Journal of
eISSN: 2373-4345


Research Article Volume 9 Issue 2
1Department of Restorative Dentistry, S?o Leopoldo Mandic Dental Research Center, Brazil
2Department of Endodontics, S?o Leopoldo Mandic Dental Research Center, Brazil
Correspondence: Simone Kreve, Department of Restorative Dentistry, S?o Leopoldo Mandic Dental Research Center, Rua Independ?ncia 1899, apto 602, Centro, Toledo, Paran
Received: April 11, 2018 | Published: April 25, 2018
Citation: Junior EVDS, Kreve S, Carvalho GAPD. Analysis of linear dimensional change of different materials used for casting dental models: plaster type 4, nanocomposites carbon nanostructures, polyurethane resin and epoxy resin. J Dent Health Oral Disord Ther. 2018;9(2):200-205. DOI: 10.15406/jdhodt.2018.09.00359
This study evaluated the linear dimensional change of two dental plasters (plaster type 4 Elite rock and plaster modified with carbon nanotubes) a PU resin (Novox) and an epoxy resin (Sikadur 32). An aluminum matrix was made to create 20 specimens for each material analyzed. The measurements were performed using SEM with differences expressed in terms of linear dimensional change. Tukey test showed that polyurethane resin had significantly greater shrinkage than plaster type 4 and nanoparticulate plaster. Polyurethane resin shrinkage was also significantly higher than that measured for the epoxy resin, though both were poor at reproducing the original cone measurements. In relation to plaster type 4, nanoparticulate plaster and epoxy resin, polyurethane resin shrinkage was 165%, 101% and 52% higher, respectively. No significant difference was observed between the tested plasters and epoxy resin regarding dimensional changes.
Keywords: calcium sulfate, polymers, models, anatomic, dimensional measurement accuracy, nanotubes, carbon
Prosthetic dentistry is key to restoring function in patients with missing teeth. During the prosthetic process, controlling dimensional changes of the materials used is paramount for treatment success. Therefore, working models should have dimensions as close as possible to those of the teeth. Dental casting is a critical stage in the process of prosthetic rehabilitation.1 The development of materials and techniques that ameliorate both impressions and cast models are therefore essential for clinical success. The fabrication of an accurate casting is dependent on many factors including impression material and technique, accuracy of die material, and waxing and casting procedures.2 Plasters routinely used to make working models include synthetic or natural plaster type 4 and plaster type V.3 Plaster products are widely used in prosthetic dentistry, despite some limitations4 such as5 low fracture resistance, dimensional instability, technical sensitivity and low wear resistance. Authors have claimed that dental plasters are not able to reproduce some details observed in elastomers.6 Many types of materials have been investigated in the last three decades for use as die materials.7 Certain mechanical features of resin-based die materials have focused increased attention upon these substances as potential substitutes for gypsum casts.4,8 Polyurethane resin models have been introduced9 as a viable alternative to stone plasters models and a possible alternative to plaster type IV.10 The need for quality and durable prosthetic work has encouraged the specialty of prosthodontics to research better materials in the process of making high quality aesthetic and functional appliances. This paper presents a comparison between models made from two types of plaster, epoxy resin and a polyurethane resin in terms of linear dimensional change.
The matrix used in this study was made of aluminum 6061-T6 from a prototype developed with the Auto-Cad program. The matrix is composed of three threaded parts that can be screwed onto each other (Figure 1). The base of the matrix has four equidistant metal cones with details carved along its body and apex. The metal cones were divided into 4 numbers identified as 1, 2, 3 and 0 at the base of each cone.
The bottom portion of the base is hinged to the portion that holds the metal cones, which allows unscrewing without tensions being transmitted to the impression materials (Figure 2). The body is screwed to the base to retain the impression material and prevent lateral displacement. It has orifices that allow extravasation of excess material (Figure 3). Four identical molds made up this impression device set, allowing four impressions to be taken, which resulted in 20 specimens (one was replicable) for each researched material. The metal cones were molded using the aforementioned multifunctional matrix. Impressions were taken using addition silicone (Futura - DFL, Rio de Janeiro, Brazil) in a one-stage approach. Once the molding tray was adapted to the base of the matrix, the light impression material was dispensed through an impression syringe to the surface of the matrix to be copied, while the heavy material was accommodated into the tray in increments to avoid over-compressing it and pushing the light material out. The matrix lid was screwed on and the excess impression material flowed through the orifices (Figure 4), resulting in accurate and standardized impressions (Figure 5). Five impressions for each casting material were obtained, which remained at rest for an hour prior to casting. The impressions were filled with plaster modified with carbon nanotubes and plaster type 4 Elite Rock (Zermack, Rome, Italy) mixed mechanically on a vacuum mixer (Elite Mix of Zhermack Technical, Rome, Italy) following the manufacturers' recommendations. The epoxy resin Sikadur 32 (Sika, Santiago, Chile) and polyurethane resin Novox (Mangran, Curitiba, Paraná, Brazil) were also mixed following the manufacturers' instructions. The impressions for plaster casts were filled using a paintbrush (marten fur brushes, number 308-0, Tigre, Joinville, Santa Catarina, Brazil) and mechanical vibration (bench mechanical vibrator for plaster casting / EDG - São Paulo - Brazil). The epoxy resin Sikadur 32 (Sika, Santiago, Chile) was applied using a 20ml disposable luer-type syringe (Injex, Ourinhos, São Paulo, Brazil) without a needle, as it is a material with a relatively thick consistency. Once the casting materials were set, the casts were separated from the impressions and a sum of 20 specimens from each material was analyzed (Figure 6). The samples were divided into the aforementioned groups 0,1, 2 and 3, according to their respective cone, so that each group was made up of 20 specimens, 5 specimens for each material. Group 1 had 5 specimens of die type 4 Elite Rock (Zermack, Rome, Italy), 5 die specimens of carbon nanotubes, 5 specimens of polyurethane resin (Novox, Mangran, Curitiba, Parana, Brazil), and 5 specimens of epoxy resin Sikadur 32 (Sika, Santiago, Chile). The same principle applied to groups 2, 3 and 0. The samples were analyzed in groups on a scanning electron microscope (INSPECT S, Hillsboro, Oregon, USA), at 50 times magnification, which measured the distance between the center of the two lines at the apex of the metal cones (0, 1, 2, 3), which were 2,000 micrometers apart (Figure 7). Prior to SEM measurements, the specimens were sputter coated with gold forming an approximately 10 nm thick layer (Balzers/SCD 004- Sputter Coater, Pfäffikon, Switzerland). Three measurements were taken from random regions between the middle aspect of the two lines located at the apex of each cone. Such measurements were compared to those obtained from the metal matrix (Figure 8) and the differences obtained between them determined the horizontal dimensional stability of the materials analyzed. The absolute dimensional change was calculated as the difference between the measurements obtained from the samples and the actual dimensions measured on the matrix. The relative dimensional change (%) was also calculated. After checking the assumptions of normality and homoscedasticity using the Shapiro-Wilk and Levene tests, respectively, the absolute values of dimensional changes were submitted to one-way analysis of variance (ANOVA). The Tukey test was used for multiple comparisons. Statistical calculations were performed on SPSS 20 (SPSS Inc., Chicago, IL, USA), at a significance level of 5% (α=0.05).
Table 1 presents the descriptive analysis in terms of means and standard deviations of the absolute (mm) and relative (%) values of dimensional change of plasters type 4 and nanoparticulate as well as polyurethane and epoxy resins. Comparing the measures obtained in each tower with those measured in the samples made with each modeling material, intraclass correlation coefficient calculations indicated that: The plasters Type 4 (CCI:0.619) and nanoparticulate (CCI:0.519) demonstrated good reproducibility with respect to the actual measurements. As for the polyurethane (CCI:0.205) and epoxy resins (CCI:0.141), reproducibility was poor. The analysis of variance at one criterion showed that there was a significant difference between the modeling materials regarding dimensional alteration (p<0.001). By Tukey test, it was found that the polyurethane resin showed a significantly higher contraction than that observed when using resinous and nanoparticulate plasters. The contraction of the polyurethane resin was also significantly higher than that measured for the epoxy resin, although both had poor replicability in relation to the measurements of the towers (Table 1) (Figure 9). Shrinkage of the polyurethane resin was significantly higher than that for the epoxy resin. Compared to plaster type 4, nanoparticulate plaster and epoxy resin, shrinkage of polyurethane resin was 165%, 101% and 52% higher (Table 1). Between the tested plasters and epoxy resin, no significant difference in dimensional change was observed. With the aim of quantifying replicability (accuracy) of the measurements made in the samples prepared with different modeling materials in relation to the matrix, intraclass correlation coefficients were used.
The absolute dimensional change was calculated by the difference between the measurements obtained in the samples and the actual dimensions measured in the matrix. The relative dimensional change (%) was also calculated. After the verification of the normality and homoscedasticity assumptions, by the Shapiro-Wilk and Levene tests, respectively, the absolute values of dimensional change were submitted to analysis of variance at one criterion. The Tukey test was used for multiple comparisons. Statistical calculations were performed using the SPSS 20 program (SPSS Inc., Chicago, IL, USA). The significance level was set at 5% (α=0.05). The Levene test indicated that the data presented homogeneity of variance (p=0.08), while the Shapiro-Wilk test also revealed that the data presented a normal distribution (p>0.05). The graphical presentation of the normality of the data can be seen in the histogram below (Figure 10).
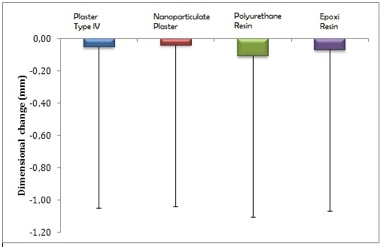
Figure 9 Bar chart of the mean dimensional change values of plasters and resins, in relation to the matrix Legend: Vertical error bars indicate standard deviations; different letters denote significant differences between materials.
Casting material |
Absolute values (mm) |
Relative Values (%) |
Plaster type 4 (batch:165745) |
-0.054 (0.083) A |
-0.027 (0.041) |
Nanoparticulate plaster |
-0.041 (0.066) A |
-0.021 (0.033) |
(Patent: PI0901141 - 2 A2) |
|
|
Polyurethane resin |
-0.109 (0.081) B |
-0.056 (0.042) |
(batch: C-002-8606-001) |
|
|
Epoxy resin |
-0.072 (0.058) A |
-0.036 (0.029) |
(batch: P/A B/6 P/B B/6 U/E 224491) |
|
|
Table 1 Dimensional change in relation to the matrix, in absolute and relative values of plasters and modeling resins
Legend: Standard deviation in brackets. Means followed by different letters indicate a significant difference between materials according to the Tukey test.
Dental plaster has been used for years to cast working models and for laboratory procedures relating to prosthetic dentistry.5 However, there are several disadvantages to its use in the fabrication of casts and dies, for example, poor abrasion resistance potential variability in fine detail reproduction, inadequate tensile strength, and need for a waiting period prior to initiation of laboratory procedures.11 New polymer-based products have been studied as an alternative to plaster. According to Yaman & Brandau2 cost and ease of manipulation are other factors important in guiding selection of a die material. In the current study, impressions for test specimens were taken using addition silicone, due to its excellent dimensional stability,12−16 compatibility with the materials tested and its superiority to reproduce detail.17 According one author, a common deficiency is failure to follow basic principles inherent to the manipulation of impression materials.18 In all studied impression techniques, the addition silicones produced more accurate stone casts than the condensation silicones.15 There is a need for compatibility19 between impression and casting materials for faithful models. There must be no interaction between the materials involved, which is one of the reasons why plaster is widely used. Changes in models obtained from condensation silicone impressions were observed when compared to the master model, which was another reason for avoiding this material. The materials used in this study were handled according to the proportions indicated by the manufacturers aiming at minimizing distortions. Adequate manipulation of the material is directly related to its dimensional stability and maintenance of its mechanical properties, e.g. the ideal water/plaster powder ratio is crucial for the performance of the material,20,21 just as the base/activator ratio of casting resin materials is also essential to maintain stability of the product.22 Since wet casts usually have inadequate strength and surface hardness, dentists normally must wait for 24–48 h before manipulating gypsum casts.23 The aforementioned ratio guidelines were followed,24 though a recent study25 observed the influence of the variation of water/powder on the compression resistance of plaster type 4 and synthetic models and observed that an increase in water by 20% caused no significant difference in the compressive strength of the material. Polyurethane resin (NOVOX, Mangran, Curitiba, and Paraná, Brazil) was presented as a material easy to handle and to homogenize its components. The product resulting from mixing the components is a very fluid liquid, when poured into the mold, flowed throughout the surface of the vinyl polysiloxane, including small details. It copied the surface requiring no mechanical vibration for casting due to the high flowability of the material. Epoxy resin Sikadur 32 (Sika, Santiago, Chile) is viscous and thick, making the pouring process much more complex, which required the aid of a disposable 20mL Luer syringe (Injex Ourinhos, São Paulo Brazil) without a needle. Cast resistance is directly affected by two factors, water/powder ratio and mixing time.25 The current study used a vacuum mechanical mixer (Elite Mix of Zhermack Technical Rome, Italy) considering that mechanized manipulation promoted a more homogenous mixture. According to the specifications of the ADA26 on evaluating dimensional changes of materials used in dental model casting, the most widely used method is the measurement of the space between two lines contained in the master model. This method was adopted in the present study, also following several authors27,28 who measured the distance between two grooves at the apex of the functional matrix cones, which were 2.000μm apart on the original matrix. The materials used to make dental models must be dimensionally accurate, reproduce details adequately, be resistant to abrasion, have surface hardness, be efficient and easy to handle, be compatible with the impression material, be non-toxic and present adequate transverse resistance.29 The authors reiterated that dimensional accuracy is a fundamental property, as it directly influences accuracy, frictional retention and marginal adaptation of the prosthetic work. Plaster is the material of choice because of its low cost and ease-to-handle characteristics,28 most plasters, however, show distortions30 and some other limitations such as low fracture resistance and low abrasion resistance as well as low reproduction of details.3,31 Stone has limited transverse strength, and this may predispose working casts to fracture when they are removed from impressions.29 In order to produce designs with improved properties, such as accuracy and durability, studies have shown the possibility of using resin materials for casting dental models.3,13, 15, 23, 26,28−39
In this study, one-way ANOVA demonstrated a significant difference between casting material and dimensional change (p<0.001). The Tukey test revealed significantly greater shrinkage of the polyurethane resin when compared to plaster type IV and nanoparticulate plaster. Such shrinkage has been observed in most studies that analyzed the dimensional behavior of resinous materials, due to the inherent polymerization shrinkage of polymers.23,27,32,31,38
One study3 evaluated the dimensional accuracy of seven materials for making dies and reported that polyurethane resin underwent a combination of expansion and shrinkage, where resin-impregnated type IV plaster was the most accurate. Conversely,37 dimensional stability has been demonstrated to be higher in silica reinforced polyurethane resin than in two synthetic type IV and type V plasters. In this study, no significant difference in dimensional behavior was observed when analyzing epoxy resin and the two plasters tested, which has also been reported elsewhere13 when gypsum and epoxy resin die materials provided a similar degree of dimensional accuracy in reproducing a complete arch when used with addition silicone impression materials.
Based on the data obtained from this study, the plasters evaluated were superior to polyurethane and epoxy resins in reproducing the actual measurements of the original matrix, with polyurethane resin showing the greatest polymerization shrinkage when compared to the other materials tested.
None.
The author declared that there is no conflict of interest.

©2018 Junior, et al. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.