has 1 to 3 years of service, intermediate successful implant for 3 to 7 years, and successful implant at a long-term for the implant that is older than 7 years.4
Systemic diseases can affect oral tissues by interfering with healing or increasing the risk of other diseases. In addition, these diseases must be treated with medication or other therapies that could affect the tissues near the implants and the osseointegration process. In the reviewed literature, systemic conditions are established that may not make the use of dental implants recommendable or, at least, question the success of this treatment. However, with the available evidence, it is not sufficient to contraindicate implant placement in these patients. According to the American Association of Anesthesiology (ASA), patients who are going to receive dental implants must be in one of the first two physical status categories corresponding to ASA I: healthy patient, or ASA II: patient with mild systemic disease. Patients with compromised conditions or any patient who is in another of the categories should arrive at ASA II to be treated.5
The risk of infection in immunosuppressed patients is one of the main considerations when placing implants in these patients. Antiretroviral therapy postpones the appearance of AIDS in patients infected with the HIV virus and also reduces the manifestations and appearance of opportunistic infections.5
Many case reports have demonstrated successful implant rehabilitations in immunocompromised but stable patients. The recommendation is to extend the follow-up time of these patients after the integration of the implants. Strietzel in 2006 exposes a series of cases with one hundred percent survival of implants placed in patients with HIV, it is not specified whether antibiotic therapy is used, but the use of 0.2% chlorhexidine daily.5
Baron et al., published the rehabilitation of a patient with 12 implants and the follow-up with clindamycin antibiotic medication.5
According to the above, this condition is not contraindicated for the placement of implants as long as they are medicated and stable patients. In addition, as mentioned, the recommendation is to extend monitoring times after implant placement.5
Among the systemic factors that put the implant at risk are smoking, which compromises healing, some medications such as bisphosphonates that inhibit bone regeneration and give rise to osteonecrosis and are indicated mainly in patients with osteoporosis, the older age of the patients and the presence of systemic diseases such as diabetes, or heart and immune diseases, among others. Smoking is a risk factor for general health and oral health, causing diseases such as oral cancer and periodontal disease.6
In this study, heavy smoking (>10 cigarettes per day) was found to be a contributing factor to early failure. Several studies have reported similar results. DeLuca et al., found a failure rate of 23.08% in patients who smoked during treatment, and observed that the greater number of cigarettes increased the failure rate (Figure 1 & 2).6

Figure 1 Results of all the procedures and characteristics of the implants.6
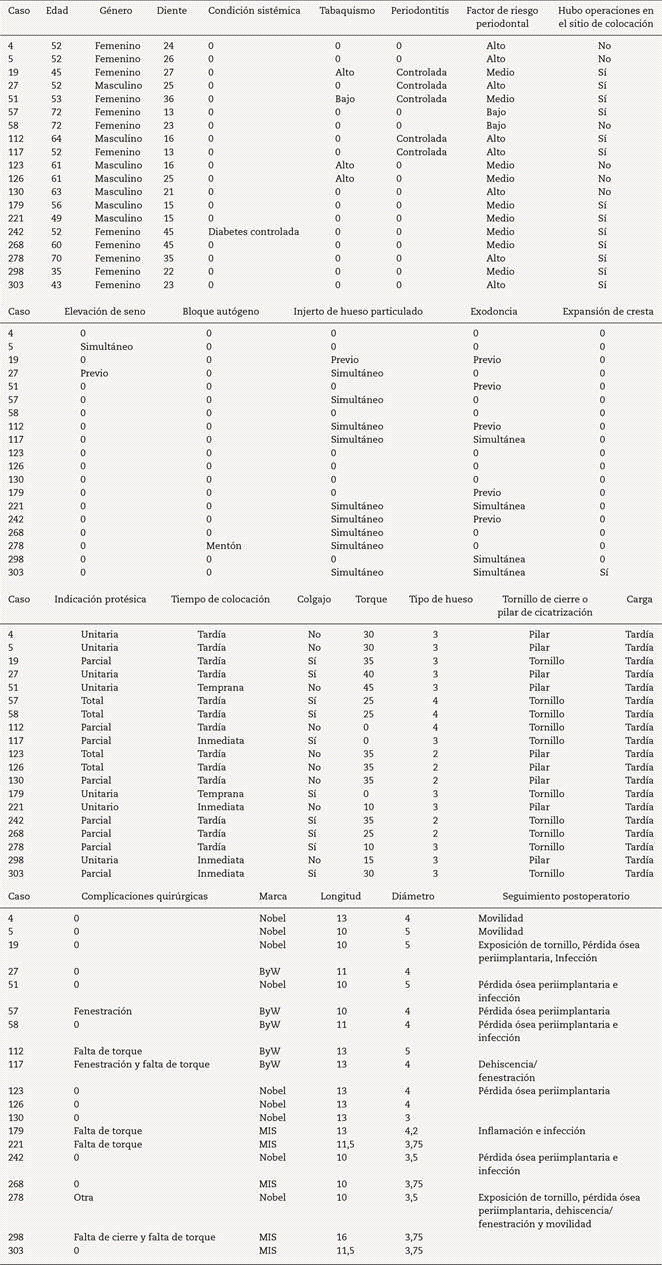
Figure 2 Characteristics of failed implants.6
The behavior of the patients is decisive in the appearance of peri-implant pathologies. It is possible that unconscious manifestations such as bruxism, stress, or undiagnosed malocclusion problems favor treatment deterioration. But above all, it is the careless attitude towards dental health that leads to new failures. People forget that the placement of implants is the result of the deterioration of natural parts. After an implantology treatment, if they continue to incur in a lack of oral hygiene, or in harmful habits such as smoking and poor nutrition, it is very likely that they will suffer from implant diseases (Table 1).7
|
Age |
No. of implants |
Failure |
% |
|
<40 |
19 |
1 |
5,3 |
|
40-59 |
221 |
10 |
4,5 |
|
>60 |
131 |
8 |
6,1 |
|
Total |
371 |
19 |
5 |
Table 1 Failure percentage according to age6
Biological failures or complications occur when osseointegration is not maintained after implant installation or when it is not maintained over the years. In relation to failures or mechanical complications, various factors have been suggested as possible causes, such as: inadequate adaptation of the prosthetic structure, bruxism, occlusal misalignments, design of prosthetic structures, implant location, implant diameter, etc. The fact that early failure occurs is usually due to causes such as overheating of the site, lack of primary stability at the time of implant placement, premature loading or microbiological contamination that alter the normal healing process of the soft tissues and prevent the intimate union between the bone and the implant from forming. It is concluded that non-osseointegration and peri-implantitis were the most frequent causes of failure in the initial phase of treatment. Regarding the anatomical regions of the oral cavity, the failure rates were low and the survival and success rates were high. To avoid the failure of dental implants, three factors must be taken care of: the surgical technique, the quality of the patient's bone and the design of the prosthesis.8
Implants can have different dimensions and shapes, which vary in length and width and allow for a greater diversity of post-implant prosthetic restorations. The modification in terms of length and width occurred due to the various anatomical situations of the alveolar ridge and the proximity of structures such as the maxillary sinus and the inferior alveolar nerve. Some authors mention that implants between 10 mm and 13 mm long present the best long-term results, as long as they are accompanied by regular diameters. Currently, short implants are an alternative to face difficult clinical situations, allowing vital structures to be avoided, eliminating the need to perform complex surgical procedures, increasing placement possibilities, reducing time and costs.9
Regarding the diameter of the implants, the regular diameter implant presents 5% more survival when compared to reduced diameter implants. In the year 2000, Polizi et al., suggested that the greater the diameter of the implant, the greater the contact surface and therefore the greater the chances of success in the treatment. From a biomechanical point of view, Vigolo & Givani concluded that narrow implants have a 25% lower resistance to fracture than regular diameter implants.9
The use of implants has boomed in recent years, however, just as there has been an increase in demand, there has also been an increase in their failure, there are multiple reasons involved for this, such as; deficiencies in the quantity and quality of bone, pre-existing bone pathologies, poor surgical technique, inadequate implant, smoking habit, among others. Peri-implant mucositis and peri-implantitis are the leading causes of complications in implants; patients with chronic degenerative diseases, smokers, and poor hygiene are considered patients at risk for peri-implantitis.5
The presence of systemic diseases such as diabetes, states of immunosuppression, cancer treatments, etc. patients with chronic degenerative diseases such as poorly controlled diabetes are considered patients at risk of presenting peri-implantitis, and this is because they have an immune response as well as a poor healing process, this confirms it. Ferreira et al., by indicating that periodontitis and diabetes increased the risk of peri-implantitis.10
Having a history of smoking is another factor that can cause damage to peri-implant tissues, since nicotine is known to impair protein synthesis and affect the adhesion capacity of gingival fibroblasts, which leads to alterations in maintenance and remodeling of the connective tissue, if poor hygiene is added to the above, which favors the formation of bacterial plaque and the entry of microorganisms into the implant placement area, the risk of developing peri-implantitis increases considerably. Kasat & Ladda conducted a review on the harm of tobacco in which they indicated that the failure rate of implants in smokers ranges from 6.5 to 20.10
The placement of dental implants today is a widely used rehabilitation option that restores both functionality and aesthetics that is dissipated by losing the dental organs, however not all patients are candidates for placing this type of attachments, not only for the presence of both the quality and quantity of bone present, if not due to both local and systemic health conditions of the patient, for which reason carrying out an adequate assessment, control and follow-up of patients with implants becomes essential for the success of the themselves.10
Among the most common complications in dental implants is the appearance of chronic inflammation that affects the hard and soft tissues around the implants, this situation is known as peri-implantitis. In recent years, some cases of the appearance of squamous cell carcinoma in peri-implant areas have been observed, and although there are few cases in the literature, it is convenient to establish what relationship implants may have in the development of this disease in patients with predisposing factors, since that in most of them the disease begins with the symptoms of peri-implantitis.11
Peri-implantitis is a condition characterized by inflammation and loss of supporting tissue around an implant. This is a catabolic condition with or without sepsis or suppuration. The main cause of this disease is the accumulation of dental plaque that begins with gingivitis, later progresses to the formation of periodontal pockets and finally causes bone loss. Other causes that contribute to the development of this ailment are: excessive and/or forced occlusal and lateral overload. The pathogenic agents involved are anaerobic bacteria, among which Peptostreptococcus spp. and Fusobacterium spp.2. Its treatment involves meticulous oral hygiene, plaque control, and local administration of antibiotics.11
In the scientific literature, the appearance of oral squamous cell carcinoma that appears in the areas around the implants is revealed. Those peri-implantitis that do not respond to treatment should be biopsied to rule out a malignant process, especially in patients with other concomitant risk factors.11
According to the reviewed published evidence, it does not appear that the implant itself is an element that causes the formation of squamous cell carcinoma, although the inflammation that occurs in the adjacent tissues may be an important factor that contributes to the development of this disease.11
Before implant treatment is performed, the patient's risk factors must be analyzed and a proper cost-benefit assessment must be carried out. In patients with risk factors, periodic reviews should be performed. In the case of finding a suspicious lesion, a biopsy should be performed with its consequent histopathological examination in order to make a correct diagnosis as soon as posible.11
The carcinoma associated with dental implants appears more frequently in the form of peri-implantitis; that is why it is very important to carry out a rigorous follow-up of the peri-implant areas in order to make a diagnosis of carcinoma in its initial phase if it occurs.11 Peri-implant diseases can be classified into three types: mucositis, peri-implantitis and peri-implant failure.12 Mucositis is defined as a reversible inflammatory reaction in which erythema and inflammation of the peri-implant mucosa is observed, accompanied by bleeding and/or suppuration on probing and increased probing depth (4-5 mm). While peri-implantitis is defined as an inflammatory process that affects the soft and hard tissues that surround an osseointegrated implant, resulting in a loss of bone support around the implants, which is frequently associated with an increase in the probing depth (>5 mm) and the presence of bleeding and/or suppuration on probing. Lastly, peri-implant failure can present with pain, mobility and purulent exudate.12
The term peri-implantitis usually appears in the literature as a synonym for implant failure, although many times, after carrying out the appropriate treatment, the peri-implant disease is stopped with complete healing of the peri-implant tissues. The failure of the implants can be an early failure, related to the lack of intimate bone-implant contact, which would prevent the osseointegration of the implant; or late failure, once the implant has already osseointegrated.12
Peri-implant disease tends to progress faster apically than periodontitis, probably because the defense mechanisms of the gingiva are more effective in preventing the apical spread of pocket microflora than those of the peri-implant mucosa. The most important inflammatory processes occur in the connective tissue, since it is a highly irrigated tissue with a high capacity to attract defensive cells against external agents, due to toxicity of the bacterial components and enzymes, and internal due to the stimulation of the specific and non-specific immunity of the host. When the biological defensive factors or mechanisms are not capable of containing said inflammatory reaction, the destruction of connective tissue and bone will occur due to osteoclastic activity.12
The factors such as smoking or a history of periodontitis, together with poor oral hygiene, are the main causes of peri-implant diseases. A correct diagnosis of the etiology, as well as the appropriate choice of therapy, can stop the progression of the peri-implant disease. After the treatment carried out, periodic control and maintenance of correct oral hygiene will be very important.12
In clinical practice, implant-supported restorations have to continuously withstand forces that tend to separate the bond. These forces are: contacts due to lateral movements, decentered centric contacts of the axis, interproximal contacts, cantilever contacts and non-passive structures.13
Dental implant failure may be related to implant-supported restorations or peri-implantitis. The first one results from technical problems and can be divided into two groups: those related to the components of the implant and those related to the prosthesis. Technical problems related to implant components include fractures of the prosthetic screw. Reports of these complications have increased, and the primary reason has been attributed to undetected loosening of the screw, which may be due to bruxism, overload, or poor prosthetic design. During routine follow-up, loosening of the screws was found in 25% of the patients. Many clinical studies report the loosening of the prosthetic abutment in single teeth as a frequent problem, especially in molars, due to the fact that they present a greater susceptibility to overloads and stress in the implant-prosthetic abutment union. Therefore, the number, position, dimension, design of the implants and the prosthesis are critical factors to consider during treatment planning.13
Experimental data on bite force in humans show that axial forces during mastication can be in the range of 77 to 2,400 N. Lateral force components are less than 100 N. "One can select an average value of 250 N as a typical for the axial component, but with the understanding that any patient can exert significantly more or less force." The average masticatory force is reported to be between 450 N and 550 N in completely dentate patients in the premolar area. A decrease in occlusal force at levels of 200 to 300 N was recorded for patients with fixed and removable implant-supported prostheses.13
The values found in this study corresponding to axial (compressive) forces, both for limit elastic load and for maximum load, exceed the typical values reported clinically, with a statistically significant difference (maximum load) between the groups, although at a clinical level might not be representative. An in vitro study applied vertical and horizontal loads of 30 N to two groups of internal and external connection implants and found almost the same pattern of force distribution under vertical load in both systems.13
For the lateral forces at 45°, with a compression-flexion component, which are the most representative type of load application of the demand that occurs during mastication, the resistance values of the systems were also higher than those found in the literature, even taking into account the wide coefficients of variation. In this test, the external connection reported a better result of resistance to static loads, with average maximum load values of 716 N. A value of 966 N was reported for external connection implants, under loads applied at 30°, until producing the doubling of the prosthetic screw.13
It has been recommended to improve the stability of the screw union by centering the occlusal contacts, reducing the cusp tilt, increasing the diameter of the abutment screw, narrowing the buccolingual width of the restoration, and reducing the placement of prostheses with free ends. However, there are no reports of the stability of the screw joint of the external hexagon system under lateral cyclic loads.13
When observing the data obtained in the tests at 90°, a greater mechanical resistance was found for the CI systems, both for limit elastic load and for maximum load, although no statistically significant differences were found between both groups. In a study with the application of loads at 90°, the external connection presented an increase in tension at the level of the cervical zone under horizontal loads and in the internal connection the tension was located in the apical zone of the implant.13
In the external connection design, the prosthetic screw is the only element that holds the abutment and implant together. This situation makes the design inherently weak to torsional forces. In the internal connection, friction plays an important role in maintaining the integrity of the connection, in addition to the torque (preload) applied during the tightening of the pillar.13
A study on the in vitro evaluation of the bond strength of the tapered implant to the abutment in 2 commercially available implant systems (ITI Straumann with an 8° internal connection and Astra Tech ST with an 11° internal connection), reported that implants ITI presented screw head fracture while Astra implants only suffered deformation of the internal cone and slight torsion within the neck of the implant. Within risk situations, it is said that the internal connection, in combination with an inadequate treatment plan and overload, can lead to fracture of the implant Wall.13
Although mechanical, clinical and microbiological advantages and disadvantages, among others, have been described for both internal and external connection systems, the actual biomechanical influences around implants have yet to be examined in detail. It is suggested that new designs should be developed using scientific methods including clinical evaluation and not simply based on speculation and professional opinion. Finally, a systematic review of the literature, working with the null hypothesis that there is no difference in clinical behavior between various types of root-shaped osseointegrated dental implants, searched for all controlled studies comparing osseointegrated implants with different materials, shapes, prosthetic connections and surface characteristics, with a follow-up of 1 to 3 years. The results showed, in ten studies analyzed, 428 patients and 9 different types of implants, that no statistically significant differences were found for failures, marginal bone level changes, and peri-implantitis. In conclusion, it was defined that there was no evidence that any of the implant systems evaluated was superior to another.13
Dental prostheses are the most widely used artificial means to replace missing teeth, in order to restore the necessary harmony, both functional and aesthetic. At a functional level, dental implants respond much better since they do not move, nor do they run the risk of detaching, being firmer and safer, allowing the patient to restore their functions of eating, drinking and leading a normal life immediately from the day of their installation.
Currently these have great successes, however, there are rates of failure that result in the loss of installed dental implants.
Accordingly, the main factors that we must take into account to avoid failure in the installation of dental implants are the experience and skill of the operator and the characteristics of the implants. Prasant MC, Thukral R, Kumar S, et al. The fact that early failure occurs is usually due to causes such as overheating of the site, lack of primary stability at the time of implant placement, premature loading or microbiological contamination that disrupts the normal healing process of soft tissues and prevents the intimate union between the bone and the implant from ever forming.
The methods followed in dental implant surgery depend on the type of implant and the state of the jaw, during this said surgery different procedures must be covered to guarantee its success. As indicated by this author. It is possible that the dental implant does not integrate correctly with the bone due to poor surgical technique, which compromises sterilization, overheating of the site, poor fit in the abutments, lack of passivity or incorrect design of the prosthesis. In general, so that we can opt for a successful installation of a dental implant, we must take into account all these characteristics, mainly obtaining a solid support, being careful in each step.
Martín-Granizo López, points out that Late postoperative complications and the causes that can lead to the failure of dental implants could be divided into three large groups of factors: those associated with bacterial infections, occlusal (mechanical), as well as systemic and psychological.
In this sense, implants affected by peri-implantitis, or infection of dental implants by bacteria, are the main causes of complications. They are usually considered as late failures, which can lead to their removal. All this also depends on the state of bone loss and the clinical state of the area. To avoid this type of complications, we must identify patients with a greater or lesser risk of developing peri-implantitis, and adequate periodic maintenance of the implants.
Another important factor that influences the failure of dental implants is smoking, tobacco is a risk factor for the appearance of periodontal diseases. Smokers are at greater risk of loss of dental attachment.
In the event that there is not an adequate and sufficient osseointegration, there may be movement of implants and radiolucency around it, this being a complication, due to the fact that mechanical destruction of any of its components or structure of the implant may occur.
There were 371 implants placed in 123 patients that were evaluated, with an average of 3 implants per patient. There were 33 men with 94 implants (25.3%) attended and 91 women with 277 implants (74.7%).The average age of the patients was 55.1 years old.6
According to their systemic condition, diseases that could influence the prognosis of the implant were identified. A patient with osteoporosis was treated, 4 patients who had received medication with bisphosphonates, who suspended their treatment and waited the time indicated by their treating physicians before starting the dental treatment for dental implant placement, and 7 patients with controlled diabetes. No implant failures were observed in these systemically compromised patients.6
It is observed that the first molars are the most replaced by each quadrant. Dental units 16 and 46 are the most replaced, with 29 implants each of the implants placed, 19 (5%) failed and 352 (95) were successful.6
We conclude that the factors that have the greatest influence on the evolution of the implants and affect the immediate result are heavy smoking, implant placement under a torque of less than 15 Nm, and in a flapless surgery. Therefore, the hypothesis is discarded.6
The fact that early failure occurs is usually due to causes such as overheating of the site, lack of primary stability at the time of implant placement, a premature loading or microbiological contamination that disrupts the normal healing process of soft tissues and prevents the intimate union between the bone and the implant from ever forming.3
The success criteria for dental implants are difficult to describe. Exogenous and endogenous factors are established, related to the surgeon's experience, as well as the presence of bone reabsorption or the need for bone grafts. But it is also true that they have been changing over time and perhaps it is more correct to speak of an implant health quality scale and relate the categories of this scale with the prognosis of existing conditions in our patients.
Radiation, smoking, cardiovascular disease and HIV do not represent contraindications for implant placement, but cases should be analyzed and the risks of the procedure explained to the patient.
Success and failure are dynamic conditions linked to time and require periodic evaluation. The main criteria to evaluate the quality of health of the dental implant are mobility and pain, the presence of any of them compromises the implant to a great extent and in many cases its removal is indicated. Implant failure is easier to describe and leads to the analysis of a series of clinical parameters and indices. The presence of pain, mobility, progressive uncontrolled bone loss and peri-implant radiolucent image confirm implant failure in most cases.
None.
None.

©2023 Palima, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.