Journal of
eISSN: 2373-4396


Research Article Volume 1 Issue 1
1American Society of Hypertension, USA
2Royal Society for Promotion of Health, UK
Correspondence: Aurelio Leone, Fellow of the American Society of Hypertension (USA) and Royal Society for Promotion of Health (UK), Via Provinciale 27, 19030 Castelnuovo Magra (SP), Italy, Tel 390187676346
Received: April 08, 2014 | Published: May 7, 2014
Citation: Leone A. What has taught almost half a century of research on the relationship between passive smoking and cardiovascular system? J Cardiol Curr Res. 2014;1(1):18-23. DOI: 10.15406/jccr.2014.01.00004
Almost half a century of research on the relationship between exposure to secondhand smoke and damage of the cardiovascular system has achieved some key findings. Cigarette smoking, in both its active and passive exposure, is a toxicosis and, therefore, should be considered as a systemic disease with marked cardiovascular impairment. The cardiovascular damage is well defined and consists of a whole series of functional and pathological manifestation prevailingly to the myocardium, vascular endothelium, and artery vessels showing a progression of atherosclerotic lesions of the coronary arteries, aorta, carotid and cerebral circulation. The efforts are to eliminate or reduce the extent of the damage with the development of techniques deputed to control the absorption of toxic products of smoke, such as nicotine, carbon monoxide and carcinogens, and save the environment, although a great failure together with the anti-smoking campaigns has been observed. Therefore, the future of the exposed individuals looks like a very difficult solution on the possibility of limiting the cardiovascular damage by tobacco smoke, unless smoking is absolutely banned.
Keywords: passive, smoking, cardiovascular, damage, patents, electronic cigarette, smoking toxics
Nowadays, two statements can be supported with certainty about the role of passive smoking with regard to the cardiovascular system. The first relates to a detailed definition of cigarette smoking as a factor of damage,1 and the second identifying specific structures of the heart and blood vessels considered as a target organ of toxic constituents of tobacco.2–5 Smoking1 is currently defined as a chemical toxicosis, which is able to cause detrimental effects either of acute or chronic type of different structures of the body like cardiovascular system, respiratory system and epithelial glands. With regards to cardiovascular structures involved in the damage from smoking, both the heart muscle and vascular system are simultaneously compromised, although by different stages and severity.2–9 It is also well documented that whatever is the approach to the study of the damage caused by passive smoking on the cardiovascular system-and there are several types of approaches: clinical, pathological, metabolic, toxicological, statistics and many others,8 the end result consists of an irreversible anatomical damage of those structures characterized by an adversely marked tropism towards smoking compounds. The type of cardiovascular damage has been variously described and, above all, interpreted as due to a different setting of research that has led to mixed results not always similar with regard to the type of studies. This review analyzes in detail only the main observations whose results may provide well-definite updates on the effects of passive smoking with regards to cardiovascular system, omitting to comment on those aspects which are still under discussion.
What is passive smoking?
Passive smoking, secondhand smoking, involuntary smoking and environmental tobacco smoke (ETS) are terms, which all indicate the exposure of a non-smoker and smoker to the combustion products of cigarette released into the environment. Exposure to passive smoking is currently defined as either an exposure to side stream smoking of burning cigarettes or to mainstream smoke. Both side stream smoke and mainstream smoke contain the largest number of toxic substances able to damage the cardiovascular system. Evidence indicates that three main phases characterize passive smoking exposure as Table 1 shows.
Phases |
Chemical pollutants |
Affected individuals |
Side stream smoke |
Gaseous nicotine |
Active smokers together with Livings |
Carbon monoxide |
Polluted environment |
|
Main stream smoke |
Carbon monoxide |
|
Nicotine in particles |
||
Vapor phase |
Carbon monoxide |
Environment and its Livings |
Gaseous and particulate nicotine |
||
Thiocyanate and Aromatic Amines |
||
Table 1 The main phases of passive smoking and its pollutants
In more detail, the three phases that characterize passive smoking have been well identified as follows. Specifically, the side stream smoke is defined as the smoke that drifts from the end of the lit cigarette; mainstream smoke is inhaled directly through the burning cigarette by the smokers, while the exhaled mainstream smoke is the smoke breathed out from the lungs. In addition, the composition of mainstream and exhaled mainstream smoke can likely differ since some of compounds retained by smokers or otherwise, altered by the process of combustion and then exhaled, may act differently. Indeed, these factors adversely influence passive smoking characteristics. The particles of side stream smoke are smaller than those that mainstream smoke has. Therefore, side stream smoke is more deeply inhaled into the lungs.10 The vapor phase contains all the gaseous compounds of cigarette smoke that pollutes the environment and is also able to spread out. Therefore, the main differences in secondhand smoke phases may be related to the duration and time of production, level of toxins in the environment and possible re-suspension of deposit particles that are able to react with other environmental toxics. These characteristics indicate that toxic compounds of cigarette smoke may potentiate their concentrations in the environment and strongly damage living individuals. Chemical compounds of tobacco smoke in the environment are a strong polluting factor, but not the strongest.
ETS is probably the main and unnecessary pollutant of indoor air in different places such as workplace, public buildings, offices and home. The harm of the cardiovascular system is the result of either an isolated or combined action of primarily some active pollutants derived from burning tobacco, which contains over 4,000 toxic chemicals.11 The large majority of these pollutants have carcinogenic and adverse effects on the heart and blood vessels in both humans and animals. However, it is now well established that three substances (Table 2) such as nicotine and its metabolites, carbon monoxide and thiocyanates, play deleterious effects for the cardiovascular system. The repeated, although irregular, action of these compounds is initially responsible for a transient, cardiovascular damage, which in time develops irreversible changes. In addition, a currently newer acquisition of the characteristics of passive smoking is to be related to the state of tobacco leaves. According to the degree of manufacturing, nicotine and its metabolites as well as thiocyanate have the same level of toxicity in either fresh or cured tobacco leaf, while carbon monoxide concentrations depend strictly on the amount of burning tobacco of the cigarette. Indeed, a strong influence in enhancing toxic residuum of passive smoking is due to the paper rolling up the cigarettes, which releases toxic chemicals as a result of its burning.12 Therefore, the number of burning cigarettes exhaling their toxics into the environment is a fundamental factor of atmosphere pollution.
Compound |
Place of production |
Nicotine and its metabolites |
Fresh tobacco leaf |
Burning cigarette |
|
Carbon monoxide |
Burning cigarette |
Thiocyanates |
Burning cigarette |
Fresh tobacco leaf |
Table 2 The main compounds of ETS damaging cardiovascular system
The characteristics of the environment are also a definite factor in identifying the harm of passive smoking for the cardiovascular system.13–15 It is worth noting that poor ventilated and limited spaces represent places where passive smoking strongly exerts its adverse effects. There is overwhelming evidence that individuals living in confined spaces meet cardiovascular, respiratory and metabolic alterations with significantly higher rates after chronic exposure to passive smoking.16,17 In addition, ETS chemicals might aggregate other air pollutants, all together potentiating the damaging power. Open spaces usually spread out the pollutants of passive smoking in a large part of the atmosphere and, in this way, the risk of poisoning are reduced if compared to that determined by active smoking. Similarly, lifestyle of non-smokers is strongly influenced by the presence and number of active smokers.17 Therefore, such a condition should be avoided since lifestyle is one of the major modifiable factors to fight the appearance of adverse events. Only in the presence of promiscuity and unhealthy spaces the power of cardiovascular damage due to passive smoking exposure is heavily enhanced.
Properties of main chemical compounds of passive smoking
It has been established that three main chemicals of tobacco smoke exposure play, among others, a damaging role in the cardiovascular system,18 although the data also attribute harmful effects to some aromatic amines.19 However, the adverse effects of nicotine, carbon monoxide and thiocyanates for cardiovascular system cannot be absolutely denied. In addition, evidence indicates that physically the spatial structure of the chemical chains of tobacco compounds strongly influences the deleterious effects.20
The main effects of nicotine, carbon monoxide and thiocyanate for the cardiovascular system are listed in Table 3. These effects have been demonstrated to be associated with different types of damage caused by ETS exposure of both heart and blood vessels.21,22 In addition, the cardiovascular damage is the result of a direct or mediated action of these chemical compounds by an isolated or combined pathological mechanism.
Chemical compound |
Effects |
Nicotine |
Sympathetic System Stimulation |
Adrenal medulla stimulation |
|
Nerve Ending Stimulation |
|
Catecholamine release |
|
Increased Heart Rate |
|
Increased Blood Pressure |
|
Increased Demand in Oxygen |
|
Carbon Monoxide |
Increased Carboxyhemoglobin |
Hypoxia |
|
Cellular Damage |
|
Thiocyanate |
Cellular damage |
Increase in Nicotine Effects |
|
Increased Carbon Monoxide Effect |
Table 3 Main adverse effects of ETS compounds on the cardiovascular system
The cardiovascular changes produced by the exposure initially consist of reversible functional alterations, which become in time pathological lesions, some of these specifically related to carbon monoxide.23,24 Very recent observations on the chemical chains of smoking compounds require a brief discussion. It is known that the spatial arrangement of molecular chains recognizes, for what concerns its physical and chemical properties, 2 topics such as open molecular chains with reactive sites most active, and closed-chain molecules chemically characterized by a greater stability. Indeed, all the three main smoking compounds nicotine, carbon monoxide and thiocyanates, have open chains with chemical sites strongly reactive and able to give more than a single reaction with the atoms of the environment. This fact makes ETS able to react with several chemicals producing a larger variety of chemical substances, sometimes more toxic than the original compounds.
The latter occurrence, although not definitely proven, explains differing degrees of damage that can be observed as an adverse effect of passive smoking for the cardiovascular system. These observations allow the conclusion that the chemicals in the secondhand smoke may play a direct action that is similar to that of the active smoke even if the latter has toxic concentrations higher to producing cardiovascular damage. In addition, an indirect action, more specifically linked to the chemical reaction with other toxic molecules of the environment, may considerably increase cardiovascular damage with a little possibility of prediction.
Cardiovascular damage
The damage caused by ETS exposure recognizes two main mechanisms: initially reversible functional and late stable pathological alterations. These two types can co-exist in some phases of the exposure. Passive smokers, similarly to what observed in active smokers25 have been shown to be bearers of atherosclerotic plaque and increased artery wall thickness with the highest rate. However, these structural changes are largely preceded by functional reversible alterations, primarily consisting of endothelial dysfunction and impaired cardiac performance during exercise in healthy and diseased individuals.3,26–31 Generally, five types of cardiovascular damage are the result of an acute or chronic exposure to passive smoking as listed in the Table 4. Functional damage usually follows an acute exposure, which recognizes different characteristics. Indeed, isolated or repeated exposure may occur, although, usually, not prolonged in time. In addition, the damage is often transient followed by baseline parameter restoration. The main functional alterations documented consist of transient endothelial dysfunction, impaired cardiac performance, changes in systolic blood pressure and heart rate, and increased carboxyhemoglobin concentrations in both healthy individuals and individuals suffering from cardiovascular disorders.3,16,26–31 These functional alterations, usually transient, may trigger the mechanism of the anatomical lesions in the time.
Damage |
Characteristics |
Type of exposure |
Functional |
Functional changes |
Acute and chronic exposure |
Clinical |
Symptoms of CV disease |
Chronic exposure |
Anatomical |
Structural CV alterations |
Chronic exposure |
Associated |
All types of alterations |
Acute and chronic exposure |
Experimental |
Functional and structural |
Acute and chronic exposure |
Table 4 Cardiovascular damage caused by ETS exposure
CV, Cardiovascular
Endothelial dysfunction is one of the most important parameters adversely influenced by the exposure to ETS.27 The endothelium is intimately linked to control vasomotor tone and prevent the atherosclerotic plaque formation because of its shape and released chemicals.32 Endothelial dysfunction following acute exposure is usually transient and, therefore, unable to cause initially irreversible morphological alterations. However, evidence indicates that the mechanisms of structural damage of the cardiovascular system are triggered at the same time of the ETS exposure. Thus, evidence indicates that endothelial dysfunction is the main key of activating atherosclerotic process.33 Several smoking compounds, primarily nicotine, adversely influence the function of endothelial cells by inducing a dysfunction of different type and degree with earlier appearance than that due to other major cardiovascular risk factors such as hypertension, increased LDL-Cholesterol concentrations, altered glucose metabolism and obesity. Usually, the latter factors chronically damage the endothelium.34–36 Since the endothelial dysfunction has been considered to be an early event in the pathogenesis of atherosclerotic plaque formation, studies have been conducted in both humans and animals to clarify the role of ETS exposure. Apart from the findings of Giannini31 and Celermajer et al.,28 there is overwhelming evidence that increased aortic stiffness in men, part of whom suffering from ischemic heart disease, is an effect of ETS exposure as Stefanidis et al.,37 experimentally documented. In addition, animals like cockerels and rabbits exposed to ETS showed heavily impaired endothelial function and accelerated atherosclerosis progression.29,38 These observations indicate with no doubt that endothelial dysfunction is an early and severe manifestation of ETS exposure.
Functional changes of cardiac performance to the exercise during ETS exposure provided definite answers on the degree and severity of cardiovascular damage in both healthy individuals and individuals suffering from ischemic heart disease3,26,39–41 as an effect of both carbon monoxide and nicotine. However performed, the exercise stress testing either on a bicycle ergo meter or treadmill showed impaired performance primarily of some parameters such as duration and power of exercise and prolonged time to recovery to baseline parameters in both healthy individuals and individuals with coronary heart disease, although with different degree from the two groups. Indeed, similarly to what demonstrated for the endothelial dysfunction, documented disorders to the exercise were initially transient and characterized by reproducibility.42
Increased systolic blood pressure and heart rate, which occur transiently during acute exposure to passive smoking and are also of short duration after exposure, are related to sympathetic nervous system stimulation, increased catecholamine release and endothelial dysfunction.43–45 Clinical and anatomical damage are the result of chronic exposure to secondhand smoke and, have many contacts since when irreversible structural changes in the cardiovascular system are manifest usually they are associated with clinical symptoms. Anatomical damage shows clearly identified characteristics that are the result of chronic effects of passive smoking. There is no doubt that several factors influence the morphology of the anatomical damage affecting the heart and blood vessels. These factors include primarily the duration of exposure and characteristics of the environment where exposed individuals are living. The types of anatomical damage due to passive smoking exposure are listed in Table 5.
CV damage |
Main references |
Myocardial infarction |
2,8,21 |
Coronary atherosclerosis |
16 |
Systemic artery atherosclerosis |
16 |
Increased aortic stiffness |
16,37 |
Peripheral artery disease |
25 |
Endothelial cell changes |
21,23 |
Cerebrovascular alterations |
8 |
Experimental myocardial alterations (experimental myocarditis) |
24,51 |
Table 5 Anatomical damage of cardiovascular system following chronic exposure to passive smoking
Among the most serious diseases, there is evidence that myocardial infarction2 may be identified as a consequence of chronic and repeated exposure to passive smoking. In addition, endothelial alterations associated with an evident increase of aortic stiffness and atherosclerosis progression are common observations in individuals exposed to passive smoking.27,37,46,47 Pathological lesions consist of typical structural changes which characterize the underlying disease. As mentioned, clinical symptoms often accompany the presence of the pathological alterations with a major incidence of those signs related to stable angina. It is worth noting that the morphological lesion due to experimental pathology shows the typical feature known as experimental myocarditis.
Experimental myocarditis or cardiomyopathy has been described as a result of a direct effect of carbon monoxide on the myocardium. The structural features consist of focal areas of necrosis specifically located in the sub-endocardium, perivascular infiltrates and typical punctuate hemorrhage.48-50 Cardiac involvement may appear early after exposure or more frequently, as a late manifestation. Rabbits,24,29 cockerels and guinea pigs51,52 showed experimentally more pronounced alterations related to experimental cardiomyopathy in both myocardial and artery vessels. The structural alterations determine changes of intracellular respiratory chains because of a reduction in oxidation-reduction processes with intracellular accumulation of toxins impairing cellular function and changes of myocardial shape because of remodeling mechanisms.53
In summary, evidence clearly indicates that both experimental findings and clinical trials show typical, but different alterations of the cardiovascular system that involve artery vessels at various levels and myocardium with final results depending on the characteristics of the exposure, duration and environment. Therefore, discussed data clearly identify cardiovascular damage from tobacco smoke as a damage characterized by polymorphism, even if the different aspects progressively converge each to other to worsening the final result of the alterations observed on the heart and blood vessels.
Electronic cigarette (E-Cigarette)
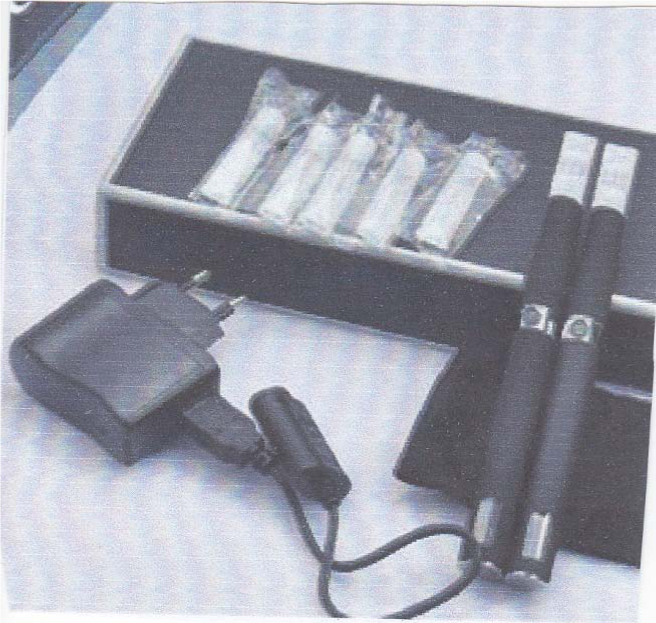
A brief comment needs the introduction of electronic cigarette with the purpose of helping smoking cessation. The electronic cigarette, also known as an e-cigarette, vaporizer or PV, is based on the principle of a device to aerosol where a liquid mixture of different composition, but not nicotine, is vaporized and inhaled, simulating both the attitude and characteristics of smoking. The mixture contains three essential components (Table 6) such as a solution of propylene glycol liquid added to aromatic flavors for producing vapor included in a small plastic container with opening on each end to bring on the mouth, an atomizer containing a small amount of the heating coil and little filament with a wick, and an energizer battery (Figure 1).
Component |
Function |
Cartridge |
Container with a mixture of propylene glycol |
Atomizer |
Heating coil and filaments with a wick |
Battery |
Lithium-ion rechargeable battery |
Table 6 Components of an electronic cigarette
Of this device supporting the idea of “smokeless non-tobacco cigarette”, there is still no evidence whether it causes or not damage to the health of the users and also helps the real capacity of smoking cessation. Therefore, a question arises: what is the link between the electronic cigarette and exposure to second-hand smoke? Undoubtedly, there is still no demonstrable link, but, as some authors argue,54,55 this device reduces significantly the number of smokers. A significant reduction in the concentrations of smoke in the environment could be obtained by using the e-cigarette and then, a decrease of cardiovascular damage hypothetically observed.
Evidence indicates that a careful assessment of the cardiovascular effects of passive smoking exposure requires a correct measure of gas concentrations in the environmental air. An individual living in both outdoor and indoor environments usually breathes from three to 9 liters of air/min to introduce the oxygen necessary to respiratory functions of both systemic and cellular structures.56 The presence of pollutants in the air, however produced, including also the toxics of tobacco, shifts adversely the oxygen balance with adverse respiratory effects on aerobic metabolism and such a condition makes exposed individuals vulnerable to the effects of passive smoking. Therefore, preventive measures to warrant clean air in the environment require also devices contributing to that57 as an e-cigarette could be. In addition, there is evidence that long-term-exposure to air pollutants was associated with increased blood pressure and hypertension particularly in men.58 another issue worthy of mention for better understanding the damage caused by the exposure to second-hand smoke is the manufacture of tobacco leaves. It is clear that lower concentrations of toxics in the cigarettes may reduce, but not completely remove the extent of damage. In this direction, the tobacco manufacturing industries have sought to develop protective patents.59–61 It is evident that discouraging results have been obtained so far from all used method of containing the extent of cardiovascular damage caused by exposure to passive smoking.
As described, there is always more evidence that smoking is a chemical toxicosis1 to be assigned, in my personal opinion, to the group of systemic disease, even if some target organs as cardiovascular, respiratory system and epithelial structures undoubtedly exist. Moreover, smoking causes physical addiction primarily because of the nicotine that opposes the attempts of smoking cessation. Cardiovascular damage due to exposure to second-hand smoke is now well identified and experimentally reproducible requiring a significant effort by the health officials to prevent it. There is evidence that the adverse effects related to passive smoking exposure are far from being solved. Therefore, an unpromising future will affect all those individuals exposed, against their will, to the harmful effects of passive smoking and, consequently, all the forces in the field of health, policy and the socioeconomic structures should defeat the contemporary plague of cigarette smoking in all its forms. Indeed, the harm caused by smoking is demonstrated by studies either clinically or related experimentally in exposed animals.62–65
These considerations emphasize the fact that exposure to passive smoking is strongly deleterious for both involuntary and active smokers because of an interaction of different factors that adversely influence cardiovascular system. In addition, the type and degree of cardiovascular damage in exposed individuals are, nowadays, undoubtedly recognized.
None.
Authors declare that there is no conflict of interest.

©2014 Leone. This is an open access article distributed under the terms of the, which permits unrestricted use, distribution, and build upon your work non-commercially.