Journal of
eISSN: 2373-4345


Case Report Volume 15 Issue 3
Department of Fixed Prosthodontics, Faculty of Dental Medicine of Monastir, University of Monastir, Research Laboratory of Occlusodontics and Ceramic Prostheses, Tunisia
Correspondence: Dr. El Ayachi Islam, DDM, Department of Fixed Prosthodontics, Research Laboratory of Occlusodontics and Ceramic Prostheses LR16ES15, Faculty of Dental Medicine, University of Monastir, TN 5000, Tunisia
Received: July 04, 2024 | Published: July 17, 2024
Citation: Islam EA. Esthetic rehabilitation of a patient with moderate fluorosis: a digital workflow. J Dent Health Oral Disord Ther. 2024;15(3):123-126. DOI: 10.15406/jdhodt.2024.15.00623
Dental fluorosis is considered as a worldwide dental health problem. Its prevalence is increasing in different parts of the world. It is described as a disorder of enamel development caused by chronic and excessive exposure to high concentrations of fluoride during the formation of enamel, which could be responsible for the hypermineralization of enamel increasing its porosity. It is clinically identified as white lines covering all or a part of the enamel surface. Posteruptively, these subsurface porosities may attract various extrinsic stains and /or bacteria and change the color of the affected enamel. In some cases, occlusal trauma may cause its detachment. The therapeutic management of dental fluorosis includes bleaching, microabrasion, veneering and crowning. The choice of the appropriate alternatives is closely linked to damages within the enamel matrix. Thylstrup-Fejerskov categorized these damages with severity scores based on their histological features. Mild-to-moderate fluorosis are often managed with bleaching and/or microabrasion, while severe fluorosis, is generally treated by veneering and crowning.
The clinical case describes the treatment of discolored teeth with veneers using lithium disilicate-reinforced glass-ceramic material and highlights the different guidelines to optimize veneer bonding on fluorosis teeth.
Keywords: enamel, porosity, color, teeth, crowning, fluoride
Excessive exposure to a high amount of fluoride during enamel development is the main cause of enamel demineralization and porosity, causing dental fluorosis. The prevalence of fluorosis within a population is from 2.1% to 74.7%.1 Dental fluorosis is a major problem in Tunisia, particularly in the endemic areas where phosphate fields are concentrated.2
Its pathogenesis describes a complex process involving genetic and environmental factors.3s This non-carious condition affects both dentitions. Permanent teeth have the most profound effects.4 Dental fluorosis is mainly manifested by white to dark brownish discolorations covering all or a part of the surface of the teeth causing pores of varying sizes in the enamel matrix.
The sub surface porosities in which the enamel becomes mottled and brittle is associated to the hypermineralization of the outer layer of the enamel.5,6 Based on the severity of enamel damage, many classifications of dental fluorosis were proposed.7 Dean and Thylstrupamp; Fejerskov are the most commonly implemented indices for measuring clinical manifestations of dental fluorosis.8
Authors tried to standardize clinical situations to include this pathological worldwide condition in the daily life practice of clinicians. They provided assessment criteria to each they associated therapeutic recommendations. There are various treatment options available to treat fluorosis depending on their extent and severity such as: bleaching, microabrasion, veneers, or full crowns.
Minimally invasive methods such as whitening, microabrasion and resin infiltration alone or in combination proved to be effective in mild cases according to Dean's Fluorosis Index.9 However, mini invasive procedures are ineffectual in moderate to severe cases.100,11 Prosthetic approach is often required to treat advanced phases of dental fluorosis.12
Porcelain veneers are able to solve esthetic and functional problems as well as fulfilling the need for adequate retention.13,14 The versatility of veneer designs allows them to be used as an alternative to full coverage crowns while preserving maximum remaining tissue. Despite the overwhelming success that clinicians had with porcelain veneers, concerns have been raised about the bonding ability of resin cements to fluorosed enamel. It has been demonstrated better shear bond strengths with total etch bonding systems than self-etching systems.15
This clinical case describes the treatment of discolored teeth with veneers using lithium disilicate-reinforced glass-ceramic material and highlights the different guidelines to optimize veneer bonding on fluorosis teeth.
A 28-year-old Tunisian woman was referred to our prosthodontics department in the dental clinic of Monastir. She had discolored teeth and diastemas.
The intraoral examination showed good oral hygiene, a bilateral class I molar occlusal relationship, slight diastemas involving the anterior region of the maxillary (Figure 1).
Clinical and radiographic examination demonstrated sound periodontal conditions. The distribution of the opaque white yellowish spots among her anterior and posterior teeth associated to pits and punch shaped porosities supported the diagnosis of dental fluorosis with a Tooth Surface Index of Fluorosis score of 5. Subsequently, a digital intraoral scan was made using a 3 shape trios 3 scanner. Full-face frontal and profile photographs of the patient were taken (Figure 2). An Exocad digital smile design software was referred to evaluate dentogingival discrepancies and manifest the patient’s demands.
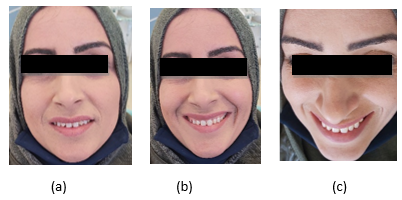
Figure 2 Photographs of the patient (a) Face with shallow smile (b) Face with a wide smile (c) The 12 o’clock view.
A 3D-printed model was fabricated to create silicone for intraoral mock-up. Threw the mock up, the patient agreed to smile enhancement using porcelain veneers for her anterior teeth given that she desired an optimum aesthetic and a long-term result.
The veneers would be placed on the patient’s upper teeth up to first premolars of both sides of the maxillary. The adhesive provisional mockup is then prepared using a round diamond burr to calibrate the depth of enamel that needed to be removed. Reduction grooves were then marked with a pencil before the removal of the mock up. Teeth preparation was kept in enamel at a depth of 0.7 mm using a 1 mm diameter tapered diamond burr. Finish lines were kept at the level of gingival margins. The incisal butt margin preparation was up to 1.5mm. The proximal preparations were extended beyond the contact area to ensure the diastemas closure.
After finishing, the sharp lines and point angles were rounded. Gingival retraction was performed for digital impression of the maxillary arch (Figures 3 & 4). We used VITA Easy shade System to select the color of our future restorations (Figure 5). Provisional restorations were then needed to protect teeth until the trying day.

Figure 3 Mini-invasive preparation (a) Guided preparation through the mock up (b) Preparation aspect after polishing.
Emax CAD veneers were fabricated and tried in for shade, marginal adaptation and color (Figure 6 & 7). They were tried-in individually using glycerin before being tried in collectively to appreciate the esthetic change of the smile.
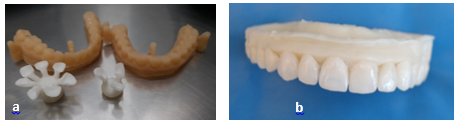
Figure 7 Computed aided manufacturing of the veneers (a) Manufacture casts with 10 freshly manufactured veneers (b) Emax CAD veneers after being polished and placed onto their positions in the digital cast.
The patient was satisfied with results and was ready for final cementation. The laminate disilicate veneers were arranged on a silicon sheet denoting the position of the tooth in the arch to ensure their correct placement. The internal surfaces of the veneers were etched with a 10% Hydrofluoric acid for 60 seconds, rinsed thoroughly using liberal amount of water and dried. They were then, coated with a Silane coupling agent. A rubber dam was placed on teeth and stabilized with retraction cords and floss ties.
Tooth conditioning started with the etching of the teeth using a 37% Phosphoric Acid for 15 seconds, air dried and bonded with a VARIOLINK dual cure resin cement agent (Figure 8). Veneers were spot cured for 5 seconds initially to allow the excess cement to be removed. A complete curing was done for 20 seconds. The occlusion was checked in centric and eccentric positions before the final polishing. The patient was satisfied with her new smile. She was brought to control after two weeks from final cementation (Figure 9).
Fluorosis is a hypo-mineralization of the tooth due to chronic fluorine intoxication during the amelogenesis period. It is clinically manifested by a symmetry of the lesions, a dyschromia, and sometimes porosities and white spots.16,17
The discolored and pitted aspect of fluorotic enamel is the most common reason for patients to seek treatment.18–21 Several management strategies have been proposed for teeth with varying alterations such as bleaching, microabrasion, composite restorations, veneering and crowning. It depends on how advanced the fluorosis is.22–25 Theses interventions could be used separately or in combination to alleviate the effects of this dental disease.
Several indices have been referred to describe the clinical appearances of dental fluorosis. The most widely used are Dean's and Thylstrup, Fejerskov (T-F index) indexes. Akapta suggested for mild fluorosis with T-F score of 1-2 to be treated by bleaching as the superficial location of the subsurface porosities makes it possible for bleaching agents to penetrate. This treatment is less invasive.26
At T-F scores of 3-4, the subsurface porosities may entrap extrinsic stains into deep and make them unavailable for bleaching agent. In 2001, Akapta suggested the microabrasion technic to control the removal of superficial stain from enamel. Microabrasion is often combined with bleaching to be more effective.26 Teeth with TFI = 4 that suffered from high occlusal trauma, may have the potential to transform to T-F score of 5.22 The hypomineralized layer could rapidly abrade away.27
In these cases, microabrasion should be tried first, and if ineffective, the tooth should then be treated by veneers. Porcelain veneers are conservative and biocompatible restorations. They are also reported to be viable restorations with 93.5 % in a 10-year estimated average survival rate.28–30
For teeth with TFI = 5-7 veneering is suggested when less than 50% of the enamel surface has been lost and so in teeth with TFI = 8-9, the fluorosed tooth should be crowned.31 In this case, teeth have a T-F score of 5. The porcelain veneers, were chosen for their highly aesthetic income, biocompatibility, durability and high translucency. However, the hypermineralized fluorotic enamel, where hydroxyapatite is replaced with fluorapatite, is expected to be more resistant to etching.25,32,33
To optimize veneer bonding, it is essential to follow the recommendations carefully:
For the choice of adhesive system: Etching and rinsing systems (M&R) is much more effective for enamel-resin bonding and more stable over time than the Self-etching systems (SAM) for fluorite teeth because the bonding material penetrates 3.5um into the enamel when using phosphoric acid (MR), while the material penetrates only 1um when using self-etch (SAM).25
For the application time with phosphoric acid: In vitro studies showed for moderate fluorosis, it is recommended to double the enamel etching time (30 seconds) with phosphoric acid in order to obtain an effective bonding strength and to remove the outer layer of hyper-mineralization 50 to 80mm thick.21,34
However, in the case of severe fluorosis, increasing the etching time may decrease the surface roughness and depth profile, which may result in a less effective micromechanical enamel surface for effective bonding.35
Another study is focused for the concentration of ortho-phosphoric acid. It showed that Maximum bond strengths were achieved when phosphoric acid of 40% concentration was used. But too high a concentration can conversely lead to the opposite, leading to an apparent decrease in adhesion.35
De-processing is the application of sodium hypochlorite NAOCL at 5.25% for 60 seconds on the fluoride enamel before etching to get more effective bonding and higher bond strength for fluorotic teeth.35
Dental fluorosis is a debilitating condition that has detrimental effects on esthetics and psychology of the patients. Various treatment options are available nowadays. They could be used separately or in combination to attempt maximum esthetic results. Porcelain veneers are esthetic, conservative and viable option for the treatment of moderate to severe fluorosis. A single treatment modality may not suffice and there may be a need to opt for a multi-treatment approach.
None.
The author declares there are no conflicts of interest.

©2024 Islam, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.