Journal of
eISSN: 2373-4345


Increasing success with endosseous implants in edentulous patients has heightened the interest in using fixed prostheses in this patient population. Despite this trend, upper lip support has been a long-standing challenge, especially in patients with a thin elongated upper lip, termed “senile”, where the presence or absence of a flange compromises the esthetic and functional outcomes. Although, the conventional solution to reestablish elevation and support of the upper lip has been an anterior flange of a removable prosthesis, fixed implant supported prostheses do not incorporate a flange for reasons of hygiene and maintenance. In this case report a patient with atrophic maxillary edentulism and upper lip senility that sought fixed rehabilitation was identified. Following pre-surgical assessment of vertical facial proportions, lip length and morphology, and inter-arch space, a surgical upper lip length reduction was performed using the Subnasal Lip Lift (SNLL) technique. 6 months after the SNLL, when the lip length stabilized, the patient received fixed implant supported monolithic zirconia prosthesis without an anterior flange. The desired amount of lip elevation and tooth display in the final prosthesis was achieved. The lip length remained stable at the 1-year follow-up, Subnasal scars were not evident by 2 months, abnormal lip dynamics were not observed, and improved vermillion eversion was present.
Keywords: lip support, fixed implant supported prostheses, lip lift, esthetic facial surgery
Patients with acquired maxillary edentulism and atrophy often present with facial soft tissue changes that limit the restorative dentist’s ability to fabricate a functional and esthetic prosthesis. Often with age, the upper lip becomes thin and elongated, due to atrophy of muscles, fat, and connective tissue1 and is termed “senile”. Interestedly, the age-related changes of lip do not result in a loss of lip volume, rather the volume is redistributed to increased length resulting in vermillion inversion and ptosis of the lip2 One of the negative consequences of the senile lip regards an unpredictable display of oral spaces, such as the buccal corridor and smile line,3 with the maxillary incisal display at rest being decreased or eliminated.4 These changes, compounded with atrophy of the underlying maxillary skeleton and tooth loss, result in significant labio-facial changes.5 The conventional prosthetic approach to provide lip support to this patient population is with a denture flange to reestablish lip support and elevation.6 However, denture flange support occurs by extension of the prosthesis into the vestibule and pushing the lip outward7,8 which alters muscle pull and subsequent tissue movement. This artificial support pushes the orbicularis oris outward uniformly and allows the superior anterior border of the flange to develop an unaesthetic Subnasal convexity. The lifting effect of the flange also seems inadequate in correcting an inverted vermillion border and does not restore convexity to the philtrum columns. Although flanges provide support to a senile lip, they cannot be employed with fixed restorations for reasons of maintenance and hygiene. Additionally, the amount and thickness of material required may limit biomechanical function.9,10 However, many patients desire fixed implant retained prosthetic solutions but lack adequate soft tissue support without a flange. Calvani evaluated lip support of 412 patients with differing prostheses and thin lips and determined 66% of full-arch implant supported fixed restorations presented with a horizontal groove in the upper lip.11 This groove, termed a “split philtrum line”, can develop with a fixed implant supported prosthetics when there is inadequate support inferior to the nasal base.
Nonetheless, surgical augmentation of the senile upper lip can facilitate the restoring dentist’s ability to provide an esthetic, fixed maxillary prosthesis for the edentulous maxilla minimizing the unwanted effects of atrophy, tissue thinning, and loss of support. Known as a Subnasal Lip Lift (SNLL), it effectively shortens the lip while simultaneously increasing the vermillion display by eversion (Figure 1). While the literature supports that the SNLL procedure has predictable esthetic outcomes to improve age-related changes to the upper lip with intact muscular function, the technique has also been refined in the past decades to diminish scar formation, with meticulous closure, laser resurfacing, or dermabrasion.5,9,12-16 This technique was employed in this case report to demonstrate the application of surgical management of maxillary edentulism accompanying a senile upper lip that was restored with a flangeless fixed implant-supported maxillary prosthesis. The purpose was to elevate the upper lip to an ideal position and philtrum contours for esthetic tooth display and lip support, thereby reducing the need for an anterior flange.
A 78 year-old female presented to the University of Alabama at Birmingham School of Dentistry seeking care. She expressed dissatisfaction with the function and esthetics of her existing maxillary prosthesis and sought rehabilitation with fixed implant supported restorations. Clinical evaluation revealed maxillary edentulism with moderate atrophy, a senile upper lip with lack of vermillion display and an unnatural convexity caused by her existing removable prosthesis due to the attempt to create an ideal maxillary tooth display (Figure 2). Vertical facial proportions, lip length/morphology and vestibular depth were assessed. Lip length was measured in repose from the Subnasal to the stomion superius and was found 25mm (Figure 3). These findings indicated that patient’s desire for maxillary fixed implant supported prosthesis could not be achieved only with prosthetic treatment. Thus, an interdisciplinary treatment plan was developed to reestablish a natural lip support with a combination of prosthetic tooth support and a SNLL procedure. Prosthodontic evaluation included a trial diagnostic tooth set-up without a flange to judge lip support provided by the prosthetic teeth alone and measure the available restorative space.17,18 The lip contours were visualized without the flange to determine a realistic pre-surgical assessment of the need for additional lip support.19,20 The teeth were set up to ideal dimensions for a fixed implant supported prosthesis, with approximately 10mm interach space.18,21 This set-up was also utilized as a reference to evaluate the desired amount of lip reduction. In final planning with the surgeon and prosthodontist, an 8 implant-supported screw retained monolithic Zirconia restorationwas selected.

Figure 2 Senile lip without denture flange support noting excessing length, flattening of contours, and vermillion inversion (A). Senile lip with a well-constructed denture flange (B, C and D) which uniformly pushes out the lip with loss of philtrum columns, unnatural fullness, inversion of the vermillion, and a subnasal convexity.
The subnasal lip lift procedure (SNLL)
The planned lip excision was marked with the patient in the upright position for accurate lip length assessment and prior to administering local anesthesia to avoid tissue distortion (Figure 4). A bullhorn-type incision in the Subnasal region was designed. The superior incision line approximates the naso-labial junction, and extends around the ala-facial groove. The inferior incision line mirrors the pattern superior excision with a separation of the excisions at the desired level of lip lift. The incision is made with a #15 blade and carried into the subcutaneous plane. The underlying orbicularis oris muscle was not excised because of the potential for irregular lip dynamics, however, some advocate muscle excision proposing it offers greater stability of the lift with less relapse.5,22 Closure was achieved with meticulous interrupted 4-0 Vicryl subcutaneous sutures (Ethicon, Somerville, NJ) and 5-0 nylon skin sutures taking care to avert the wound edges (Figure 5). The wound was treated with topical antibiotic ointment, applied daily for 1 week, and the nylon sutures were removed in 7 days. Sunblock was recommended for six months to avoid any potential for hyper pigmentation. On the same day of the SNLL 8 dental implants were placed utilizing a surgical guide fabricated from the trial teeth set-up (Figure 6). Delayed engagement of the implants was applied due to inadequate primary stability and a tissue-borne interim denture was inserted one week after SNLL. The anterior flange was reduced as much as possible to accommodate the lip elevation and minimize excessive anterior tooth display. It is important to inform the patient that the ideal dimensions and esthetics of this provisional prosthesis may not be feasible during the healing phase. However, if the initial implant stability permits, the denture prosthesis may be immediately converted to a flangeless screw-retained fixed provisional restoration, which will allow for more optimal esthetics.
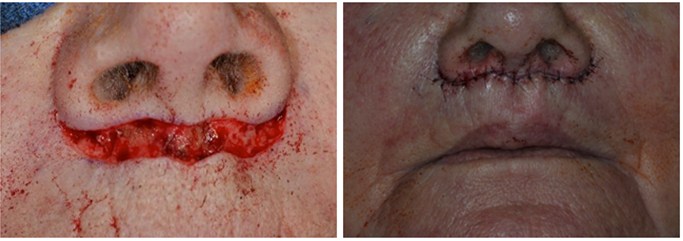
Figure 5 A Surgical excision of superficial layers without encroachment into the underlying muscle tissue. B. Post-surgical final closure prior to anticipated partial relapse.

Figure 6 Surgical guide dublicated from the diagnostic teeth set-up and placemant of 8 dental Implants.
After approximately six months of healing following the implant placement and the SNLL, an implant supported fixed provisional restoration was fabricated to reassess tooth position, lip support, and to serve as a guide for the final implant supported prosthesis. The delay is not only for adequate osseointegration, but to allow for the anticipated partial relapse of the SNLL prior to stabilization of the lift length.22 The patient had a preoperative lip length of 25 mm and underwent an 8 mm Subnasal tissue resection resulting in a 19 mm immediately post-operative. At 6-months lip length was found to be 21 mm lip (Figure 7). These measurements were stable at 1-year follow-up, while the Subnasal scar was inconspicuous by 2 months. For the definitive prosthesis a screw-retained monolithic Zirconia restoration was fabricated; while the prosthesis replaced teeth and tissue, there was no extension into anterior vestibule. The final outcomes demonstrated an increase in vermillion show and elimination of a Subnasal bulge for the upper lip. Satisfactory lip support was accomplished with the combination of the SNLL and the fixed implant-supported restoration. Philtrum columns and an age-appropriate vermillion display were achieved, (Figure 8). At the one-year follow up patient expressed high satisfaction with the esthetic results of her treatment, as well as improved function of her implant-supported prosthesis.
Inadequate lip support may result from reasons other than maxillary atrophy with a senile lip, and a comprehensive oral and facial evaluation should be performed to determine if soft tissue surgical procedures, such as a SNLL, are appropriate rather than procedures involving hard tissues. To determine the etiology, an assessment should include the facial height, facial profile, lip thickness and lip length.10 The assessment is done with and without patients existing dentures in place, if available, evaluating both the vertical facial proportions of the upper lip, lower lip, and chin as well as the contribution of the vertical dimension of occlusion. Documentation of upper lip length, depth of the vestibule, and height of the anterior maxillary ridge is important to aid interdisciplinary planning for SNLL treatment. The fullness of the upper lip is assessed by a measure of the nasiolabial angle (normal range 85°-105°) or from measures against normal diagnostic lines, such as Burstone’s, Steiner’s, or Ricket’s lines.23 Factors such as lip thickness, morphology of the nasal base, and presence of facial hair effects the perception of support and is challenged with the senile lip. The normal upper lip length at rest is estimated to range from 18-22 mm.23,24 However, rather than endorsing a set numeric range to guide the need for surgical correction, greater emphasis should be placed on proportional values to account for individual and ethnic variance. The vermilion follows proportions by division into thirds with the upper lip being 1/3 and the lower lip being 2/3 of total vermilion height.22,26,27 These proportions believed to be relatively consistent in classical measures of attractiveness.
Perenack noted the relative contraindications to an SNLL are a short lip length, less than 18 mm, or a history of forming hypertrophic scars and keloids, otherwise excellent outcomes could be routinely obtained. 5 If the lip length is found to be approximately 18 mm or less, the lip may be well supported by the prosthetic teeth alone since their position and angulation are the major supporting features of the inferior portion of the upper lip. The changes in lip length associated with orthagnathic surgery are also well established whereas conventional bone grafting of the atrophic maxilla may provide only minimal success in supporting the senile lip largely due to the extent of grafting necessary and does not address the lip length or morphology.27-29 Evaluation of the apical position of the upper lip during maximum smile is also critical. Lip function that provides less gingival display was often deemed more esthetic, and a low lip line is advantageous for the fixed anterior prostheses, since the tissue-prosthesis junction can be visible in high smile patients.30,31
The described Subnasal lip lift (SNLL) offered a predictable and esthetic improvement of age-related upper lip changes, and allowed for a functionally successful restoration with fixed implant-support prosthetics. Esthetic and functional outcomes were enhanced by normalizing upper lip length, increasing vermilion show, increasing tooth display, eliminating a Subnasal convexity, and reduction of restorative material. Additional factors of expense, multiple staged procedures, and overall treatment time must be considered. Overall, the Subnasal lip lift provided a highly satisfactory treatment outcome. Preservation of muscular function and avoidance of an underlying flange are key elements of this treatment modality.
None.
None.
Author declares that there is no conflict of interest.

© . This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.