Journal of
eISSN: 2373-4345


Mini Review Volume 15 Issue 3
Department of Basic Sciences, School of Dentistry, São Paulo State University (UNESP), Brazil
Correspondence: Gabriel Mulinari-Santos, DDs, MSc and PhD, Department of Basic Sciences, School of Dentistry, São Paulo State University (UNESP), Araçatuba 16015-253, SP, Brazil
Received: August 20, 2024 | Published: September 18, 2024
Citation: Mulinari-Santos G, Okamoto R, Botacin PR. Biomechanical analysis of the skull: a didactic analogy with civil construction. J Dent Health Oral Disord Ther. 2024;15(3):151-153. DOI: 10.15406/jdhodt.2024.15.00628
A didactic description is essential for understanding the biomechanical analysis of the skull. Therefore, this article aimed to establish an educational description through an analogy between the structures of the skull and civil construction. The arrangements of buttresses and arches present in both circumstances are fundamental for strengthening and resistance. This didactic approach has the potential to enhance anatomy education with relevance to clinical practice, especially for students and professionals in maxillofacial surgery and implantology.
Keywords: bones, skull, anatomy, masticatory system, biomechanical phenomena
The skull must be able to resist the forces exerted on it, just like a civil construction. In the same way that a building must resist the forces of rain, wind or storm, the skull must also withstand the muscular forces used on it. The structure of the skull is made up of bone tissue, which in turn responds to the stress to which it is subjected.1 According to the fundamental laws of biology, the internal bone structure is a direct response mainly to muscle function.2 An example of this is the practice of physical exercise to improve bone quality and prevent osteoporosis.3 The bone microarchitecture is proportional to the forces applied.1,4 This relationship is accepted as Wolff's law and follows under the fundamental laws of biology.5
The bone is forced to have its resistance and compaction in its smallest arrangement.6,7 Bone shape is influenced by primary and secondary factors.6 Its external shape is directly related to primary factors, while its internal structure is influenced by secondary factors.6 The primary factors are hereditary and determined by genetic influence.6 For example, human skeletons have a similar external shape to the femur or tibia.6 However, the secondary factors for defining the internal structure are variable and determined mainly by the muscular arrangement and systemic conditions.8 Therefore, the bone trabeculae will be arranged according to the direction of muscular forces8. Moreover, aging-related diseases influence the bone microarchitecture.9
The bone trabeculae has its microarchitecture defined to resist the forces to which it is exposed.7,10 Pneumatic cavities, such as the paranasal sinuses, are not capable of withstanding these forces 6. The places where forces are concentrated by muscular forces are reinforced with denser cortical bone or spongy bone with more trabeculae.8 Thereby, the greater the force on a given bone area, the more bone growth will be formed.7,8 A simple illustration is the base of the mandible, where various muscles inserted into this bone result in the formation of a thicker cortical bone.
In clinical practice, bone density may vary according to the bone region, age, sex and systemic disorders.11 Greater forces increase the probability of finding a dense bone.8,11 For instance, the area in the anterior region of the body of the mandible is thick and it can be an area of autogenous bone graft donor. This location is the origin of the mental muscles, which also exert their forces on this region. The action of the medial pterygoid muscles contributes to the strengthening and thickening of this mental region.6 Furthermore, muscular forces also have the purpose of maintaining bone shape.10 Interestingly, the shape of the zygomatic arch can be maintained by the balance of the superior action of the temporalis fascia and inferior action by the origin of the masseter muscle.12,13
In a didactic explanation, the utility of the civil construction analogy can support understanding skull biomechanics. Cortical bone can be compared to reinforced concrete, which is dense and used for areas that require reinforcement and force dissipation, like the foundations of buildings. On the other hand, medullary bone can be compared to clay bricks, which have lower density and are used for support. Cortical bone, like reinforced concrete, is dense and does not have marrow spaces, only allowing for blood vessels and nerves. Meanwhile, medullary bone, like clay bricks, has small hole spaces inside known as medullary spaces.
Therefore, this article aimed to establish an educational description of the functional analysis of the skull, to facilitate teaching and understanding for students and professionals in the health field, especially dentistry and all those interested in the topic.
There is the action of muscular forces on the skull, but also compressive forces coming from the spine.14 In dentistry, it is necessary to understand the forces of the masticatory muscles. These forces are neutralized by the buttresses and arches present in the skull, also like the building structure. In the skull, places designed to resist the greatest forces on the maxilla are the buttresses, and these require a greater amount of cortical bone for this purpose.13 Likewise, the buttresses of buildings are mostly made of reinforced concrete. The arches of the skull and buildings are made to nullify the forces coming from the buttresses. According to the physics, the forces on the arches are dissipated into tangent forces and thus cancel out the forces on the buttresses. Didactically, examples of civil constructions maintained by the buttresses and arches are the Ponte do Gard in France, the Ponte Vecchio in Florence and the Arco da Lapa in Rio de Janeiro. A didactic analogy with civil construction is presented in Figure 1.
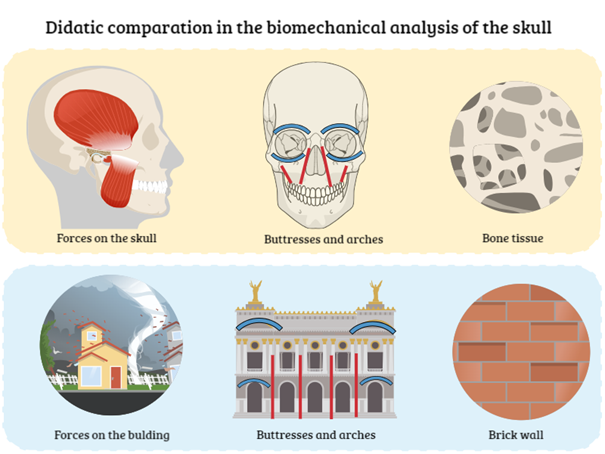
Figure 1 Instructive comparation of the forces, buttresses (red lines) and arches (blue lines) in the skull and building.
The buttresses in the neurocranium are the glabella, zygomatic process of the frontal, mastoid process and external occipital protuberance.6 In the facial skeleton, the buttresses directly receive the masticatory forces on the maxilla, they are canine, zygomatic and pterygoid.6 Orbital arches unite the canine and zygomatic buttresses.6 The superciliary arches are crucial for dissipating chewing forces. In the glabella, bilateral forces are concentrated at a more medial point.6 The arch formed by the alveolar process of the maxilla also nullifies the masticatory force.6 The masticatory force still follows to the base of the skull, where they are also nullified internally by the internal structure of arches in the skull.6 It is worth remembering that in the mandible, the reinforcement areas are named trajectories.6 Knowledge of the structure of buttresses and arches is indispensable for the treatment of facial fractures15 and dental implant placement.16
The reconstruction of buttresses, trajectories and arches is the basis of the treatment of maxillofacial fractures.15 Didactically, a collapsed civil construction first needs the reconstruction of its buttresses, the same occurs in the skull. In Le Fort I fractures with fractures of the canine and zygomatic buttresses, their rebuilding is recommended as a treatment.17 In Le Fort II fractures with rupture of the canine buttresses extend to the glabella, it is also necessary to reconstruct the canine buttresses with titanium plates in the frontal process of the maxilla.17 In Le Fort III, with the addition of recomposing the zygomatic at the frontozygomatic suture.17 The same in the mandible, where the reestablishment of trajectories is crucial.18,19 Therefore, the titanium plates currently used in the treatment of facial fractures are placed to restore the marginal, alveolar and temporal trajectories in the mandible.19
Finally, dental implants can also be placed in areas of higher density to improve initial implant stability.16 This strategy of treatment is mainly needed in individuals with an atrophic edentulous maxilla or mandible. One of these higher-density bone areas in the maxilla are the canine, zygomatic, and pterygoid buttresses. Thus, the buttresses of the maxilla are used for implant placement in edentulous individuals.16 Besides the higher density, these buttresses can maintain themselves even after pneumatization of the sinus. On the other hand, the areas of denser bone are the mandibular trajectories, which can also be worthy for obtaining bone grafts to address bone loss in other areas. Understanding the biomechanics of the skull is crucial to providing an adequate anchorage in dental implant treatment.
It can be concluded that a didactic model establishing a parallel between the structures of civil construction and the skull can facilitate the understanding of anatomy education. Furthermore, knowledge of skull biomechanics is fundamental for students and professionals in the health field, especially in maxillofacial surgery and implantology. In maxillofacial surgery, reconstructing the buttresses is considered a fundamental principle for the treatment of facial fractures. In implantology, buttresses are crucial for providing support for implant placement in edentulous individuals. Thus, this analogy in anatomy education is valuable in both clinical and educational contexts.
The authors would like to thank the Program for Improvement and Support for Teaching in Higher Education (PAADES-FOA/Unesp, Notice 07/2018) for the support on the author activity G.M.S. in the Anatomy discipline of Araçatuba Dental School.
The authors declare that there are no conflicts of interest.

©2024 Mulinari-Santos, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.