Journal of
eISSN: 2373-4345


Research Article Volume 1 Issue 5
Department of Oral & Maxillofacial Surgery, Government Dental College, India
Correspondence: Amrit Pal Singh, Government Dental College, Jammu, India, Tel 918000000000
Received: October 10, 2014 | Published: October 27, 2014
Citation: Singh AP, Shah AA, Ahmad I. Efficacy of interpositional arthroplasty with temporalis myofascia flap in treatment of TMJ ankylosis. J Dent Health Oral Disord Ther. 2014;1(5):152-156. DOI: 10.15406/jdhodt.2014.01.00032
Aims and objective: The present study was done to evaluate the efficacy of interpositional arthroplasty with temporalis muscle and fascia (myofascia) flap in preventing the re-ankylosis, to evaluate the growth of mandible, and to assess Al-Kayat and Bramley’s incision for its versatility in allowing muscle transfer and excellent exposure of the joint.
Materials and Methods: Fifteen patients with ankylosis were treated with interpositional arthroplasty with temporalis myofascia flap. Maximum Interincisal Opening (MIO) was measured at different periods, i.e. preoperative, intraoperative, immediate post operative, 1 month post-operative, 6 month post-operative, 1 year post-operative. Pain was measured using Visual analogue scales in closed mouth position (spontaneously) & on mouth opening. Six cephalometric points were taken for evaluating the mandibular growth.
Results: A statistically significant difference of 30.73mm (p<0.001) was obtained between pre-operative and post-operative interincisal opening after a period of one year follow up. The pain score at different periods of time revealed that the pain incidence significantly reduced to almost zero post-operatively (p<0.5 for closed mouth, p<0.01 for open mouth).
Conclusion: The temporalis myofascia flap is an efficient interpositional material that acts as a barrier and prevents the chances of reankylosis to a greater extent.
Keywords: interpositional arthroplasty, temporomandibular joint, temporalis myofascia flap
MIO, Maximum Interincisal Opening; SMV, Submentovertex
Ankylosis of temporomandibular joint is an affliction which occasions much misery for the unfortunate victim, interfering with the mastication and digestion of food, denying the body the benefits of a balanced diet, and preventing participation in the pleasures traditionally associated with the culinary arts. If the condition develops in childhood, facial deformity brings psychological stress which adds to the physical handicap, thus disturbing family life and creating emotional disturbance”.1,2
Trauma is well proven to be the predominant cause of temporomandibular joint ankylosis. The other causes that could lead to TMJ ankylosis are local or systemic infections (like otitis media in the childhood), tumors, systemic diseases like ankylosing spondylitis, rheumatoid arthritis and psoriasis, and a complication of previous TMJ surgery.3
TMJ ankylosis may be unilateral or bilateral. According to the type of tissue involved it is classified as bony or fibrous ankylosis. Sawhney offered a lucid classification of ankylosis which is helpful in selecting an appropriate, corrective operation.4
Whatsoever may be the type, early surgical correction of the deformity soon followed by jaw mobility exercises should be encouraged in order to get good results out of surgery and also prevent future reankylosis.2
Surgical intervention by resection of the ankylotic mass through gap arthroplasty alone resulted in reankylosis. Attempts have been made to prevent such reankylosis with interpositional arthroplasty. Numerous materials have been interposed between the resected bone surface and articular fossa at the base of the skull. Alloplastic materials such as silicone, silastic, proplast, Teflon, rubber prosthesis, metals, methyl methacrylate; and autogenous material such as full thickness skin, dermis, fascia, auricular cartilage, fat, Lyodura, costochondral graft, metatarsals, metacarpophalangeal joint transfer, sternoclavicular joint transfer and temporalis muscle and fascia have been used.5,6
Non-biologic materials like acrylic though cost effective and less time consuming present the risk of foreign body reactions, hypersensitivity and slippage. Silicone also has a tendency to slip from the implanted position. Lyodura is abandoned due to the possible transmission of Creutzfeldt-Jakob disease.7,8 Autogenous materials present problem of a second surgical site. Temporalis Myofascial flap due to its proximity to the joint and high vascular supply has been considered as one of the best interpositioning materials used.9
The aim of this study was to carry out retrospective and prospective assessment to evaluate the efficacy of interpositional arthoplasty with temporalis muscle and fascia (myofascia) flap in preventing the re-ankylosis, to evaluate the growth of mandible, and to assess Al-Kayat and Bramley’s10 incision for its versatility in allowing muscle transfer and excellent exposure of the joint.
This retrospective and prospective study was conducted in the Department of Oral and Maxillofacial Surgery, Govt. Dental College, Srinagar. Fifteen patients with TMJ ankylosis were included in the study, of which 7 were males and 8 were females with a mean age of 14.2 years (ranging from 5 years to 26 years).
Patients who reported to the Department with a chief complaint of inability to open the mouth were included in the study on the basis of clinical examination and only those patients who presented with a restricted mouth opening secondary to ankylosis were selected for the study (Figure 1).
During this two and a half years period of study (June 2007 to Nov 2010) 15 patients with ankylosis were treated with interpositional arthroplasty with temporalis myofascia flap (Figure 2).
The information that was collected mainly focused on the age at which patient reported to the department and age of occurrence of the condition. A diagnosis of unilateral / bilateral TMJ ankylosis was mainly obtained with the help of extraoral and intraoral examinations and OPG. Rarely PA view and special views like submentovertex (SMV) were used to assess coronoid. CT scan (axial and coronal views) was done in all patients in order to know the medial extent of the ankylotic mass. 3D-CT was used for one patient. Lateral cephalograms were also taken to assess the mandibular growth.
The parameter taken was Maximum Interincisal Opening (MIO) taken at different periods, i.e. preoperative, intraoperative, immediate post operative, 1 month post-operative, 6 month post-operative, 1 year post-operative. Pain was measured on the basis of grades using Visual analogue scales as No pain (0), mild pain (1) VAS 1-4, moderate pain (2) VAS 5-7, and severe pain (3) VAS 8-10. Preoperative pain was measured in closed mouth position (spontaneously) & on mouth opening, followed by 6 months and 1 year later both in closed mouth position & on mouth opening.
Six cephalometric points were taken for evaluating the mandibular growth. Articulare (Ar) to Gonion (Go) for vertical growth of ramus. Gonion (Go) to Pogonion (Pg) for anterioposterior growth of mandible. Point B to Menton (Me) for vertical growth at symphysis region.
Informed consent for difficult intubation and emergency tracheostomy was obtained from all patients/guardians in case of minors. Tracheostomy was done for all patients except one in whom blind nasal intubation was successful.
The operative protocol consisted of
Figure 3 Resection of ankylotic mass by Al-Kayat & P Bramley.10
The study evaluated 15 patients with ankylosis of the temporomandibular joint. Seven (46.66%) patients had only one TMJ involved and 8 (53.33%) patients showed bilateral ankylosis, making a total of 23 joints. Maximum patients (13) reported in first two decades of life. 4 patients reported in the age groups of 1-10 years (26.66%), 9 patients reported in the age group of 11-20 years (60%) and 2 in the age group of 21 to 30 years. Out of the total, 7 (46.66%) were males and 8 (53.33%) were females. All the patients showed etiologic factors with trauma responsible for all the cases of TMJ Ankylosis.
Mean difference of 30.73mm (p<0.001) between pre-operative and post-operative interincisal opening after a period of one year follow up. The results were statistically significant using paired t-test (Table 1).
Time of Assessment |
Mean±SD |
Difference from Pre-Operative |
p-value |
Pre-Operative |
4.2±2.9 |
- |
- |
Intra-Operative |
39.0±3.0 |
34.800 |
<.001 |
Immediate |
26.06±3.3 |
21.867 |
<.001 |
1 Month |
33.33±2.5 |
29.133 |
<.001 |
6 Months |
35.06±2.2 |
30.867 |
<.001 |
1 Year |
34.93±2.2 |
30.733 |
<.001 |
Table 1 Maximum interincisal opening (in mm)
Chart 1 shows pain score at different periods of time. In the closed mouth position the spontaneous pain scores were 0.9 preoperatively, 0.3 and 0.06 at six months and 1 year respectively. When the patient tends to open his mouth, the score was 2.1, 0.6 and 0.2 for preoperative, 6 months and 1 year respectively. This shows that pain incidence has significantly reduced to almost zero post-operatively (p<0.5 for closed mouth, p<0.01 for open mouth).
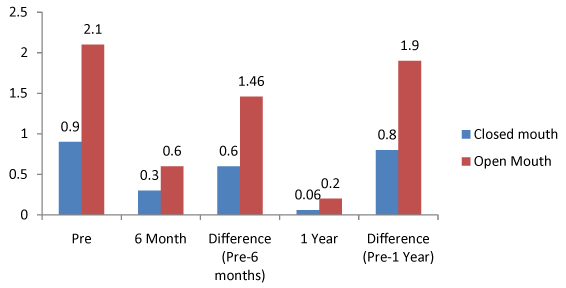
Graph 1 Pain score (vas) at different periods of time.
Paired t- test; P<.05, P<.01 Significant changes
Table 2 shows the mean cephalometric measurements comparing the growth changes of mandible in anterioposterior and vertical directions. Mean growth change in vertical ramus height from Ar-Go in 6 months and 1 year was 0.4±0.5mm and 0.93±0.8mm respectively (p<0.01, significant). Similarly, in anterioposterior direction from Go-Pg it was 0.26±0.4mm in six months and 1.00±0.8mm in 1 year (p<0.01, Significant). Also at symphyseal region between Point B and Me there is significant change of 0.06±0.2mm in six months and about 0.53±0.5mm in 1 year (p≤0.33, p<0.01).
Measurement |
|
Pre |
6 months |
Difference |
1 year |
Difference |
Ar – Go |
Mean±SD |
39.20±4.4 |
39.60±4.3 |
0.4±0.5 |
41.33±3.9 |
0.93±0.8 |
t |
- |
- |
3.45 |
- |
7.79 |
|
P |
- |
- |
<.008 |
- |
<.001 |
|
Go – Pg |
Mean±SD |
54.26±5.2 |
54.53±5.1 |
0.26±0.4 |
55.26±5.1 |
1.00±0.8 |
t |
- |
- |
2.25 |
- |
4.58 |
|
P |
- |
- |
.0406 |
- |
.004 |
|
Point B-Me |
Mean±SD |
18.86±1.7 |
18.93±1.7 |
0.06±0.2 |
19.33±1.4 |
0.53±0.5 |
t |
- |
- |
1.00 |
- |
4.00 |
|
P |
- |
- |
0.33 |
- |
.0013 |
Table 1 Amplitude in mill volts of the Lead-1 of electrocardiography in sheep
*Significant (P≤0.05); NSNot significant (P>0.05)
Ankylosis of the temporomandibular joint makes mastication impossible, deteriorates oral hygiene, and impairs speech. It may also give rise to psychological problems.11
Ankylosis might occur at any age. The reported age distribution ranges from 2 to 63 years, the highest incidence being in the 10-19 year age group.12 In present study 15 patients, about 13 patients reported the onset of ankylosis before 10 years of age; two patients had it at the age of 10 years and 12 years respectively. Thus, about 86.66% of the patients had the onset of ankylosis before the age of 10.
The cases selected were only of intra articular ankylosis for this study and all patients had bony ankylosis. There is unanimous agreement that surgery is the treatment of choice for ankylosis of the temporomandibular joint. The principal surgical procedures are gap arthroplasty, interpositional arthroplasty and joint reconstruction with autogenous or alloplastic materials.
The technique of gap arthroplasty has been supported by various authors like Rajgopal et al.13 & Roychoudhary et al.14 They state that excision of an adequate amount of bone is imperative and if done in that way, interposition of any material becomes unnecessary. Although advantages of gap arthroplasty are its simplicity and short operative time, clinical experience and the literature on ankylosis suggest that in spite of creating a wide gap, the recurrence rate is quite high.15
Hence the concept of interpositional arthroplasty was born, in which an interpositional medium is placed between the severed ends of the bone to act as an obstacle to reunion. A variety of interpositional materials have been used including alloplastic and autogenous materials.
Alloplastic materials have not been very successful in preventing reankylosis. This is because of the fact that although the bone surfaces are prevented from contacting each other, bone can form on both sides and eventually bridge the gap. There is a possibility of rejection of the foreign material also. The use of alloplastic materials also may result in severe degenerative changes and possible systemic release of particles.16,17 To avoid these complications, a variety of autogenous materials are advocated.
We have used Al-Kayat and Bramley10 incision which gives wide exposure with adequate visibility, prevents damage to the nerves and at the same time allows raising a pedicled flap of temporalis myofascia flap. Similar incision has been used by Chidzonga,18 Mehrotra et al.19 & Danda et al.20 in TMJ ankylosis patients in their respective studies.
Su-Gwan determined the efficacy of interpositional arthroplasty with temporalis myofascia flap in the treatment of unilateral temporomandibular joint ankylosis in adults. Patients had a mean preoperative maximal interincisal opening of 15mm. During the last follow up observation after surgery the patients had a mean maximal interincisal opening of 36.1mm. Pre operatively all patients had some degree of pain in the joint involved which significantly decreased after the operation.2
Brusati et al used the temporalis muscle flap to treat the severely damaged TMJ structural components. Using this surgical technique 13 TMJ yielded positive functional results without any complication.21 In the present study, the temporalis myofascia flap was evaluated to be efficient in preventing the reankylosis. Preoperatively the mean interincisal opening was 4.2mm and post-operatively after a period of 1 year follow-up it remained as 34.93mm (P<0.001). Only in one patient the mouth opening was reduced to less than 30mm. This is because the patient did not follow the post operative regimen of mouth exercises and physiotherapy which play an important role in preventing the post-operative adhesions. In this study, preoperatively almost all patients had some degree of pain in joint spontaneously or on opening the mouth. But after the interpositional arthroplasty with temporalis myofascia flap, the pain incidence was significantly reduced. This is in conformity with the findings of Su-Gwan2 who reported a general decrease in pain ratings after the operation.
Sorensen and Laskin22 explained the mandibular growth after ankylosis treatment on the basis of functional matrix theory. Restoration of normal function is therefore mandatory for restoring normal growth. In this data, according to cephalometric measurements, mean growth change in vertical ramus height from Ar-Go in 6 months and 1 year was 0.4mm and 0.9mm respectively (p<0.01, significant). Similarly the body growth in anterioposterior direction from Go-Pg was 0.2mm in six months and 1.0mm in 1 year (p<0.01, significant). Similarly at symphyseal region between Point B and Me there is a change of 0.2mm in six months and about 0.5mm in 1 year. Thus after the release of ankylosis, the mandibular growth continued corresponding to the normal population, but the growth deficit already occurred, could not be made up. There was no accelerated growth spurt as such.
The temporalis myofascia flap is an efficient interpositional material. It is a biologic, autogenous tissue, so there is no question of any rejection. It is a pedicled flap, so it maintains its viability. It can be procured by the same incision used for exposure of the joint. It is easily mobilized and made to cover the complete area of the glenoid fossa. Thus it acts as a barrier and prevents the chances of reankylosis to a greater extent. Also the mandibular growth continues as normal after the temporalis myofascia interposition.
None.
None.
The authors declare that there is no conflict of interest.

©2014 Singh, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.