Journal of
eISSN: 2373-4345


Research Article Volume 1 Issue 1
Dental Biomaterials, College of Oral and Dental Medicine, Misr University for Science & Technology, Egypt
Correspondence: Nagy Abdul-Samee Abdul-Hameed, Dental Biomaterials, College of Oral and Dental Medicine, Misr University for Science & Technology, Al-Motamayez District, P.O. Box: 77, 6th of October City, Egypt
Received: April 17, 2014 | Published: May 7, 2014
Citation: Abdul-Hameed NAS. Evaluation of thermoplastic resin as a new pattern material for posts: dimensional accuracy and detail reproduction. J Dent Health Oral Disord Ther. 2014;1(1):10-13. DOI: 10.15406/jdhodt.2014.01.00005
Traditionally, dark-cure (cold-cure) acrylic resin is used as pattern material for cast post and core. A new post system that incorporates a specially designed plastic support rod and a thermoplastic resin has been introduced to the market and is claimed to simplify the procedure for cast posts fabrication.
The aim of the present work was to evaluate the dimensional accuracy and detail reproduction of thermoplastic resin when used as pattern or impression material for posts, and the amount of solid residue after ignition when used as pattern material.
Materials used were thermoplastic resin (Trigger Feed, Glue Gun, China), polyether rubber base material (Permadyne, ESPE), and Duralay acrylic resin (Relience Dental Manufacturing Co). A machined cut circular stainless steel (st.st) mold similar to those described in ADA specification No. 19 and BS 4269 was constructed with two horizontal and three vertical sharp line grooves. The scribed horizontal lines were used to measure the dimensional changes. The scribed vertical lines provided a measure of surface detail reproduction. A ring of 5mm thickness was machined cut that placed on the circular st.st. mold shoulder leaving 2mm thickness for the impression material. Thirty impressions of st. st. die were made, ten from each material used in the study. Three readings were made for each impression disc to the nearest 0.001mm using a travelling microscope (Unitron Bi5-3174) at ×10 magnification. The percentage of dimensional change was calculated. Surface detail reproduction was evaluated, by inspecting each vertical line under a travelling microscope (Unitron Bi5-3174) at X10 magnification using low-angle illumination. The reproduction was considered acceptable if two of three of the vertical lines were reproduced continuously and well defined for the full length. Two grams of thermoplastic resin and two grams of cold cure resin were ignited separately in porcelain crucible at 700°C. The nonvolatile residue left was weight using electronic balance.
Results of the study showed that there was no statistically significant difference in surface detail reproduction as well as dimensional stability during hardening between thermoplastic resin, cold-cure resin pattern material or polyether elastomeric impression material. There was no statistical significant difference in the percentages of solid residue left after burning out of thermoplastic resin or cold cure resin.
Clinical relevance: Thermoplastic resin is a cheap, low cost, easily manipulated, elastic material, and as accurate and dimensionally stable as the rigid cold cure resin pattern. Hence, it must replace the traditional post-core pattern materials or impression materials for post hole(s).
Keywords: thermoplastic resin, pattern materials, post, dimensional accuracy, detail reproduction
Severe destruction of coronal portion of the tooth with pulp involvement needs endodontic treatment followed by restoring the tooth to its normal function. Such restorations involved posts-core construction with cast full crowns. Custom-made posts and cores are more preferable and popular, than ready made one, for the restoration of endodontically treated teeth especially when flared or elliptical canals exist. Custom-made post can be cast from a direct pattern or indirect one.1−3
A direct technique utilizing autopolymerizing resin,1 light-curing resin4 or hard dental inlay casting wax are recommended for single canals whereas an indirect procedure utilizing soft dental inlay casting wax is more appropriate for multiple canals.5 Post pattern is made directly in the canal with the use of a cold-cure resin and a brush-bead technique. The canal is lightly lubricated, and a loose fitting plastic dowel is typically used to support the resin.1 Light-curing resin materials are available for the fabrication of patterns for cast metal post-cores. The materials are provided as high or low viscosity pastes or liquids and are based on a diurethane methacrylate oligomer with 40% to 55% resin filler. A pattern is fabricated by applying the resin in layers and curing in a light chamber or by using a handheld light-curing unit.4 Hard inlay pattern wax is also used for construction of direct pattern of cast post and core.6 Resin pattern has higher strength, higher resistance to flow and good dimensional stability than wax.4
Difficulties that can be encountered with the use of these materials include voids in the pattern, locking of the pattern into undercuts or collateral canals, and fracture of the resin or the wax during removal. Furthermore, the use of cold-cure resin is time-consuming to polymerize. A new post system (cast posts and plastic, Merritt EZ Cast Post Inc., Hendersonville, N.C.) that incorporates a specially designed plastic support rod and a thermoplastic resin has been introduced to the market and claimed to simplify the procedure for the fabrication of cast posts.7
The aim of the present work was to evaluate the dimensional accuracy and detail reproduction of thermoplastic resin when used as pattern or impression material for posts, and the amount of solid residue after ignition when used as pattern material.
Materials used were thermoplastic resin (Trigger Feed, Glue Gun, China), polyether rubber base material (Permadyne, ESPE), and Duralay acrylic resin (Relience Dental Manufacturing Co).
Specimen preparation
A machined cut circular stainless steel (st.st) mold (Figure 1) similar to those described in ADA specification No. 198 and BS 42699 was constructed with two horizontal and three vertical sharp line grooves. The horizontal lines were numbered d and d’ and the distance d-d’ is measured on the st.st. die (Figure 2a) and compared with that on the pattern (impression) discs (Figure 2b) to give an indication of dimensional changes. The vertical lines are numbered 1, 2 and 3. They are ‘V’ shaped in section and are 0.075, 0.05, and 0.02mm wide respectively. The scribed vertical lines provided a measure of surface detail reproduction. A ring of 5 mm thickness was machined cut that placed on the circular st.st. mold shoulder leaving 2 mm thickness for the impression material.

Thirty impressions of st. st. die were made from each material used in the study. The stainless steel die was warmed to 37°C, each time before loading with the materials under investigation, to simulate oral conditions. The rubber base and duralay impressions were made following manufacturer’s directions. Thermoplastic resin impressions were made. Softening the resin using electrical gun (Figure 3) and care was taken to push the impression material ahead of the gun tip inside the st.st. mold. Pressure was exerted on the top of the mold using a flat metal piece of 500 grams weight that lined with polyethylene strip. The entire assembly is kept in water bath at 32±1°C in accordance with ADA specification No.19 for 10 minutes.
valuation of dimensional accuracy
Three readings were made for each impression disc to the nearest 0.001 mm using a travelling microscope (Unitron Bi5-3174) at ×10 magnification. The percentage of dimensional change was calculated by the following equation:
valuation of surface detail reproduction
Surface detail reproduction was evaluated one hour after removal of the impression from the water bath. Each vertical line (numbered 1,2, and 3) was inspected under a travelling microscope (Unitron Bi5-3174) at X 10 magnification using low-angle illumination.
The reproduction was considered:
Measurements of the amount of non-volatile residue
Two grams of thermoplastic resin and two grams of cold cure resin were ignited separately in porcelain crucible at 700°C. The nonvolatile residue left was weighed using Metler electric balance (sensitive to 0.0001mg) according to the technique recommended by ADA Specification No 4 for inlay pattern waxes.11 The percentage of solid residue was calculated using the following formula:
Statistical analysis
The dimensional accuracy data were evaluated statistically using one way analysis of variance (ANOVA). Reliability of the dimensional accuracy for observers was taken against the standard stainless steel die.
The amount of solid residue data was collected and comparison of means was conducted by the use of the unpaired t-test. All tests were performed at a confidence level of 95%.
Dimensional accuracy
There was no statistically significant difference (P>0.05) in dimensional accuracy between the three types of materials used and the standard die or between any of the materials used (Table 1). Dimensional change values ranged from -0.22 % to -0.26 % for the materials used. All values were within the ADA standards of less than 0.5 % shrinkage for the non-aqueous elastomeric dental impression materials.
Polyether |
Duralay |
Thermoplastic resin |
Calculated F value |
Tabulated F value |
Pvalue |
|||
|---|---|---|---|---|---|---|---|---|
X |
SD |
X |
SD |
X |
SD |
|||
0.22 |
±0.081 |
0.23 |
±0.095 |
0.26 |
±0.073 |
0.00064 |
3.3541 |
P > 0.05 (NS) |
Table 1 One-way analysis of variance (ANOVA) of the dimensional accuracy (linear dimensional change %)
X: Mean; SD: Standard Deviation; NS: Non Significant Difference P>0.05.
Surface detail reproduction
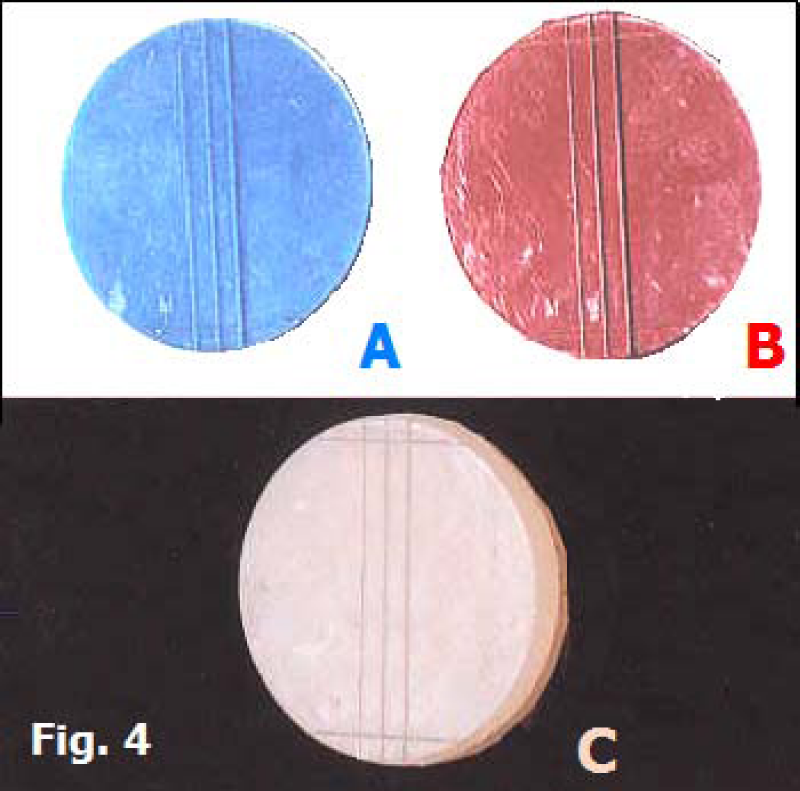
All the impressions proved to have acceptable surface detail (Table 2). The lines were clearly reproduced with distinct edges along their entire length (Figure 4a for polyether elastomeric impression material, Figure 4b for cold cure resin and Figure 4c for the thermoplastic resin).
Result |
Polyether |
Duralay |
Thermoplastic resin |
Acceptable |
10 |
10 |
10 |
Table 2 Surface detail reproduction
The amount of non-volatile residue
The percentage of solid residue (Table 3) left after burning out of thermoplastic resin was 0.079±0.004 and that of cold cure resin was 0.082±0.002. There was no statistically significant difference between them in this respect (P>0.05). Each one was within the limits of ANSA/ADA Specification No. 4 for dental inlay casting wax, which limits the non volatile (solid) residue be not more than 0.10% of the original weight of the specimen at an ignition temperature of 700°C.12
Duralay |
Thermoplastic resin |
Calculated tvalue |
Tabulated tvalue |
P value |
||
|---|---|---|---|---|---|---|
X |
SD |
X |
SD |
|||
0.082 |
±0.002 |
0.079 |
±0.004 |
0.0386 |
2.101 |
P>0.05 (NS) |
Table 3 Unpaired t-test of the amount of nonvolatile residue (%)
NS: Non significant difference P>0.05.
Advantages of using thermoplastic resins as a direct pattern material in manufacturing of cast post and core are: low cost, the amount of time needed for its cooling and solidifying is 1 minute which is much less than the time needed for polymerization of cold-cure resin or incremental building of the inlay pattern wax, good flow in its molten state which leaves the surface of the post pattern free from voids that may affect the accuracy of the investing procedures, and enough elasticity that allows its withdrawal from undercut. Another merit for the thermoplastic resin is that it could be used as an impression for the post hole preparation for the indirect technique.7 This paid our attention to evaluate its dimensional accuracy, detail reproduction and the amount of solid residue left after ignition.
In this study the test material was compared with cold cure resin (Duralay) because it is the most commonly used material for direct pattern construction and with polyether rubber base impression material because it is one of the most dimensionally stable impression material.
Although thermoplastic resin produced the largest dimensional changes (0.26±0.073) but no statistical significant difference (P>0.05) was found between it and other materials tested (Polyether 0.22±0.081 & Duralay 0.23±0.095). The contraction of cold cure resin and polyether rubber base during their setting could be attributed to the cross-linking and rearrangement of bonds within and between polymer chains.8 The contraction of thermoplastic resin during its hardening is explained on the basis of coefficient of thermal expansion.12 Furthermore, the present work showed that the dimensional changes of the investigated materials were within the ADA specifications No. 19 for the non-aqueous elastomeric impression material.8
Regarding detail reproduction, all materials used in this study were acceptable because all the three vertical lines were reproduced continuously and well defined for the full length. This may be attributed to the high flow, of all materials investigated, at the time of mold packing. There was no statistically significant difference of the solid residue left after burning out of thermoplastic resin and cold cure resin (P>0.05). Moreover, these solid residues were within the limits of ANSA/ADA Specification No. 4 (ISO 1561) for dental inlay casting wax. This could be attributed to the fact that both of them are formed of organic materials. The coloring materials in the cold cure resin that used as pattern material (e.g. Duralay), are also organic one.
Within the limits of this work, the following conclusions were derived from the results:
None.
The author declares that there is no conflicts of interest.

©2014 Abdul-Hameed. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.